Podcast
Questions and Answers
What physiological process is directly responsible for generating the electrical current in the sinoatrial (SA) node?
What physiological process is directly responsible for generating the electrical current in the sinoatrial (SA) node?
- The movement of positively and negatively charged ions across the cell membrane (correct)
- The metabolism of glucose within the cardiac muscle cells
- The rapid diffusion of oxygen across the cell membrane
- The mechanical stretching of the cardiac muscle fibers
A key strategy of cardiac compensation involves minimizing heart rate to conserve energy and reduce myocardial oxygen demand.
A key strategy of cardiac compensation involves minimizing heart rate to conserve energy and reduce myocardial oxygen demand.
False (B)
If a patient with mitral valve insufficiency develops congestive heart failure, what class of vasodilator is specifically indicated to reduce afterload and improve cardiac output?
If a patient with mitral valve insufficiency develops congestive heart failure, what class of vasodilator is specifically indicated to reduce afterload and improve cardiac output?
Arterial dilators
The use of furosemide in treating congestive heart failure can lead to a potentially dangerous electrolyte imbalance known as ______, which may increase the risk of digitalis toxicity.
The use of furosemide in treating congestive heart failure can lead to a potentially dangerous electrolyte imbalance known as ______, which may increase the risk of digitalis toxicity.
Match the following antiarrhythmic drug classes with their primary mechanism of action:
Match the following antiarrhythmic drug classes with their primary mechanism of action:
In a patient with atrial fibrillation, which drug is used to slow atrioventricular conduction time and control heart rate?
In a patient with atrial fibrillation, which drug is used to slow atrioventricular conduction time and control heart rate?
The primary effect of nitroglycerin ointment in treating heart failure is to increase afterload, thereby improving cardiac output.
The primary effect of nitroglycerin ointment in treating heart failure is to increase afterload, thereby improving cardiac output.
Why must pregnant women avoid handling telmisartan?
Why must pregnant women avoid handling telmisartan?
Unlike skeletal muscle, cardiac muscle cells transmit ______ impulses from one cell to the next without requiring a nerve.
Unlike skeletal muscle, cardiac muscle cells transmit ______ impulses from one cell to the next without requiring a nerve.
Match each disease to the associated valve that can lead to ascites when affected:
Match each disease to the associated valve that can lead to ascites when affected:
Which drug would be effective in the treatment of supraventricular tachyarrhythmias?
Which drug would be effective in the treatment of supraventricular tachyarrhythmias?
The SA node transmits electrical impulses through the AV node into the purkinje fibers.
The SA node transmits electrical impulses through the AV node into the purkinje fibers.
What electrolyte imbalance is caused by furosemide that poses a risk of digitalis toxicity?
What electrolyte imbalance is caused by furosemide that poses a risk of digitalis toxicity?
If a focus of cardiac muscle depolarizes out of sequence with the SA node, ______ occurs.
If a focus of cardiac muscle depolarizes out of sequence with the SA node, ______ occurs.
Match the following types of cardiomyopathy with breeds likely affected:
Match the following types of cardiomyopathy with breeds likely affected:
What is the primary effect of Alpha 1 receptors?
What is the primary effect of Alpha 1 receptors?
Beta 2 receptors produces positive chronotropic effects.
Beta 2 receptors produces positive chronotropic effects.
What is the antidote for atropine?
What is the antidote for atropine?
An ectopic _______ of cells outside the sinoatrial node causes Arrhythmia.
An ectopic _______ of cells outside the sinoatrial node causes Arrhythmia.
Match the drug to the definition by description:
Match the drug to the definition by description:
Flashcards
Systole
Systole
The phase when the heart muscle contracts and ejects blood from the atria to the ventricles and from the ventricles to the arteries.
Diastole
Diastole
The phase when the heart muscle relaxes and fills with blood.
Sinoatrial node (SA node)
Sinoatrial node (SA node)
An area of specialized cardiac muscle cells in the heart capable of automatically generating electrical impulses.
Polarization
Polarization
Signup and view all the flashcards
Depolarization
Depolarization
Signup and view all the flashcards
AV Node
AV Node
Signup and view all the flashcards
Positive inotropic and chronotropic effects
Positive inotropic and chronotropic effects
Signup and view all the flashcards
Alpha 1 receptors
Alpha 1 receptors
Signup and view all the flashcards
Beta 2 receptors
Beta 2 receptors
Signup and view all the flashcards
Yes, its a compensatory mechanism.
Yes, its a compensatory mechanism.
Signup and view all the flashcards
Dilative cardiomyopathy
Dilative cardiomyopathy
Signup and view all the flashcards
Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy
Signup and view all the flashcards
Congestive heart failure (CHF)
Congestive heart failure (CHF)
Signup and view all the flashcards
Epinephrine
Epinephrine
Signup and view all the flashcards
Dopamine
Dopamine
Signup and view all the flashcards
Bipyridine derivatives
Bipyridine derivatives
Signup and view all the flashcards
Pimobendan
Pimobendan
Signup and view all the flashcards
Arrhythmia
Arrhythmia
Signup and view all the flashcards
Class 1A Antiarrhythmics
Class 1A Antiarrhythmics
Signup and view all the flashcards
lass 1B Antiarrhythmics
lass 1B Antiarrhythmics
Signup and view all the flashcards
Study Notes
Introduction
- Heart disease is often diagnosed in veterinary medicine due to increased pet longevity
- Acquired heart disease is most prevalent in geriatric patients
- Congenital heart disease presents more often in young animals
- Treatment of heart disease is very specific to both the patient and its disease stage
- Cardiovascular drugs have a small margin of safety and requires careful monitoring
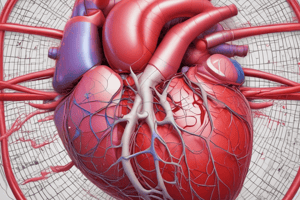
Cardiac Anatomy/Physiology
- The body delivers deoxygenated blood into to the right atrium via the cranial and caudal vena cava
- Blood passes though the right atrioventricular/tricuspid valve into to the right ventricle
- During Systole the right AV valve closes
- The right ventricle pushes deoxygenated blood out the pulmonic valve to the pulmonary arteries and then to the alveoli to become oxygenated
- Blood returns to the heart via pulmonary veins leading to the left atrium
- The blood then flows from the left atrium through the left atrioventricular/mitral valve into the left ventricle
- During systole the mitral valve closes
- The left ventricle then contracts pushing blood through the aortic valve into the coronary arteries, the aorta and arteries of the body
Cardiac Cycle
- Each complete contraction and relaxation is termed the cardiac cycle
- Systole is when the heart muscle contracts pushing blood to atria/ventricles
- Diastole is when the heart muscle relaxes and refills with blood
- The sinoatrial node (SA) node emits heartbeat impulses
- The SA node is a specialized cardiac muscle cell are that automatically generates the electrical impulses that trigger the heart to beat
- The SA node generates electrical current by moving cations (Na+, K+, Ca++) and anions (Cl-)
- Cations pumped across the cell membrane is polarization
- Opening of the gates on cell membrane causes cations flow out which equalizes charge as the cell depolarizes
- Action of depolarization generates the electrical current that tells cardiac muscles to contract
- Electrical current from the SA node takes two routes from heart base to its apex
- One is fast and goes via specific cardiac cells of the SA node to the AV node and Purkinje fibers
- The action of the other slower route travels locally through cardiac muscle fibers
- Cardiac cells can transmit electrical impulses from cell to cell
- Skeletal muscles needs electrical message which requires a nerve
- Electrical impulse when exiting SA node will quickly travel to the AV node
- There is slightly slower conduction through the AV node
- The AV node conducts of electrical impulse from the atria to the ventricles
- AV node delay allows the atria can complete their systolic contraction before ventricular systole begins
- Simultaneous atrial and ventricular systole generates high pressure which stops blood flow from the atria into the ventricles
- Electrical impulse from the AV node travels via of the Purkinje fibers/bundle of His through ventricles
- Bundle of His fibers run down interventricular septum to apex of the right and left ventricles
- Purkinje fibers bring impulses from the bundle of His into ventricular myocardium
- Ventricular contraction will start at the heart's apex for effective ejection of blood even if the electrical impulse starts at the heart's base
- During ventricular systole, the atria are in diastole while filling with blood for the next heart contraction
- Spontaneous cardiac muscle depolarization, or an abnormal conduction system may cause arrhythmia
Cardiac Receptor Physiology
- Sympathetic nervous system physiology:
- Beta-1 receptors generate positive inotropic action (increases contractility)
- Beta-1 receptors also generate positive chronotropic effects (increases heart rate)
- Parasympathetic nervous system physiology utilizes Cholinergic receptors which produce negative chronotropic effects
- Alpha 1 receptors cause arterioles to constrict when stimulated
- Beta 2 receptors cause arterioles to dilate when stimulated
Cardiac Compensatory Mechanisms
- The system has reserves to increase output during times of need- like athletic performance
- Increased heart rate can compensate for cardiac disease up to the point where ventricular filling goes too fast
- Increasing stroke volume via increased force of contraction can increase the amount of pumped blood to a limit
- Enhanced efficiency of the heart muscle and physiologic heart enlargement are other compensatory mechanisms
- Cardiac muscle can respond to the amount of work by increasing in size and becoming stronger
Basic Cardiac Diseases
- Valvular disease is a common acquired heart disorder
- Ascites may occur if the right AV/tricuspid valve has been affected
- Pulmonary edema occurs is left AV/mitral valve has been affected
- Valvular disease can be caused by stenosis or progressive endocarditis
- Valvular disease can be associated with a murmur
- Cardiac arrhythmias can be caused by cardiac muscle depolarizing the SA node
- Rapid heart rate is defined as Tachyarrhythmia
- Slow heart rate is defined as Bradyarrhythmia
- Supraventricular arrhythmia is arrhythmia that starts in the atria
- Ventricular arrhythmia is arrhythmia that starts ventricles
- Some cardiac drugs can predispose the heart to arrhythmia
Myocardial Disease
- Cardiomyopathy refers to any disease of the cardiac muscle
- Dilative muscle becomes thin and ineffective at pumping
- Great Danes and Boxer breeds are prone to Dilative, AKA boxer cardiomyopathy
- Hypertrophic heart muscle is thickened restricting ventricular filling
- More common in cats and may be associated with hyperthyroidism
- Congenital defects, abnormal cardiac innervation, hypertension, heartworm disease can cause cardiomyopathy
- Congestive heart failure (CHF) is an end stage for many diseases
- Sodium and water end up being retained by the kidneys because the heart fails impairing its pumping ability to compensate for inadequate cardiac output
- Signs of CHF:
- Exercise intolerance
- Pulmonary edema
- Ascites
- Cyanosis
- Cardiac enlargement
Objectives for Treatment
- Controlling rhythm disturbances
- Increasing cardiac output by:
- Increasing strength of contraction
- Decreasing afterload using an Arteriolar dilator
- Decreasing preload with Venodilator
- Relieving fluid accumulation by using Diuretics and dietary salt restriction
- Increasing oxygenation of blood with Bronchodilation
- Ancillary treatment may include Narcotics/sedatives and oxygen
Positive Inotropic Drugs
- Cardiac glycosides like Digitalis
- Catecholamines like Isoproterenol, Dopamine and Dobutamine
- Bipyridine derivatives
- Inotropic/mixed dilator such as Pimobendan
Cardiac Glycoside- Digitalis
- Digoxin and digitoxin are derived from Digitalis purpurea
- Cardiac contractility is improved
- Includes increased calcium ions available for contraction
- Heart rate decreases and slows atrioventricular conduction time increasing parasympathetic stimulation
- It also has antiarrhythmic effects and decreases signs of dyspnea
- Digitalis is used in treatment of CHF, atrial fibrillation, and supraventricular tachycardia
- Adverse effects include anorexia, vomiting, diarrhea, and arrhythmia
- These drugs are narrow with their therapeutic range and drug levels affect many drugs, needing compatibility checks
Catecholamines
- Sympathomimetic compounds
- Muscle contraction force and rate increases
- Elevates blood glucose and constricts peripheral vessels to elevate blood pressure
- Acts by stimulating the beta 1 receptors
- They are short-acting and can only be used for short term management
Epinephrine
- The preferred drug for cardiac arrest, AKA adrenalin
- Not useful for chronic heart failure management
- Can use IV, intratracheal, intravenous route
- Concentration is typically 1:10,000= 0.1mg/ml or 1:1000= 1mg/ml
- The drug is light sensitive and most formulations are stored in refrigerator
Isoproterenol
- Atropine-resistant bradycardia is an indication
Dopamine
- A synthetic precursor of norepinephrine
- Dopaminergic receptors are stimulated in the coronary, renal and cerebral vascular beds
- Stimulates alpha and beta adrenergic receptors
- Heart contractility, rate, and blood pressure increases
- Dopamine is a treatment for heart failure with anesthetic emergencies, acute heart failure, oliguric renal failure, pharmacologic support of blood pressure
- Supportive shock treatment
- Adverse effects: Vomiting, tachycardia, dyspnea and variations in BP
Dobutamine
- A synthetic inotrope related to dopamine
- Cardiac contractility increases
- No dilation of select vascular beds occur and it is a Direct beta 1 adrenergic agonist
- Increases cardiac output without increased HR or arrhythmia
- Administered as an IV infusion
- Given to many anesthetized horses to support blood pressure
Bipyridine Derivatives
- Amrinone and milrinone are a new class of positive inotrope that increases cellular calcium but not often used in veterinary medicine
Inotropic, Mixed Dilator “Inolator”= Pimobendan
- Approved for use in 2007
- Positive inotrope
- Increases calcium sensitivity
- Inhibits phosphodiesterase
- The Vetmedin version is becoming a popular treatment for heart failure
- Labeled for treatment for arterioventricular insufficiency and dilated cardiomyopathy and is available as chewable tablets
- Adverse effects includes anorexia, lethargy, diarrhea
- Hypertrophic cardiomyopathy is a contraindication although has been used successfully in cats
- Aortic stenosis is a contraindication
Antiarrhythmic Drugs
- Arrhythmia that is a variation from normal rhythm may arise from an ectopic focus of cells being outside of the sinoatrial node
- Trained auscultation can find abnormality, but ECG may be required
- Potential factors predisposing heart to arrhythmia include hypoxemia, electrolyte imbalances, increased levels or sensitivity to catecholamines, drugs and/or cardiac trauma.
- May be tachyarrhythmias or bradyarrhythmias
Antiarrhythmic Drug Categories
- Drugs in Class 1A depress myocardial excitability, prolong the refractory period and treat atrial/ventricular arrhythmias
- Can be administered orally long term
- Quinidine is made from cinchona plants or quinine
- Used for ventricular arrhythmias and atrial fibrillation
- May cause anorexia, vomiting, diarrhea, weakness, and laminitis
- Primary treatment for equine A-fib
- Procainamide is chemically related to procaine
- Prescribed to treat ventricular premature contractions (VPCs)
- Maybe related to anorexia, vomiting, diarrhea, hypotension
- Drugs in Class 1B stabilize cell membranes by blocking the influx of sodium into the cell to prevent depolarization
- Lidocaine is a local anesthetic and antiarrhythmic, only available for Injectable, and is commonly recommended for emergency treatment of VPCs and V-tach in 1 and 2 % solutions
- Do not combine lidocaine with epinephrine for arrhythmia treatment
- Tocainide is available as a oral form with a similar use to lidocaine
- Mexiletine is available as a oral form with a similar use to lidocaine
Other Classes of Antiarrhythmic Drugs
- Class 1C drugs are not used in veterinary medicine
- Available meds include Flecainide and Encainide
- Class II blocks beta 1 and/or beta-2 adrenergic receptors, used in treatments of atrial/ventricular arrhythmias
- Beta blockers reduce cardiac conduction, cardiac output, and blood pressure
- Propanolol blocks beta1 and beta 2
- Decreases myocardial oxygen demand and decreases HR, BP, and cardiac output
- Hypertrophic cardiomyopathy in animals can benefit
- Can use in cats for hypertension
- May cause May cause bradycardia, hypotension, bronchospasm, or depression
- Sinus bradycardia and overt heart failure is a Contraindications
- Do not end administration of meds rapidly because hypertension and tachycardia can occur
- Atenolol is a selective beta-1 blocker and can be safer in animals prone to bronchospasm
- Is known to decreases HR, BP, CO, and myocardial oxygen demand
- Can be used for supraventricular tachyarrhythmia, VPC, hypertension, and cardiomyopathy
- May cause bradycardia, syncope, lethargy, heart failure and/or depression in older animals
- Class III is not commonly prescribed, amiodarone only in CPR for emergency treatment of ventricular arrhythmias
Calcium Channel Blockers
- Class IV meds block channels that allow calcium ions to pass trans cardiac cell membrane
- This depresses cardiac and smooth muscle contraction which depresses impulse transmission
- Verapamil has limited use in the vet field
- Used for supraventricular tachycardia, atrial fibrillation or atrial flutter
- Amlodipine is a calcium channel blocker
- Used for hypertension
- Commonly prescribed to cats who have hypertension from hyperthyroidism and chronic renal disease
- Diltiazem is a calcium channel blocker
- Given for dogs/cats battling supraventricular tachyarrhythmia
- Is commonly given for cats battling hypertrophic cardiomyopathy
Vasodilator Drugs
- Heart failure may result in decreased cardiac output, low blood pressure and overall poor perfusion
- Body responds to this outcome via stimulating the sympathetic nervous system
- Heart rate increases
- Small arteries constrict to increase blood pressure
- Renin is released by poorly perfused kidneys which activates the renin-angiotensin system
- Releases signals which convert angiotensin to angiotensin I
- Angiotensin I is converted to angiotensin-converting enzyme (ACE) which turns into angiotensin II
- Angiotensin II initiates further vasoconstriction and aldosterone release
- Aldosterone directs kidneys to reabsorb sodium and osmotic water
- Increases tissue perfusion expanding total blood volume containing water and sodium
- In the short term this is beneficial, but long term the heart has to push through constricted vessels and the increased blood which is increasingly harder
- Vasodilators dilate arteries, veins, or both
- Angiotensin I drugs may act via direct action on smooth muscles or block how Angiotensin II converts
- Improves cardiac output, preload, and dilates vessels
Vasodilator Drugs List
- Hydralazine is a arterial dilator that effects smooth muscle via calcium movement interference and contraction inhibition
- Reduces afterload and improves cardiac output in CHF and CHF especially due to mitral valve insufficiency
- Common adverse effects include vomiting, tachycardia, hypotension, diarrhea, sodium and water retention.
- Nitroglycerin Ointment is venodilator that reduces preload via lessening venous return to the heart
Angiotensin-Converting Enzyme Inhibitors (ACE Inhibitors)
- Vasodilators that prevent formation of vasoconstrictor angiotensin II
- Prevent the conversion of angiotensin I to angiotensin II
- May combine with diuretics, cardiac glycosides and pimobendan
- Treats the renin-angiotensin cycle, these meds are frequently administered
- Options includes Captopril, Enalapril, Lisinopril and Benazepril
- When combined risk of hypotension can occur
- Recommended that kidney health is re-tested along with electrolytes a few weeks after medication starts
Angiotensin II Antagonist/Angiotensin Receptor Blocker
- Can be used for animals with proteinuria
- Telmisartan is a New hypertension drug specifically prescribed to cats, and especially those that have renal secondary hypertension
- Preserves beneficial effects of angiotensin II
- Monitor for anemia at the initial stage of treatment
- Monitor for weight loss when start of treatment
- Cannot be handled by pregnant women during pregnancy due to risk associated with fetal morbidity and death
- Cannot combine with hepatic disease, safety in animals is not yet tested
Diuretics
- Prescribed in the treatment of cardiac diseases due to their ability to reduce preload through diuresis
- Reduce reabsorption of sodium and water in the tubules
- Retaining sodium means water stays within the tubules and is urinated
Loop Diuretics
- Furosemide is the most effective and common in veterinary medicine
- Assists with removing edema in CHF patients, and is commonly prescribed for rapid pulmonary edema/CHF
- Can administer (PO, IM, IV, SQ) and the sodium reabsorption happens in the loop of Henle
- Adverse effects may include weakness and also ototoxicity
- Hypokalemia may increase the risk of digitalis toxicity requiring that potassium has supplements
- Animals need open access to drink water to stay hydrated and urinate 20-30 mins post administration
Thiazides and Spironolactone
- Thiazides loop the distal tubules
- Is not commonly used, the ingredient is chlorothiazide
- Spironolactone is a potassium diuretic
- Has aldosterone antagonist- sodium reabsorption is reduced from kidneys
- May prescribe in combinations of diuretics
- Used in veterinary medicines in situations with high hyperkalemia
Helpful Care Aspects for Pets with Heart Failure
- Dietary Management is prescribed for reducing sodium, controlling weight and support digestible diets
- Have pets follow low sodium diet and avoid treats
- Owners can give oxygen
- Decreases both hypoxia and cyanosis that stem from pulmonary from edema with oxygen from face masks
- Pets prescribed anti-clotting formation is prescribed to those with hypertrophic cardiomyopathy
- Reductions of hypoventilation occur with reduce anxiety, and sedation
Thoracocentesis and Pleurocentesis
- A lifesaving method of cardiac medications assists to improve function via removal of pulmonary treatments
- Ascites removals reduces diaphragm pressure improves ventilation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.