Podcast
Questions and Answers
Which statement accurately describes the function of the semilunar valves?
Which statement accurately describes the function of the semilunar valves?
- They close during systole to prevent backflow.
- They open during systole to allow blood to exit the heart. (correct)
- They regulate pressure gradients throughout the cardiac cycle.
- They open during diastole to facilitate blood flow.
What is the normal range for Right Atrial Pressure (RAP) in mmHg?
What is the normal range for Right Atrial Pressure (RAP) in mmHg?
- 15-25
- 2-8 (correct)
- 10-15
- 4-12
How does the pressure gradient affect the function of the atrioventricular valves?
How does the pressure gradient affect the function of the atrioventricular valves?
- They remain closed at all times due to high pressure.
- They close when the pressure in the heart is equal.
- They open during diastole when pressure is higher in the ventricles.
- They open during systole when pressure is higher in the atria. (correct)
What does the pressure gradient (PG) relate to in cardiac physiology?
What does the pressure gradient (PG) relate to in cardiac physiology?
What is the function of the Left Ventricular Pressure (LVP) in the cardiac cycle?
What is the function of the Left Ventricular Pressure (LVP) in the cardiac cycle?
Flashcards
Pressure Gradient (PG)
Pressure Gradient (PG)
The difference in pressure between two locations. It drives the flow of blood.
Atrioventricular (AV) Valves
Atrioventricular (AV) Valves
Valves in the heart that open during diastole (heart relaxation) allowing blood to flow from the atria to the ventricles.
Semilunar (SL) Valves
Semilunar (SL) Valves
Valves in the heart that open during systole (heart contraction) allowing blood to flow from the ventricles to the arteries.
Right Atrial Pressure (RAP)
Right Atrial Pressure (RAP)
Signup and view all the flashcards
Left Ventricular Pressure (LVP) Transfer
Left Ventricular Pressure (LVP) Transfer
Signup and view all the flashcards
Study Notes
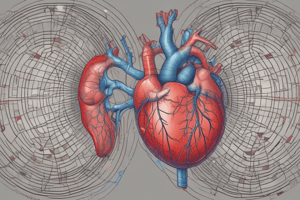
Cardiac Physiology Part 1
- Left heart pressures are greater than right heart pressures
- Atrioventricular (AV) valves (mitral and tricuspid) open during diastole
- Semilunar valves (aortic and pulmonary) open during systole
- Blood moves from higher pressure areas to lower pressure areas
- Pressure gradient (PG) drives blood flow
- Normal cardiac pressures are measured in mmHg
- RAP: 2-8 (mean)
- RVP: 15-25
- PAP: 15-25
- PCWP: 2-12
- LAP: 2-12
- LVP: <120
- Ao: <120
- Cardiac cycle has four phases:
- Diastole
- Isovolumic Contraction Time (IVCT)
- Systole
- Isovolumic Relaxation Time (IVRT)
Diastole
- Diastole is the period of heart relaxation when the ventricles fill with blood
- Atrial pressure rises as atriums fill
- AV valves open when atrial pressure exceeds ventricular pressure
- Blood flows from high pressure to low pressure
- Three phases of diastole:
- Early Rapid Filling ("the dump")
- Diastasis ("the slow down")
- Atrial Contraction ("the kick")
End-Diastolic Volume (EDV)
- EDV is the largest volume of blood in the heart during the cardiac cycle
- Ventricular pressures are higher than atrial pressures
- Closure of AV Valves signals the end of diastole
Atrioventricular Valves & Diastolic Pressure Gradients
- Pressure from the left atrium (LA) across the mitral valve (MV) to the left ventricle (LV)
- Mean LAP: 2-12 mmHg
- Diastolic LVP: 3-12 mmHg
- Pressure from the right atrium (RA) across the tricuspid valve (TV) to the right ventricle (RV)
- Mean RAP: 2-8 mmHg
- Diastolic RVP: 2-8 mmHg
Semilunar Valves & Diastolic Pressure Gradients
- Diastolic LVP: 3-12 mmHg
- Diastolic (aortic) pressure: ~80 mmHg
- Large pressure gradient (~70 mmHg) keeps the aortic valve (AoV) shut
- Diastolic RVP: 2-8 mmHg
- Diastolic (pulmonary) pressure: 4-12 mmHg
- Sufficient pressure gradient keeps the pulmonary valve (PV) shut
Isovolumic Contraction Time (IVCT)
- Short period immediately preceding systole
- Ventricles are in the process of contracting, but blood has not yet left the ventricles
- Ventricular volumes remain constant.
- All four valves are closed
- Ventricular pressures increase
- Ventricular wall thickness increases
- Atrial filling continues
Systole
- Systole is a period of heart contraction when ventricles eject blood
- Ventricular pressure exceeds great artery pressure; semilunar valves open
- Blood ejects from ventricles to great arteries
- Blood flows from high pressure areas to lower pressure areas
- Semilunar valves close which signals the end of systole.
End-Systolic Volume (ESV)
- ESV is the smallest volume of blood in the heart during the cardiac cycle
- Represents the amount of blood remaining in ventricles at the end of systole
Systolic & Diastolic Function Recap
- Ventricular pressure exceeds great artery pressure
- Cause SL valves to open
- SL valves close (2nd heart sound)
- Systolic function, diastolic function dependent on several components:
- Contractility
- Wall thickening & motion
- Indication of adequate coronary blood flow and oxygen
- Chamber size
- Ventricular end-diastolic pressure
Wall Motion Abnormalities (WMA)
- Cardiac walls that do not thicken/contract properly
- May indicate ischemic heart disease
- Can be global (entire chamber) or local (small area)
Wall Motion Terminology
- Hyperkinetic: excessive wall motion (walls squeezing more than normal)
- Hypokinetic: decreased wall motion (walls squeezing less)
- Akinetic: no wall movement or thickening (walls not squeezing)
- Dyskinetic: movement away from the center, or in the opposite direction (may indicate heart attack)
What Causes Wall Motion Abnormalities (WMA)?
- Myocardial ischemia (starvation of blood flow to the heart muscle) can lead to myocardial infarction
- Abnormal relaxation (diastolic dysfunction)
- Reduced systolic function
Heart Sound Recap
- 1st heart sound (S1): AV valve closure ("lub")
- 2nd heart sound (S2): SL valve closure ("dub")
- 3rd heart sound (S3): Early rapid filling ("ventricular dump")
- 4th heart sound (S4): Atrial contraction ("ventricular kick")
Cardiac Function
- Cardiac function relates to the heart's ability to pump oxygenated blood successfully under various circumstances.
- Supply needs to equal demand
- Compensation mechanisms (e.g., increased heart rate, increased force of contraction) adjust during exercise
- Reduced demand during rest leads to slower heart rate and reduced contraction force
- Function is dependent upon systolic and diastolic functions
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.