Podcast
Questions and Answers
Which heart valve prevents backflow of blood from the left ventricle into the left atrium?
Which heart valve prevents backflow of blood from the left ventricle into the left atrium?
- Aortic valve
- Mitral valve (correct)
- Pulmonic valve
- Tricuspid valve
Deoxygenated blood enters the heart through which major blood vessel?
Deoxygenated blood enters the heart through which major blood vessel?
- Aorta
- Pulmonary artery
- Pulmonary veins
- Superior and inferior vena cavae (correct)
Which coronary artery is most commonly involved in myocardial infarctions affecting the anterior wall of the left ventricle?
Which coronary artery is most commonly involved in myocardial infarctions affecting the anterior wall of the left ventricle?
- Left anterior descending (LAD) artery (correct)
- Right coronary artery (RCA)
- Left main coronary artery
- Circumflex artery
What is the primary function of the sinoatrial (SA) node?
What is the primary function of the sinoatrial (SA) node?
Which of the following best describes the pathophysiology of atherosclerosis?
Which of the following best describes the pathophysiology of atherosclerosis?
Which condition results from a complete blockage of blood flow to a part of the heart, causing tissue damage?
Which condition results from a complete blockage of blood flow to a part of the heart, causing tissue damage?
A patient reports chest pain that is predictable and relieved by rest. What type of angina is the patient most likely experiencing?
A patient reports chest pain that is predictable and relieved by rest. What type of angina is the patient most likely experiencing?
Which of the following is a common cause of heart failure?
Which of the following is a common cause of heart failure?
What is the term for a heart rate that is abnormally fast, typically greater than 100 beats per minute?
What is the term for a heart rate that is abnormally fast, typically greater than 100 beats per minute?
What is the role of the atrioventricular (AV) node in the heart's electrical conduction system?
What is the role of the atrioventricular (AV) node in the heart's electrical conduction system?
A patient presents with shortness of breath, fatigue, and edema in the lower extremities. Which condition is most likely causing these symptoms?
A patient presents with shortness of breath, fatigue, and edema in the lower extremities. Which condition is most likely causing these symptoms?
Which diagnostic finding is most indicative of a myocardial infarction (MI)?
Which diagnostic finding is most indicative of a myocardial infarction (MI)?
A patient is diagnosed with ischemia. What does this term refer to?
A patient is diagnosed with ischemia. What does this term refer to?
Which heart valve is located between the right ventricle and the pulmonary artery?
Which heart valve is located between the right ventricle and the pulmonary artery?
What is the primary role of the coronary arteries?
What is the primary role of the coronary arteries?
A patient is diagnosed with unstable angina. Which of the following is most characteristic of this condition?
A patient is diagnosed with unstable angina. Which of the following is most characteristic of this condition?
Which of the following best describes the function of the Purkinje fibers?
Which of the following best describes the function of the Purkinje fibers?
A patient has a heart rate of 45 bpm. Which term best describes this condition?
A patient has a heart rate of 45 bpm. Which term best describes this condition?
Which of the following valves prevents backflow of blood from the aorta into the left ventricle?
Which of the following valves prevents backflow of blood from the aorta into the left ventricle?
Through which valve does blood flow when moving from the right atrium to the right ventricle?
Through which valve does blood flow when moving from the right atrium to the right ventricle?
A patient with a history of coronary artery disease (CAD) presents to the clinic. Which of the following is the most important modifiable risk factor to discuss with the patient?
A patient with a history of coronary artery disease (CAD) presents to the clinic. Which of the following is the most important modifiable risk factor to discuss with the patient?
A patient reports experiencing chest discomfort. What characteristic of their pain would be most concerning for acute myocardial ischemia?
A patient reports experiencing chest discomfort. What characteristic of their pain would be most concerning for acute myocardial ischemia?
While assessing a patient, you notice jugular venous distention (JVD). This finding is most indicative of which underlying condition?
While assessing a patient, you notice jugular venous distention (JVD). This finding is most indicative of which underlying condition?
A patient has a history of heart failure. Which symptom would most likely prompt you to suspect acute decompensation?
A patient has a history of heart failure. Which symptom would most likely prompt you to suspect acute decompensation?
You're auscultating a patient's heart sounds and hear an extra heart sound (S3). This is associated with which condition?
You're auscultating a patient's heart sounds and hear an extra heart sound (S3). This is associated with which condition?
An ECG shows an elevated ST segment. What condition is this most indicative of?
An ECG shows an elevated ST segment. What condition is this most indicative of?
While assessing a patient, you palpate a bounding pulse. Which of the following factors could contribute to this finding?
While assessing a patient, you palpate a bounding pulse. Which of the following factors could contribute to this finding?
A patient with chronic hypertension is scheduled for an echocardiogram. What is the MOST likely finding you would expect?
A patient with chronic hypertension is scheduled for an echocardiogram. What is the MOST likely finding you would expect?
Which of the following blood pressure readings would be classified as Stage 2 hypertension, according to current guidelines?
Which of the following blood pressure readings would be classified as Stage 2 hypertension, according to current guidelines?
During a physical examination, where is the point of maximal impulse (PMI) typically located in a healthy adult?
During a physical examination, where is the point of maximal impulse (PMI) typically located in a healthy adult?
A patient reports paroxysmal nocturnal dyspnea (PND). Which explanation best describes this symptom?
A patient reports paroxysmal nocturnal dyspnea (PND). Which explanation best describes this symptom?
What heart sound is often associated with mitral valve stenosis?
What heart sound is often associated with mitral valve stenosis?
A patient develops a deep vein thrombosis (DVT) in their leg. If the thrombus dislodges and travels to the lungs, what is the MOST likely resulting condition?
A patient develops a deep vein thrombosis (DVT) in their leg. If the thrombus dislodges and travels to the lungs, what is the MOST likely resulting condition?
Which of the following findings would be MOST suggestive of peripheral artery disease (PAD) in a patient's lower extremities?
Which of the following findings would be MOST suggestive of peripheral artery disease (PAD) in a patient's lower extremities?
During a focused cardiac assessment, what is the primary purpose of palpating the carotid arteries?
During a focused cardiac assessment, what is the primary purpose of palpating the carotid arteries?
A provider orders troponin levels for a patient. What condition is the provider MOST likely evaluating?
A provider orders troponin levels for a patient. What condition is the provider MOST likely evaluating?
A patient's ECG shows a prolonged PR interval. What does this indicate?
A patient's ECG shows a prolonged PR interval. What does this indicate?
Which of the following physical exam findings is MOST indicative of chronic venous insufficiency?
Which of the following physical exam findings is MOST indicative of chronic venous insufficiency?
You osculate a patient with a harsh, blowing sound over the carotid artery. How whould you document this sound?
You osculate a patient with a harsh, blowing sound over the carotid artery. How whould you document this sound?
A patient is scheduled for an ankle-brachial index (ABI) test. What condition is the test assessing? (Select all that apply)
A patient is scheduled for an ankle-brachial index (ABI) test. What condition is the test assessing? (Select all that apply)
A patient is complaining of claudication. What is the MOST reasonable action to take?
A patient is complaining of claudication. What is the MOST reasonable action to take?
Which one of these characteristics helps differentiate between PAD and venous insufficiency?
Which one of these characteristics helps differentiate between PAD and venous insufficiency?
Which of the patient statements indicates the patient has orthopnea?
Which of the patient statements indicates the patient has orthopnea?
Flashcards
Coronary Artery Disease (CAD)
Coronary Artery Disease (CAD)
Primary cause of most cardiac-related issues.
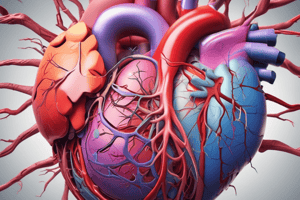
Heart
Heart
Four-chambered muscular organ responsible for pumping blood throughout the body.
Atria (Right and Left)
Atria (Right and Left)
Two upper chambers of the heart that receive blood.
Ventricles (Right and Left)
Ventricles (Right and Left)
Signup and view all the flashcards
Right Atrium
Right Atrium
Signup and view all the flashcards
Right Ventricle
Right Ventricle
Signup and view all the flashcards
Left Atrium
Left Atrium
Signup and view all the flashcards
Left Ventricle
Left Ventricle
Signup and view all the flashcards
Valves
Valves
Signup and view all the flashcards
Tricuspid Valve
Tricuspid Valve
Signup and view all the flashcards
Pulmonic Valve
Pulmonic Valve
Signup and view all the flashcards
Mitral (Bicuspid) Valve
Mitral (Bicuspid) Valve
Signup and view all the flashcards
Aortic Valve
Aortic Valve
Signup and view all the flashcards
Coronary Arteries
Coronary Arteries
Signup and view all the flashcards
Main Coronary Arteries
Main Coronary Arteries
Signup and view all the flashcards
Electrical Conduction System
Electrical Conduction System
Signup and view all the flashcards
Sinoatrial (SA) Node
Sinoatrial (SA) Node
Signup and view all the flashcards
Atrioventricular (AV) Node
Atrioventricular (AV) Node
Signup and view all the flashcards
Bundle of His
Bundle of His
Signup and view all the flashcards
Left and Right Bundle Branches
Left and Right Bundle Branches
Signup and view all the flashcards
Purkinje Fibers
Purkinje Fibers
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
Ischemia
Ischemia
Signup and view all the flashcards
Myocardial Infarction (MI)
Myocardial Infarction (MI)
Signup and view all the flashcards
Angina Pectoris
Angina Pectoris
Signup and view all the flashcards
Stable Angina
Stable Angina
Signup and view all the flashcards
Unstable Angina
Unstable Angina
Signup and view all the flashcards
Heart Failure
Heart Failure
Signup and view all the flashcards
Arrhythmias
Arrhythmias
Signup and view all the flashcards
Study Notes
- Coronary artery disease (CAD) is the primary cause of most cardiac-related issues
Cardiac Anatomy
- The heart is a four-chambered muscular organ responsible for pumping blood throughout the body
- The heart consists of two atria (right and left) and two ventricles (right and left)
- The atria receive blood, while the ventricles pump blood out of the heart
- The right atrium receives deoxygenated blood from the body via the superior and inferior vena cavae
- The right ventricle pumps deoxygenated blood to the lungs via the pulmonary artery
- The left atrium receives oxygenated blood from the lungs via the pulmonary veins
- The left ventricle pumps oxygenated blood to the body via the aorta
- Valves ensure unidirectional blood flow through the heart:
- Tricuspid valve: between the right atrium and right ventricle
- Pulmonic valve: between the right ventricle and pulmonary artery
- Mitral (bicuspid) valve: between the left atrium and left ventricle
- Aortic valve: between the left ventricle and aorta
- The coronary arteries supply the heart muscle with oxygenated blood
- The main coronary arteries are the left main, left anterior descending (LAD), circumflex, and right coronary artery (RCA)
- The heart's electrical conduction system controls heart rate and rhythm
- Sinoatrial (SA) node: the heart's primary pacemaker, located in the right atrium
- Atrioventricular (AV) node: delays the electrical impulse, allowing the atria to contract before the ventricles
- Bundle of His: conducts the impulse from the AV node to the ventricles
- Left and right bundle branches: conduct the impulse through the ventricles
- Purkinje fibers: distribute the impulse throughout the ventricular myocardium, causing contraction
Cardiac Pathophysiology
- Atherosclerosis: plaque buildup inside the arteries, leading to narrowing and reduced blood flow
- Can lead to angina (chest pain) or myocardial infarction (heart attack) if a coronary artery is affected
- Ischemia: insufficient blood supply to the heart muscle, often due to CAD
- Prolonged ischemia can lead to tissue damage or death (infarction)
- Myocardial Infarction (MI): occurs when blood flow to a part of the heart is completely blocked, causing tissue damage
- Commonly caused by a thrombus (blood clot) forming on a ruptured atherosclerotic plaque
- Diagnosed by ECG changes and elevated cardiac biomarkers (e.g., troponin) in the blood
- Angina Pectoris: chest pain caused by temporary myocardial ischemia
- Stable angina: predictable and relieved by rest or nitroglycerin
- Unstable angina: unpredictable and may occur at rest; a sign of worsening CAD
- Heart Failure: the heart's inability to pump enough blood to meet the body's needs
- Can result from various conditions, including MI, hypertension, and valve disorders
- Leads to fluid retention, shortness of breath, and fatigue
- Arrhythmias: abnormal heart rhythms caused by disturbances in the heart's electrical conduction system
- Tachycardia: heart rate too fast (usually >100 bpm)
- Bradycardia: heart rate too slow (usually <60 bpm)
- Atrial fibrillation: rapid, irregular atrial contractions
- Ventricular tachycardia: rapid, life-threatening ventricular contractions
- Ventricular fibrillation: disorganized, ineffective ventricular contractions; leads to cardiac arrest
- Cardiomyopathy: disease of the heart muscle, making it harder for the heart to pump blood
- Dilated cardiomyopathy: enlarged heart with weakened pumping ability
- Hypertrophic cardiomyopathy: thickened heart muscle, which can obstruct blood flow
- Restrictive cardiomyopathy: stiff heart muscle, limiting its ability to fill with blood
- Valvular Heart Disease: conditions affecting the heart valves, disrupting blood flow
- Stenosis: narrowing of a valve, restricting blood flow
- Regurgitation (insufficiency): leakage of blood backward through a valve
- Hypertensive Heart Disease: heart problems caused by long-term high blood pressure
- Can lead to left ventricular hypertrophy, heart failure, and increased risk of arrhythmias
- Congenital Heart Defects: structural abnormalities of the heart present at birth
- Examples include ventricular septal defect (VSD), atrial septal defect (ASD), and tetralogy of Fallot
- Cardiac Tamponade: compression of the heart caused by fluid accumulation in the pericardial sac
- Restricts the heart's ability to fill with blood, leading to decreased cardiac output
- Beck's triad (hypotension, muffled heart sounds, and jugular venous distension) is a classic sign
- Pericarditis: inflammation of the pericardium (the sac surrounding the heart)
- Causes chest pain that may worsen with breathing or lying down
Patient Assessment
- Gather a thorough history, including:
- Chief complaint
- History of present illness (HPI)
- Past medical history (PMH)
- Medications
- Allergies
- Social history (smoking, alcohol, drug use)
- Family history (cardiac disease, hypertension, diabetes)
- Key questions to ask:
- "Can you describe your chest pain?" (location, intensity, duration, quality, radiation)
- "What makes the pain better or worse?"
- "Do you have any other symptoms, such as shortness of breath, nausea, vomiting, sweating, or dizziness?"
- "Do you have a history of heart problems?"
- Vital Signs:
- Heart rate (HR)
- Blood pressure (BP)
- Respiratory rate (RR)
- Oxygen saturation (SpO2)
- Temperature
- Assess level of consciousness (LOC) and mental status
- Cardiac-Specific Assessment:
- Auscultate heart sounds (normal S1 and S2, extra sounds like S3 or S4, murmurs)
- Auscultate lung sounds (clear, wheezes, crackles)
- Palpate pulses (rate, rhythm, strength)
- Observe for signs of fluid retention (edema in extremities, jugular venous distension)
- Examine skin color and temperature (pale, cool, diaphoretic)
- 12-Lead ECG:
- Essential for identifying cardiac arrhythmias, ischemia, and infarction
- Placement of electrodes:
- V1: 4th intercostal space, right sternal border
- V2: 4th intercostal space, left sternal border
- V4: 5th intercostal space, midclavicular line
- V3: Midway between V2 and V4
- V5: 5th intercostal space, anterior axillary line
- V6: 5th intercostal space, mid-axillary line
- Limb leads: RA, LA, RL, LL (placed on the limbs)
- Analyze the ECG for:
- Heart rate and rhythm
- P waves (atrial depolarization)
- QRS complexes (ventricular depolarization)
- T waves (ventricular repolarization)
- ST segment (elevation or depression indicates ischemia/infarction)
- PR interval (time from atrial to ventricular depolarization)
- QT interval (total time for ventricular depolarization and repolarization)
- Blood Glucose:
- Check blood glucose level, especially in patients with altered mental status or suspected diabetes
- Capnography (ETCO2):
- Can provide information about ventilation and perfusion
- Continuous Monitoring:
- Continuously monitor ECG, vital signs, and SpO2
- SAMPLE History:
- Signs and Symptoms
- Allergies
- Medications
- Pertinent Past History
- Last Oral Intake
- Events Leading to the Incident
- OPQRST for Pain Assessment:
- Onset
- Provocation/Palliation
- Quality
- Region/Radiation
- Severity
- Timing
- Physical Exam Techniques:
- Inspection: Look for visible signs of distress, such as cyanosis, diaphoresis, or difficulty breathing.
- Palpation: Check for pulses, edema, and tenderness.
- Auscultation: Listen to heart and lung sounds for abnormalities.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.