Podcast
Questions and Answers
Flashcards
What is syncope?
What is syncope?
Abrupt, transient loss of consciousness and postural tone due to inadequate O2 or glucose to the brain.
Pulsus paradoxus
Pulsus paradoxus
An exaggerated decrease in systolic pressure during inspiration, detected as a weak pulse.
Thoracic auscultation
Thoracic auscultation
Identify normal sounds, detect abnormal sounds, and evaluate cardiac and pulmonary rhythms.
Study Notes
- This presents an introduction to the examination of the cardiovascular system and VMC 5110 by Dr. C Hankanga Malombola
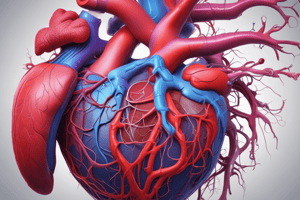
Cardiovascular Overview
- The pulmonary artery transports blood to the lungs, where it is oxygenated
- The pulmonary vein brings oxygenated blood from the lungs back to the heart
- The aorta distributes oxygenated blood to the body
- The Vena cava returns deoxygenated blood from the body to the heart
Heart Anatomy
- The heart is composed of the right atrium, the left atrium, the right ventricle, and the left ventricle
- Relevant components include the aortic arch, pulmonary artery, coronary vessels, and chordae tendineae
History and Signalment
- Information regarding age, breed, and sex is relevant
- Vaccination status?
- Any changes in diet and water intake?
- Where was the animal obtained?
- Is the pet housed indoors or outdoors?
- How much time is spent outside, supervised?
- Normal activity level?
- Any coughing, excessive panting, gagging, or vomiting?
- Any recent changes in urinary habits?
- Episodes of fainting or weakness?
- Are the tongue and mucous membranes always pink, especially during exercise?
- Recent changes in attitude and activity level?
- Current medications?
- Any medications used in the past, and were they effective?
Clinical signs of heart disease
- General clinical signs include coughing, dyspnea, exercise intolerance, syncope, murmurs, and pulse abnormalities even if the animal is not in heart failure
- Weakness and syncope occur when cardiac output is reduced due to heart disease or heart failure
- Exercise intolerance and tiring may be caused by reduced skeletal muscle perfusion
Syncope Defined
- Syncope indicates an abrupt and transient loss of consciousness and postural tone
- Syncope is caused by an inadequate supply of oxygen or glucose to the brain
- Syncope can be differentiated from intermittent weakness or seizures
- It is characterized by rear limb weakness, sudden collapse, lateral recumbency, stiffening of forelimbs, opisthotonus, micturition, and vocalization
- Tonic/clonic motion, facial fits, defecation aura, postictal dementia, and neurological deficits are not characteristic of syncope
- Cardiac, pulmonary, metabolic, hematological, and neurological issues can cause syncope or episodic weakness
Clinical Signs: Cough
- Cough is typically seen in both respiratory and cardiac disease
Differentiating Cough: Cardiac vs Respiratory
- Cardiac: Thin/weight loss, worse at night with soft cough, possible rare pink sputum
- Respiratory: Normal or obese, often caused by exercise, ± mucopurulent sputum, harsh, debilitating
- Lung sounds in cardiac are none, crackles, wheezes most common, in the respiratory, it is none, wheezes, crackles; wheezes most common
- Airway cytology is normal in cardiac, Inflammatory or neoplastic in the respiratory
- Diuretics are responsive in cardiac patients but unresponsive in respiratory
- Hemogram in cardiac is normal or stress, showing normal results or ± polycythemia in respiratory
- The heart rate/rhythm is usually rapid, sinus rhythm/tachycardia in cardiac vs normal to slow, sinus arrhythmia in respiratory
Observation and General Examination
- Assess attitude, posture, body condition, level of anxiety, and respiratory pattern during the general examination
Physical Exam: Mucous Membranes
- Mucous membranes and capillary refill time (CRT) are assessed to determine peripheral perfusion, using oral, ocular, prepuce, or vaginal areas
Abnormal Mucous Membrane Colors:
- Pale: Anemia or poor cardiac output/high sympathetic tone
- Injected/Brick-red: Polycythemia, sepsis, excitement, other causes of peripheral dilation
- Cyanotic: Pulmonary parenchymal disease, airway obstruction, pleural space disease, pulmonary edema, right to left shunting, hypoventilation, shock, cold exposure, or methemoglobinemia
- Differential cyanosis: Reversed PDA where the head and forelimbs receive oxygenated blood, and caudal parts receive desaturated blood via the ductus
- Icterus: Hemolysis, hepatobiliary disease, or biliary obstruction
Physical Exam: Jugular Veins
- Systemic and right heart filling pressures are reflected at the jugular veins
- Veins should not be distended when the animal is standing with its head in a normal position
- Persistent jugular distention associated with right-sided heart failure, compression of cranial vena cava, or jugular or caudal vena cava thrombosis
- Jugular pulsations extending more than one-third of the way up the neck from the thoracic inlet are abnormal
- To differentiate true pulse from carotid transmission, occlude the vein lightly below the area of the visible pulse; if the pulse disappears, then it is a true jugular pulse; if it continues, it is being transmitted from the carotid
Causes of Jugular Distension/Pulsation:
- Distension alone is caused by Pericardial effusion/tamponade, right atrial mass/inflow obstruction, dilated cardiomyopathy, cranial mediastinal mass, and jugular v./cranial vena cava thrombosis
- Pulsation+Distension include Tricuspid insufficiency of any cause, Pulmonic stenosis, heartworm disease, pulmonary hypertension, ventricular premature contractions, and complete heart block
Hepatojugular Reflux
- Hepatojugular reflux is due to impaired right ventricular filling or tricuspid regurgitation
- Positive test: Applies firm pressure to the cranial abdomen while the animal stands, in order to increase venous return and cause transient jugular distension
Arterial Pulses
- Arterial pulses must be assessed for their strength, regularity, and pulse rate
- The difference between the systolic and diastolic arterial pressure equals pulse pressure
- When the difference is wide, the pulse is strong on palpation (hyperkinetic)
- When the difference is small, the pulse is weak (hypokinetic)
- If the rise to maximum systolic pressure is prolonged in severe SAS, the pulse feels weak (pulsus parvus et tardus)
- Alternately weak and strong pulses may indicate severe myocardial failure (pulsus alterans)
- An exaggerated decrease in systolic pressure during inspiration may indicate cardiac tamponade (pulsus paradoxus)
- Pulses should be palpated and compared; the femoral pulse should be evaluated simultaneously with the direct heart rate
- Fewer femoral pulses than heart beats indicate pulse deficits
- Weak pulse is associated with Excitement, HCM (cats), and Fever/sepsis
- Strong Pulses are associated with Dilated Cardiomyopathy, Aortic Stenosis, Pulmonic Stenosis
- Very strong bounding pulses are associated with Fever/sepsis, Shock Dehydration, and PDA
Additional Assessment
- Precordium: Palpate both sides of the animal's chest, strongest beat is in the left 5th intercostal space near the costochondral junction
- The precordial impulse will be stronger on the left side
- A shifted precordial impulse may indicate cardiomegaly or thoracic mass
- Reduced intensity may indicate obesity, weak cardiac contractions, pericardial effusion, intrathoracic masses, pleural effusion, or pneumothorax
- Palpable vibrations may indicate loud murmurs
Evaluation for Fluid Accumulation
- Evaluation of fluid accumulation includes in the body cavities, subcutis in dependant areas, and pulmonary oedema through observing, palpating, and auscultating
Thoracic Auscultation
- Identify normal heart sounds.
- Determine presence or absence of abnormal sounds.
- Assess cardiac rhythm
- Evaluate pulmonary sounds
Auscultation: Heart Sounds & Murmurs
- Heart sounds created by turbulent blood flow and associated vibrations in adjacent tissue during the cardiac cycle.
- Transient sounds are short duration; cardiac murmurs are longer duration.
- Heart sounds are characterized by frequency, amplitude, duration and quality/timbre
- The point of maximum intensity PMI of any abnormal sound should be located
- S1 is associated with closure and tensing of AV valves at the onset of systole
- S2 is associated with closure of aortic and pulmonic valves
- S3 and S4 diastolic are not audible in normal dogs and cats
- Loud S1 indicates thin chest wall, high sympathetic tone, tachycardia, systemic arterial hypertension
- Muffled S1 indicates obesity, pericardial effusion, diaphragmatic hernia, DCM, hypovolemia/poor ventricular filling, or pleural effusion
- Loud S2 indicates pulmonary hypertension
Cardiac Murmurs
- Represent sounds of longer duration than transient heart sounds
- Cardiac Murmurs are caused by turbulent flow in the heart and adjacent blood vessels
- Innocent murmurs should disappear as the dog matures and are thought to be due to larger stroke volumes in puppies
- Described by timing, intensity, radiation, quality, and pitch
Additional Sound
- Gallop sounds describe when S3 and S4 are audible, when the heart may sound like a galloping horse (gallop rhythm)
- Low freq. sounds
- Audible S3 indicates a ventricular dilation with myocardial failure
- Audible S4 indicates increased ventricular stiffness and hypertrophy
Valve Location for Auscultation
- Mitral: Lift, within the 5th intercostal space at the costochondral junction
- Pulmonic: Left, Between 2nd and 4th intercostal spaces just above the sternum
- Aortic: Left, within the 4th intercostal space just above the costochondral junction
- Tricuspid: Right, between the 3rd and 5th near the costochondral junction
Murmur Shapes and Descriptions
- Holosystolic refers to plateau or regurgitant
- Crescendo-decrescendo refers to diamond-shaped ejection
GRADING HEART MURMURS
- Grade I is a very soft murmur, heard only in a quiet room
- Grade II is a soft murmur but easily heard
- Grade III is a moderate-intensity murmur that radiates somewhat
- Grade IV is a loud murmur but not accompanied by precordial thrill and radiates over a larger area than III
- Grade V is a loud murmur with palpable precordial thrill
- Grade VI is a very loud murmur that can be heard with a stethoscope off the chest wall and is accompanied by a precordial thrill
Describing Murmurs
- Intensity is based on grade
- Position and Duration in Cardiac Cycle: Systolic,diastolic,pan-, holo- ,early-, late- continuous
- Valve area corresponding to PMI: Pulmonic, Mitral, Aortic, Tricuspid
- Quality: Plateau, crescendo, decrescendo, or diamond
- Character/Pitch: Blowing, musical, honking, harsh, or noisy, etc
Auscultatory findings
- Sub (aortic stenosis: Timing is systolic, ejection (crescendo-decrendo), and PMI is in the left base
- Mitral valve dysplasia: Timing is systolic, regurgitant (holosystolic, and PMI is in the left apex
- PDA: Timing is continuous; the sound is machinery and PMI is in the left base
- Pulmonic Stenosis: Timing is systolic ejection crescendo-decrendo, PMI is in the left base
- Tetralogy of Fallot: Timing is systolic , ejection crescendo-decrendo, PMI is in the left base
- Tricuspid valve dysplasia: Timing is systolic, regurgitant holosystolic, PMI is in the right midprecordium
- VSD: Timing is systolic, regurgitant (holosystolic), PMI is in the right base
- Atrial septal defect: Timing is systolic (diastolic, the sound is ejection, PMI is in the left base
Listen to Murmurs
- More information is available at http://www.veterinarypartner.com/Content.plx?P=A&S=0&C=0&A=2488&EVetID=3002209
Additional Testing - Radiography
- Radiography helps to differentiate pulmonary from cardiac disease, judge severity of oedema or pleural effusions
- Assess the size and shape of the heart in cardiac images
- Assess cardiac chamber and intrathoracic blood vessel enlargements
- Normal VHS: L + S = 8.5-10.5
Electrical Testing
- Atrial depolarization corresponds to the P Wave on the ECG
- PR interval in electrocardiography corresponds to AV node conduction
- Ventricular Depolarization corresponds to the QRS Complex
- Purkinje fibers play a role in Ventricular Depolarization
- Ventricular repolarization corresponds to the T Wave
Normal ECG Waveforms and Descriptions
- P Wave: Atrial muscle activation wave, normally positive in leads II and aVF
- PR Interval: Aka PQ interval, duration of atrial muscle activation, and conduction over the AV node, bundle of His, and Purkinje fibers, measure from the start of the P wave to the QRS complex
- QRS Complex: Ventricular muscle activation wave; Q is the first negative deflection, R is the first positive deflection, and S is the negative deflection after R
- J Point: Point after the QRS complex and ST-T
- ST Segment: Represents the period between ventricular depolarization and repolarization correlates with phase 2 of the action potential
- T Wave: Ventricular muscle repolarization wave
- QT interval: Total time of ventricular depolarization and repolarization and measures from QRS complex start to end of T wave
Electrocardiography
- ECG often run when rhythm disturbances are present
- Height and width of P and QRS complexes can reveal chamber enlargements
- Abnormal QRS complexes can show electrolyte imbalances
- It can diagnose specific arrhythmias
Additional testing
- Echocardiography is non-invasive, used to evaluate cardiac chamber size, wall thickness, wall motion, valve configuration and motion and the proximal great vessels
- Doppler can measure direction and velocity of blood flow ###Angiography
- Angiography is done by injection of radiopaque dye to identify anatomic abnormalities especially congenital heart disease as well as the path of blood flow
- Cardiac catheterisation involves the placement of specialized catheters to measure pressure, cardiac output, and blood oxygen in different areas of the heart and vasculature
- It is important in estimating the severity of cardiac defects
biochemical Markers
- Cardiac troponins regulatory proteins associated with the thin contractile filaments.
- Cardiac troponin I (cTnl and cardiac troponin T (cTnT increase within a few hours of acute myocardial injury or necrosis
- Myocardial-bound creatinine kinase is an indicator of cardiac muscle damage
- Atrial natriuretic peptide (ANP) and Brain natriuretic peptide (BNP)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.