Podcast
Questions and Answers
Which of the following best describes the function of arteries?
Which of the following best describes the function of arteries?
- Take blood back to the heart
- Responsible for gas and nutrient exchange
- Regulate blood pressure
- Take blood away from the heart (correct)
Which layer of the blood vessel wall is primarily responsible for vasoconstriction and vasodilation?
Which layer of the blood vessel wall is primarily responsible for vasoconstriction and vasodilation?
- Lumen
- Tunica media (correct)
- Tunica intima
- Tunica externa
Nutrients and waste exchange occurs in which kind of vessel?
Nutrients and waste exchange occurs in which kind of vessel?
- Capillaries (correct)
- Veins
- Arteries
- Arterioles
The tunica intima of capillaries is composed of:
The tunica intima of capillaries is composed of:
What is the role of nitric oxide in regulating the contraction of smooth muscle in blood vessels?
What is the role of nitric oxide in regulating the contraction of smooth muscle in blood vessels?
Which of the following describes the vasa vasorum found in the tunica externa of blood vessels?
Which of the following describes the vasa vasorum found in the tunica externa of blood vessels?
Companion arteries and veins:
Companion arteries and veins:
What is the primary structural difference between elastic arteries and resistance arteries?
What is the primary structural difference between elastic arteries and resistance arteries?
Which type of blood vessel plays a key role in regulating blood pressure?
Which type of blood vessel plays a key role in regulating blood pressure?
What is the primary characteristic of continuous capillaries that allows them to constitute the blood-brain barrier?
What is the primary characteristic of continuous capillaries that allows them to constitute the blood-brain barrier?
Fenestrated capillaries are characterized by:
Fenestrated capillaries are characterized by:
In which location would you most likely find sinusoidal capillaries?
In which location would you most likely find sinusoidal capillaries?
What is the role of precapillary sphincters?
What is the role of precapillary sphincters?
Which characteristic allows veins to function as blood reservoirs?
Which characteristic allows veins to function as blood reservoirs?
What is the primary function of valves in veins?
What is the primary function of valves in veins?
Which percentage of blood is typically found within systemic veins at rest?
Which percentage of blood is typically found within systemic veins at rest?
Which of the following is an example of an alternative pathway for blood vessels?
Which of the following is an example of an alternative pathway for blood vessels?
What is the primary mechanism for the exchange of respiratory gases in capillaries?
What is the primary mechanism for the exchange of respiratory gases in capillaries?
What is the primary factor determining whether a substance moves into or out of the blood via diffusion?
What is the primary factor determining whether a substance moves into or out of the blood via diffusion?
In the context of capillary exchange, which process involves the movement of fluid and solutes due to a pressure gradient?
In the context of capillary exchange, which process involves the movement of fluid and solutes due to a pressure gradient?
What is the primary force that drives filtration at the arterial end of a capillary?
What is the primary force that drives filtration at the arterial end of a capillary?
Net filtration pressure (NFP) is calculated by:
Net filtration pressure (NFP) is calculated by:
Tissues with high metabolic activity have:
Tissues with high metabolic activity have:
What term describes the formation of new blood vessels from pre-existing ones?
What term describes the formation of new blood vessels from pre-existing ones?
What is the primary result of blocking angiogenesis in cancer treatment?
What is the primary result of blocking angiogenesis in cancer treatment?
Which of the following is a key factor that opposes blood flow?
Which of the following is a key factor that opposes blood flow?
According to Poiseuille's equation, what happens to resistance when vessel radius decreases?
According to Poiseuille's equation, what happens to resistance when vessel radius decreases?
What is the effect of increased blood viscosity on resistance and blood flow?
What is the effect of increased blood viscosity on resistance and blood flow?
Which factor has the most significant influence on blood flow?
Which factor has the most significant influence on blood flow?
What is the outcome of vasodilation on resistance and blood flow?
What is the outcome of vasodilation on resistance and blood flow?
Blood pressure is the:
Blood pressure is the:
What does the pulse pressure in arteries represent?
What does the pulse pressure in arteries represent?
What is the definition of Mean Arterial Pressure (MAP)?
What is the definition of Mean Arterial Pressure (MAP)?
What might be happening in a patient that has sustained capillary blood pressure and cerebral edema?
What might be happening in a patient that has sustained capillary blood pressure and cerebral edema?
What does the skeletal muscle pump assist in?
What does the skeletal muscle pump assist in?
During the respiratory pump, which process increases blood flow into thoracic veins?
During the respiratory pump, which process increases blood flow into thoracic veins?
Autoregulation is the process by which:
Autoregulation is the process by which:
Which of following will stimulate vasodilation?
Which of following will stimulate vasodilation?
A patient is suffering from long-term increase blood volume and blood pressure. What type of mechanism is triggered?
A patient is suffering from long-term increase blood volume and blood pressure. What type of mechanism is triggered?
The cardiovascular center is primarily located in the:
The cardiovascular center is primarily located in the:
Flashcards
Blood Vessel Functions
Blood Vessel Functions
Arteries take blood away from the heart, while veins return blood. Capillaries facilitate gas and nutrient exchange.
Tunics of Blood Vessels
Tunics of Blood Vessels
The walls of blood vessels are composed of three layers: tunica intima, tunica media, and tunica externa.
Tunica Intima
Tunica Intima
The tunica intima is the innermost layer of a vessel wall, consisting of endothelium and a subendothelial layer.
Tunica Media
Tunica Media
Signup and view all the flashcards
Tunica Externa
Tunica Externa
Signup and view all the flashcards
Artery vs. Vein Shape
Artery vs. Vein Shape
Signup and view all the flashcards
Capillary Structure
Capillary Structure
Signup and view all the flashcards
Elastic (Conducting) Arteries
Elastic (Conducting) Arteries
Signup and view all the flashcards
Muscular (Distributing) Arteries
Muscular (Distributing) Arteries
Signup and view all the flashcards
Arterioles Function
Arterioles Function
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
Characteristics of Capillaries
Characteristics of Capillaries
Signup and view all the flashcards
Structural types of Capillaries
Structural types of Capillaries
Signup and view all the flashcards
Continuous Capillaries
Continuous Capillaries
Signup and view all the flashcards
Fenestrated Capillaries
Fenestrated Capillaries
Signup and view all the flashcards
Sinusoidal Capillaries
Sinusoidal Capillaries
Signup and view all the flashcards
Capillary Beds
Capillary Beds
Signup and view all the flashcards
Vasomotion
Vasomotion
Signup and view all the flashcards
Venules
Venules
Signup and view all the flashcards
Traveling vessels
Traveling vessels
Signup and view all the flashcards
Systemic Veins
Systemic Veins
Signup and view all the flashcards
Anastomoses
Anastomoses
Signup and view all the flashcards
Capillary Exchange
Capillary Exchange
Signup and view all the flashcards
Vesicular transport.
Vesicular transport.
Signup and view all the flashcards
Fluids flow
Fluids flow
Signup and view all the flashcards
What is the NFP
What is the NFP
Signup and view all the flashcards
Degree of Vascularization
Degree of Vascularization
Signup and view all the flashcards
Angiogenesis
Angiogenesis
Signup and view all the flashcards
Bulk Flow
Bulk Flow
Signup and view all the flashcards
Blood pressure
Blood pressure
Signup and view all the flashcards
Myogenic Response
Myogenic Response
Signup and view all the flashcards
Vasoactive Chemicals
Vasoactive Chemicals
Signup and view all the flashcards
Neural regulation
Neural regulation
Signup and view all the flashcards
Baroreceptors
Baroreceptors
Signup and view all the flashcards
Chemoreceptors
Chemoreceptors
Signup and view all the flashcards
Hormonal regulation
Hormonal regulation
Signup and view all the flashcards
Types of vessles
Types of vessles
Signup and view all the flashcards
Cardiac output
Cardiac output
Signup and view all the flashcards
Hyper tension
Hyper tension
Signup and view all the flashcards
Pulmonary vs system
Pulmonary vs system
Signup and view all the flashcards
Study Notes
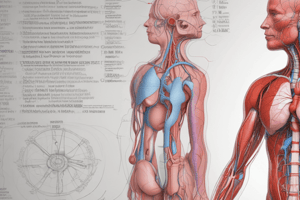
Cardiovascular System: Vessels and Circulation
- Arteries carry blood away from the heart.
- Veins carry blood back to the heart.
- Capillaries facilitate gas and nutrient exchange.
Vessel Wall Composition
- Walls are composed of three layers called tunics.
- These are the tunica externa, tunica media, and tunica intima.
- Arteries and veins have all three tunics.
- Capillaries only have a tunica intima, which consists of an endothelial layer and a basement membrane.
- The space inside a vessel is called the lumen.
Tunica Intima
- The tunica intima is the innermost layer of a vessel wall.
- It is composed of endothelium, which is a simple squamous epithelium.
- The endothelium provides a smooth surface for blood to move through the lumen.
- It contains the subendothelial layer or areolar connective tissue.
- The tunica intima releases substances to regulate smooth muscle contraction like nitric oxide, which causes relaxation, and endotunicn, which causes vasoconstriction.
Tunica Media
- The tunica media is the middle layer of a vessel.
- It comprises circularly arranged layers of smooth muscle cells with elastic fibers.
- Contraction causes vasoconstriction and relaxation causes vasodilation.
Tunica Externa
- The tunica externa is the outermost layer of a vessel, consisting of areolar connective tissue with elastic and collagen fibers.
- This layer anchors the vessel to other structures.
- It contains vasa vasorum which are small arteries for supplying very large vessels.
Companion Vessels
- Arteries and veins serving the same body region lie next to each other.
Artery vs Vein Comparison
- Arteries generally have a narrower lumen diameter than veins and veins a wider lumen.
- Artery walls are thicker than veins and veins walls are narrower.
- Arteries have a more maintained cross-sectional shape, even without blood, whereas veins tend to flatten out (collapse) without blood.
- The thickest tunic in arteries is the tunica media, while in veins it is the tunica externa.
- Arteries contain more elastic and collagen fibers in their tunics while veins have less.
- Valves are are abundant in veins but arteries contain none.
- Arteries have a higher blood pressure, around 100 mm Hg in larger arteries to 40 mm Hg in smaller arterioles, while veins have lower pressure ranging from 20 mm Hg in venules to 0 mm Hg in the inferior vena cava. Blood Flow and Oxygen Levels:
- Systemic arteries transport blood high in O₂, and systemic veins transport blood low in O₂.
- Pulmonary arteries transport blood low in O₂, and pulmonary veins transport blood high in O₂.
Capillaries
- Capillaries only contain tunica intima without a sub-endothelial layer.
- They are composed of endothelium and a basement membrane, with a thin wall that allows for exchange.
Elastic (Conducting) Arteries
- These are the largest, thick-walled arteries near the heart with a diameter between 2.5 to 1 cm.
- Their large lumen allows low-resistance conduction of blood.
- They contain elastin, especially in the tunica media so the artery can stretch and accommodate blood during ventricular systole and diastole.
Muscular (Distributing) Arteries
- These arteries deliver blood to body organs and are distal to elastic arteries, ranging from 1 cm to 0.3 mm. They have a thick tunica media and are active in vasoconstriction and dilation. They have elastic tissue in two layers: internal and external elastic lamina.
Arterioles
- These are the smallest arteries with diameters of 0.3 mm to 10 UM.
- Larger arterioles have three tunics, while smaller ones have only thin endothelium and a single layer of smooth muscle.
- Smooth muscle is usually somewhat constricted, regulated by vasomotor tone in the brainstem.
- Arterioles regulate systemic blood pressure and flow.
Atherosclerosis
- This is a progressive disease of elastic and muscular arteries.
- It involves the presence of atheroma, or atheromatous plaque.
- It involves the thickening of the tunica intima and narrowing of the arterial lumen, which may be caused by an injury response to endothelium.
- The injury response hypothesis is considered to be caused by infection, trauma, and hypertension.
- Atherosclerosis results in an inflammation reaction and atheroma formation.
- Lumen becomes narrower with atheroma enlargement, and plaques are not noticed until they restrict blood flow to a specific region.
Angioplasty
- During angioplasty, an uninflated balloon and compressed stent are passed through a catheter to the area of the obstructed artery.
- The balloon inflates, expanding the stent and compressing the atheroma.
- The stent typically remains in the vessel as the balloon is deflated and the catheter withdrawn.
Capillaries
- These are the smallest blood vessels, 8-10 UM in diameter.
- The capillary walls consist of an endothelial layer on a basement membrane.
- Red blood cells travel through capillaries in a single file.
- Three Structural Types: continuous capillaries, fenestrated capillaries, and sinusoidal capillaries
- Permeability varies based on the type of capillary
- Gas and nutrient exchange occurs in the capillaries, which connect arterioles with venules.
Continuous Capillaries
- The most common type of capillaries and are found in skin, muscles, lungs, and the CNS.
- They have endothelial cells that provide an uninterrupted lining, with tight junctions connecting the cells.
- Intercellular clefts are the gaps that allow small particles such as glucose and gases to pass, while large particles, cells, or proteins can not pass.
- Continuous capillaries constitute the blood-brain barrier and have no intercellular clefts.
Fenestrated Capillaries
- These are found in kidneys, small intestines, endocrine organs, etc., where a lot of fluid transport occurs.
- Characterized by an endothelium riddled with pores or fenestrations.
- They exhibit a greater permeability than other capillaries and allow for smaller plasma protein movement.
Sinusoidal Capillaries
- Leaky, fenestrated capillaries with large lumens with incomplete lining of endothelial cells.
- They are found in the liver, bone marrow, lymphoid tissue, and some endocrine glands.
- Blood flow is sluggish so they Allow large molecules such as proteins and blood cells to pass between the blood and surrounding tissues.
Capillary Beds
- Groups of 10 to 100 capillaries functioning together. They are fed by metarterioles, a vessel branch of an arteriole.
- The proximal part of a metarteriole is encircled by scattered smooth muscle cells.
- The distal part, or thoroughfare channel, lacks smooth muscle cells and connects to a post capillary venule, serving as a draining bed..
- Vessels are branching from metarterioles.
Precapillary Sphincter
- A smooth muscle ring surrounds the origin of a true capillary.
- Relaxation permits blood flow and contraction causes blood to bypass the capillary bed.
- Vasomotion is the cycle of contracting and relaxing of precapillary sphincters and allows for only 1/4 of the body's capillary beds being open at any given time.
- Perfusion is the blood flow through body tissues.
Venules
- The smallest veins, with a 8-100 UM diameter.
- They have all three tunics.
- They serve as companion vessels with arterioles.
- They merge to form veins.
Veins
- Small and medium-sized veins are companion vessels with muscular arteries.
- Large veins travel with elastic arteries.
- They ensure blood flow toward the heart.
- Veins are made of tunica intima + elastic and collagen fibers with a similar valve structure to the heart's semilunar valves.
- The act as blood reservoirs.
- They contain valves to prevent blood pooling.
Blood Distribution
- At rest, 70% of blood is in systemic circulation so 55% of the total blood is in systemic veins, 10 percent in systemic arteries, and 5 percent in systemic capillaries. ,
- In pulmonary circulation, 18% of blood is circulating.
- 12% of the total volume of blood is in the heart.
Blood Vessel Pathways
- Blood vessels can be arranged in either simple pathways or in alternative pathways with anastomoses.
- Simple pathway: Artery -> capillary bed -> veins -> heart
- Anastomoses: Joining together of blood vessels, provides an alternative pathway for blood transportation
Capillary Exchange of Respiratory Gases and Nutrients
- O₂, CO₂, nutrients, and metabolic wastes diffuse or are transported between the blood and the interstitial fluid along concentration gradients.
Diffusion
- Substances moves in or out of blood dependent on its concentration gradient..
- Oxygen, hormones, nutrients, and small solutes move from blood to the interstitial fluid, .
- Carbon dioxide and wastes diffuse from tissue to blood.
Vesicular Transport
- Endothelial cells use endocytosis/pinocytosis to transport fluids across capillary walls.
- It moves substances across capillaries.
Bulk Flow
- Fluids move along a pressure gradient.
- Fluids and dissolved substances move in large amounts.
- Movement direction is determined by the net pressure of opposing forces, notably the balance between Hydrostatic and colloid pressure
- In filtration fluid moves out of the blood on arterial end.
- In reabsorption, fluid moves back into the blood at venuous end.
Hydrostatic Pressure
- Force exerted by a fluid
Colloid Osmotic Pressure
- The "pull" on water due to proteins
Net Filtration Pressure
- Equal to all the forces acting on a capillary bed.
- NFP is the difference between net hydrostatic pressure and net colloid osmotic pressure.
- At the arterial end of a bed, hydrostatic pressure dominates (fluids flow out).
- At the venous end of a bed, colloid osmotic pressure dominates leading to fluids flow in.
- Excess fluid is returned to the blood via the lymphatic system.
Degree of Vascularization
- The amount of blood vessels in a tissue.
- It depends on the tissue type.
- Metabolically active tissues have high vascularity.
- Tendons, ligaments, epithelia, and cornea, have little or no vascularity.
- The amount of vascularization may increase over time through angiogenesis and decrease through regression.
Angiogenesis
- Angiogenesis is the formation of new blood vessels.
- Two types are sprouting and intussusception and can occur over weeks to months to increase potential perfusion.
- It is the Skeletal muscle responds used to increase blood flow in response to aerobic training.
- It occurs in adipose tissue with weight gain and is the way coronary vessels respond to gradual blockage.
Steps of Angiogenesis
- Induction of VEGF signaling: Vascular endothelial growth factor
- Formation of tip cells.
- Stalk cell development.
- Vessel outgrowth.
- Anastomosis & perfusion.
- Maturation & stabilization.
Atherosclerosis
- Angiogenesis forms more blood vessels to feed tumors
- If tumor angiogenesis can be blocked. this deprives the tumor of nutrients.
- Many angiogenesis inhibitors are monoclonal antibodies that end in "-mab".
Regression
- Regression is the return to previous state of blood vessels.
- Examples include, skeletal muscle after individual becomes sedentary or in adipose tissue when weight is lost
Myogenic Response
- Contraction and relaxation of smooth muscle in BV walls to increase or decrease blood flow
- Constriction occurs if systemic blood pressure rises and more blood enters an arteriole.
- Dilation occurs if systemic blood pressure decreases and amount of blood decreases
- Myogenic response involves both contraction of smooth muscle in blood vessel walls in response to an increase in stretch and relaxation of smooth muscle in blood vessel walls in response to a decrease in stretch to maintain a constant blood flow..
Local, Short-Term Regulation
- Blood flow is regulated based on need Changes occur when metabolic activity changes or tissue is damaged.
Vasoactive Chemicals
- Vasoactive chemicals can alter blood flow.
- Vasodilators will dilate arterioles and relax precapillary sphincters.
- Vasoconstrictors will constrict arterioles and cause contraction of precapillary sphincters..
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.