Podcast
Questions and Answers
What is the primary consequence of ATP depletion on cellular sodium and potassium levels?
What is the primary consequence of ATP depletion on cellular sodium and potassium levels?
- Increased sodium efflux and decreased potassium influx
- Decreased sodium and potassium levels in the cytoplasm
- Decreased intracellular sodium and increased potassium efflux
- Increased intracellular sodium and decreased extracellular potassium (correct)
What is a main consequence of reduced Na/K pump activity in cells?
What is a main consequence of reduced Na/K pump activity in cells?
- Increased uptake of glucose
- Decreased calcium influx
- Enhanced protein synthesis
- Altered membrane potential (correct)
Which pathway predominantly produces ATP under aerobic conditions?
Which pathway predominantly produces ATP under aerobic conditions?
- Conversion of fats to energy
- Anaerobic glycolysis
- Fermentation of glucose
- Oxidative phosphorylation (correct)
Which of the following is a direct effect of glycolysis during ischemia?
Which of the following is a direct effect of glycolysis during ischemia?
What effect does lactic acid accumulation have on cellular enzyme activity during ATP depletion?
What effect does lactic acid accumulation have on cellular enzyme activity during ATP depletion?
What primarily triggers the unfolded protein response in cells?
What primarily triggers the unfolded protein response in cells?
What is a direct result of the failure of the Ca2+ pump in a cell with depleted ATP?
What is a direct result of the failure of the Ca2+ pump in a cell with depleted ATP?
Which factors are known to cause mitochondrial damage?
Which factors are known to cause mitochondrial damage?
What is one of the roles of ATP in the cell's synthetic processes?
What is one of the roles of ATP in the cell's synthetic processes?
What is a consequence of ribosome detachment from the endoplasmic reticulum?
What is a consequence of ribosome detachment from the endoplasmic reticulum?
What triggers the irreversible phase of mitochondrial permeability transition?
What triggers the irreversible phase of mitochondrial permeability transition?
Which of the following enzymes is NOT activated by increased cytosolic calcium concentration?
Which of the following enzymes is NOT activated by increased cytosolic calcium concentration?
What is a consequence of mitochondrial damage related to cytochrome C?
What is a consequence of mitochondrial damage related to cytochrome C?
What is a potential outcome of calcium homeostasis loss during ischemia?
What is a potential outcome of calcium homeostasis loss during ischemia?
Which of the following factors contributes to the accumulation of free radicals in cells?
Which of the following factors contributes to the accumulation of free radicals in cells?
What is a primary consequence of an imbalance between free radical-generating and radical-scavenging systems?
What is a primary consequence of an imbalance between free radical-generating and radical-scavenging systems?
Which of the following is NOT a recognized trigger for free radical formation within cells?
Which of the following is NOT a recognized trigger for free radical formation within cells?
What is the primary way that reactive oxygen species damage cellular structures?
What is the primary way that reactive oxygen species damage cellular structures?
Which of the following is a free radical that can act as a mediator within the body?
Which of the following is a free radical that can act as a mediator within the body?
Which type of injury is NOT typically associated with free radical-mediated damage?
Which type of injury is NOT typically associated with free radical-mediated damage?
Which of the following indicates irreversible cell injury?
Which of the following indicates irreversible cell injury?
What is a definitive characteristic of irreversible injury in relation to mitochondrial function?
What is a definitive characteristic of irreversible injury in relation to mitochondrial function?
Which change is most clearly associated with the progression from reversible to irreversible cell injury?
Which change is most clearly associated with the progression from reversible to irreversible cell injury?
Which statement best describes the general capacity of a cell to recover from injury?
Which statement best describes the general capacity of a cell to recover from injury?
Which of the following phenomena consistently marks the transition to irreversible cell injury?
Which of the following phenomena consistently marks the transition to irreversible cell injury?
What type of necrosis is characterized by the transformation of tissue into a liquid viscous mass following a bacterial infection?
What type of necrosis is characterized by the transformation of tissue into a liquid viscous mass following a bacterial infection?
In which type of necrosis does the tissue become amorphous pink granular debris surrounded by granuloma?
In which type of necrosis does the tissue become amorphous pink granular debris surrounded by granuloma?
Which of the following types of necrosis typically involves the release of activated pancreatic lipases?
Which of the following types of necrosis typically involves the release of activated pancreatic lipases?
Gangrenous necrosis can evolve into which type through the action of bacteria and leukocytes?
Gangrenous necrosis can evolve into which type through the action of bacteria and leukocytes?
Coagulative necrosis is most characteristic of the hypoxic death of which types of cells?
Coagulative necrosis is most characteristic of the hypoxic death of which types of cells?
What distinguishes apoptosis from necrosis in terms of cellular integrity?
What distinguishes apoptosis from necrosis in terms of cellular integrity?
Which of the following accurately describes a physiologic cause of apoptosis?
Which of the following accurately describes a physiologic cause of apoptosis?
How does apoptosis prevent an inflammatory response compared to necrosis?
How does apoptosis prevent an inflammatory response compared to necrosis?
Which cellular process can occur simultaneously with necrosis?
Which cellular process can occur simultaneously with necrosis?
What is a pathological cause of apoptosis?
What is a pathological cause of apoptosis?
What is the characteristic appearance of necrotic cells due to glycogen particle loss?
What is the characteristic appearance of necrotic cells due to glycogen particle loss?
Which nuclear change is characterized by fragmentation and degraded chromatin structure?
Which nuclear change is characterized by fragmentation and degraded chromatin structure?
Which type of necrosis is primarily associated with the preservation of cell outlines due to protein denaturation?
Which type of necrosis is primarily associated with the preservation of cell outlines due to protein denaturation?
Which electron microscopy finding is commonly associated with necrotic cells?
Which electron microscopy finding is commonly associated with necrotic cells?
What occurs to chromatin during pyknosis?
What occurs to chromatin during pyknosis?
Which of the following statements accurately describes a role of antioxidants in cellular protection?
Which of the following statements accurately describes a role of antioxidants in cellular protection?
What is a significant consequence of mitochondrial dysfunction in cells?
What is a significant consequence of mitochondrial dysfunction in cells?
Which of the following factors contributes most to the irreversible injury of cells?
Which of the following factors contributes most to the irreversible injury of cells?
Which mechanism primarily contributes to membrane damage in ischemic cells?
Which mechanism primarily contributes to membrane damage in ischemic cells?
Which of the following is NOT a common result of reactive oxygen species on cellular structures?
Which of the following is NOT a common result of reactive oxygen species on cellular structures?
What role do antioxidants play in protecting cells from damage?
What role do antioxidants play in protecting cells from damage?
Which of the following enzymes is involved in removing hydrogen peroxide from cells?
Which of the following enzymes is involved in removing hydrogen peroxide from cells?
How does mitochondrial dysfunction contribute to membrane damage?
How does mitochondrial dysfunction contribute to membrane damage?
What is a major consequence of defects in membrane permeability?
What is a major consequence of defects in membrane permeability?
What is one of the consequences of lipid damage caused by reactive oxygen species?
What is one of the consequences of lipid damage caused by reactive oxygen species?
Flashcards are hidden until you start studying
Study Notes
Depletion of ATP
- ATP is essential for many cellular processes, including membrane integrity and synthesis.
- ATP is produced via oxidative phosphorylation and glycolysis.
- Reduced oxygen supply inhibits oxidative phosphorylation, leading to depletion of glycogen stores.
- Anaerobic metabolism (glycolysis) produces lactic acid, decreasing intracellular pH, which further hinders enzyme activity.
- Reduced ATP levels impair the sodium pump, resulting in intracellular sodium accumulation, potassium loss, cell swelling, and ER dilation.
- Failure of the calcium pump leads to calcium influx, damaging cellular components.
- Ribosomes detach from the endoplasmic reticulum (RER), and polysomes break down into monosomes, reducing protein synthesis.
Effects of Depleted ATP
- Reduced sodium pump activity causes sodium to accumulate intracellularly and potassium to diffuse out, resulting in cell swelling.
- Decreased oxygen supply leads to glycogen depletion and lactic acid accumulation, lowering intracellular pH.
- Failure of the calcium pump results in calcium influx, damaging various cellular components.
- Ribosome detachment from the RER reduces protein synthesis.
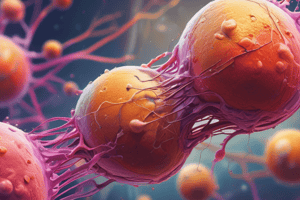
Mitochondrial Damage
- Mitochondria are susceptible to injury, particularly during hypoxic and toxic conditions.
- Increased intracellular calcium concentration, oxidative stress, breakdown of phospholipids, and breakdown of lipid products all contribute to mitochondrial damage.
- Mitochondrial damage can lead to the formation of a high-conductance channel (the mitochondrial permeability transition pore) in the inner mitochondrial membrane, which can be reversible initially but becomes irreversible, causing cell death.
- Mitochondrial damage can also result in leakage of cytochrome C into the cytosol.
Influx of Intracellular Calcium
- Ischemia and other injuries increase cytosolic calcium concentration.
- Elevated calcium activates enzymes like ATPases, phospholipases, proteases, and endonucleases, further damaging the cell.
Accumulation of Oxygen-Derived Free Radicals
- Small amounts of reactive oxygen species (ROS) are generated as byproducts of mitochondrial respiration.
- ROS can damage lipids, proteins, and nucleic acids.
- Cells have both defense systems to prevent ROS-induced damage and an imbalance between ROS generation and scavenging systems can lead to oxidative stress.
- Oxidative stress contributes to cell injury in various scenarios, including chemical and radiation injury, ischemia-reperfusion injury, cellular aging, and microbial killing by phagocytes.
Free Radicals
- Free radicals are chemical species with an unpaired electron in their outer orbit.
- They are generated in cells through various mechanisms, including:
- Absorption of radiant energy (UV light, X-rays)
- Enzymatic metabolism of exogenous chemicals or drugs
- Reduction-oxidation reactions during normal metabolism
- Transition metals like iron and copper
- Nitric oxide (NO)
- The main reactive oxygen species include superoxide anion radical (O₂⁻), hydrogen peroxide (H₂O₂), and hydroxyl ions (OH).
Main Effects of Reactive Species
- Lipid peroxidation of membranes, causing extensive damage to membranes, organelles, and cells.
- Protein fragmentation due to oxidative modification of proteins.
Membrane Damage
- Membrane damage in ischemic cells can result from ATP depletion and calcium-modulated activation of phospholipases.
- Direct damage by bacterial toxins, viral proteins, and other agents can also occur.
- Biochemical mechanisms contributing to membrane damage include:
- Mitochondrial dysfunction leading to increased intracellular calcium and activation of phospholipases
- Cytoskeletal abnormalities
- Reactive oxygen species causing lipid damage
- Lipid breakdown products
Mechanisms to Remove Free Radicals
- Cells have multiple mechanisms to remove free radicals and minimize damage, including:
- Antioxidants like vitamins A, C, and E
- Enzymes like catalase, superoxide dismutases, and glutathione peroxidase that break down hydrogen peroxide and superoxide anion.
Reversible and Irreversible Cell Injury
- Earliest changes associated with cell injury include:
- Decreased ATP generation
- Loss of cell membrane integrity
- Defects in protein synthesis
- Cytoskeleton damage
- DNA damage
- Within limits, the cell can compensate for these changes. Injury is reversible if the injurious stimulus is removed.
- Persistent or excessive injury leads to irreversible injury marked by:
- Severe mitochondrial vacuolization
- Extensive damage to plasma membranes
- Swelling of lysosomes
- Appearance of large, amorphous densities in mitochondria
- Irreversible injury is characterized by:
- Inability to reverse mitochondrial dysfunction (lack of oxidative phosphorylation and ATP generation) even after removing the injury.
- Profound loss of membrane function.
Morphology of Necrosis
- Necrotic cells display increased eosinophilia, a glassy homogeneous appearance, and vacuolation.
- Nuclear changes include:
- Karyolysis (fading of basophilia of chromatin)
- Pyknosis (nuclear shrinkage and increased basophilia)
- Karyorrhexis (fragmentation of the nucleus)
- Electron microscopy reveals discontinuities in plasma membranes, dilated mitochondria with amorphous densities, amorphous osmiophilic debris, and aggregates of fluffy material.
Types of Necrosis
- Coagulative necrosis: Preservation of the basic outline of the coagulated cell, characteristic of hypoxic death in tissues except the brain.
- Liquefactive necrosis: Complete digestion of dead cells, leaving a liquid viscous mass, typical of bacterial or fungal infections.
- Gangrenous necrosis: Occurs in limbs with loss of blood supply, often with superimposed bacterial infection leading to liquefactive changes.
- Caseous necrosis: A type of coagulative necrosis with a cheesy, amorphous pink granular debris, seen in tuberculosis infections.
- Fat necrosis: Focal fat destruction caused by activated pancreatic lipases, often seen in acute pancreatitis.
Apoptosis
- Apoptosis is a programmed cell death pathway.
- Cells activate their own enzymes to degrade DNA, nuclear proteins, and cytoplasmic proteins, while keeping the plasma membrane intact.
- Macrophages efficiently phagocytose apoptotic cells, preventing the release of cellular contents and inflammation.
- Apoptosis occurs both physiologically (eg., during embryogenesis) and pathologically (eg., to eliminate damaged cells).
Relationship between Apoptosis and Necrosis
- Apoptosis is fundamentally different from necrosis, which is characterized by membrane loss, enzymatic digestion of cell contents, and host reaction.
- Sometimes apoptosis and necrosis can coexist.
Description of Cellular Changes in Necrosis
- Fat necrosis involves the release of fatty acids combining with calcium to form chalky white areas (fat saponification).
- Histologically, fat necrosis appears as shadowy foci of necrotic fat cells with basophilic calcium deposits surrounded by inflammation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.