Podcast
Questions and Answers
What condition is primarily described as the heart's inability to contract effectively, leading to poor chamber emptying?
What condition is primarily described as the heart's inability to contract effectively, leading to poor chamber emptying?
- Valvular regurgitation
- Systolic dysfunction (correct)
- Diastolic dysfunction
- Arrhythmia
Which anatomical change is associated with aging and contributes to reduced filling of the heart?
Which anatomical change is associated with aging and contributes to reduced filling of the heart?
- Enlargement of the left ventricular cavity
- Thickening of the basal ventricular septum
- Increased blood viscosity
- Reduction of myocytes (correct)
What is a major consequence of left ventricular outflow obstruction due to aging?
What is a major consequence of left ventricular outflow obstruction due to aging?
- Improved cardiac output
- Decreased connective tissue
- Overworked myocardium (correct)
- Increased chance of myocardial infarction
Which condition is characterized by the deposition of extracellular amyloid in older hearts?
Which condition is characterized by the deposition of extracellular amyloid in older hearts?
What type of dysfunction results when the myocardium cannot relax sufficiently to allow for ventricular filling?
What type of dysfunction results when the myocardium cannot relax sufficiently to allow for ventricular filling?
Which of the following is NOT typically associated with cardiac aging changes?
Which of the following is NOT typically associated with cardiac aging changes?
What type of cardiac disorder can lead to left ventricular overwork due to backward blood flow?
What type of cardiac disorder can lead to left ventricular overwork due to backward blood flow?
What is the typical biochemical consequence of myocardial ischemia shortly after its onset?
What is the typical biochemical consequence of myocardial ischemia shortly after its onset?
What evidence of coronary thrombosis is typically found when angiography is performed shortly after the onset of myocardial ischemia?
What evidence of coronary thrombosis is typically found when angiography is performed shortly after the onset of myocardial ischemia?
What might occur in the absence of intervention during myocardial ischemia within 12 to 24 hours?
What might occur in the absence of intervention during myocardial ischemia within 12 to 24 hours?
Which of the following factors is not associated with the early success of thrombolysis and/or angioplasty in managing ischemia?
Which of the following factors is not associated with the early success of thrombolysis and/or angioplasty in managing ischemia?
What is the significance of myocardial contractility cessation within a minute after the onset of ischemia?
What is the significance of myocardial contractility cessation within a minute after the onset of ischemia?
What is characterized by new sarcomeres being assembled in series within existing sarcomeres?
What is characterized by new sarcomeres being assembled in series within existing sarcomeres?
Which mechanism maintains arterial pressure when cardiac function is compromised?
Which mechanism maintains arterial pressure when cardiac function is compromised?
In pressure-overload hypertrophy, how are new sarcomeres predominantly assembled?
In pressure-overload hypertrophy, how are new sarcomeres predominantly assembled?
Which of the following conditions is NOT associated with acute hemodynamic stress?
Which of the following conditions is NOT associated with acute hemodynamic stress?
What primarily increases in response to dilation due to volume overload?
What primarily increases in response to dilation due to volume overload?
What role does norepinephrine play in heart function during overload conditions?
What role does norepinephrine play in heart function during overload conditions?
Which of the following is a feature of volume-overload hypertrophy?
Which of the following is a feature of volume-overload hypertrophy?
Which physiological mechanism is involved in regulating filling volumes and pressures in heart dysfunction?
Which physiological mechanism is involved in regulating filling volumes and pressures in heart dysfunction?
What is the consequence of chronic work overload on myocytes?
What is the consequence of chronic work overload on myocytes?
What is the primary effect of activating the renin-angiotensin-aldosterone system?
What is the primary effect of activating the renin-angiotensin-aldosterone system?
In patients with systemic hypertension, what is the typical change in heart weight?
In patients with systemic hypertension, what is the typical change in heart weight?
How does atrial natriuretic peptide counteract the renin-angiotensin-aldosterone system?
How does atrial natriuretic peptide counteract the renin-angiotensin-aldosterone system?
What is the significant morphological change observed in myocyte hypertrophy?
What is the significant morphological change observed in myocyte hypertrophy?
Which condition is least likely to directly cause dramatic cardiac hypertrophy?
Which condition is least likely to directly cause dramatic cardiac hypertrophy?
What type of hypertrophy is primarily associated with left ventricular outflow obstruction?
What type of hypertrophy is primarily associated with left ventricular outflow obstruction?
Which aspect best describes heart failure in relation to cardiac hypertrophy?
Which aspect best describes heart failure in relation to cardiac hypertrophy?
What key physiological change occurs at the tissue level during heart failure?
What key physiological change occurs at the tissue level during heart failure?
Which of the following types of heart conditions does NOT typically lead to significant left ventricular hypertrophy?
Which of the following types of heart conditions does NOT typically lead to significant left ventricular hypertrophy?
Which imaging technique is commonly used to observe ventricular hypertrophy?
Which imaging technique is commonly used to observe ventricular hypertrophy?
What is the main difference between stable angina and unstable angina?
What is the main difference between stable angina and unstable angina?
Which statement about myocardial infarction (MI) is true?
Which statement about myocardial infarction (MI) is true?
What is the primary underlying cause of ischemic heart disease (IHD)?
What is the primary underlying cause of ischemic heart disease (IHD)?
How does the frequency of myocardial infarction (MI) change with age?
How does the frequency of myocardial infarction (MI) change with age?
What factor is generally associated with an increased risk of myocardial infarction in men?
What factor is generally associated with an increased risk of myocardial infarction in men?
What could cause sudden cardiac death related to myocardial ischemia?
What could cause sudden cardiac death related to myocardial ischemia?
At what age does the risk of ischemic heart disease (IHD) typically begin to increase significantly?
At what age does the risk of ischemic heart disease (IHD) typically begin to increase significantly?
What role does estrogen play in the risk for ischemic heart disease in women?
What role does estrogen play in the risk for ischemic heart disease in women?
What type of changes can lead to unstable angina?
What type of changes can lead to unstable angina?
What is likely to happen to blood flow in the presence of disrupted plaques in coronary arteries?
What is likely to happen to blood flow in the presence of disrupted plaques in coronary arteries?
Flashcards
Systolic Dysfunction
Systolic Dysfunction
The heart muscle (myocardium) weakens and the heart chambers cannot empty properly, resulting in reduced pumping efficiency.
Diastolic Dysfunction
Diastolic Dysfunction
The heart muscle cannot relax sufficiently to allow for proper filling of the ventricles, affecting the heart's ability to fill with blood during diastole.
Aging Changes in the Heart
Aging Changes in the Heart
Age-related changes in the heart include a decrease in the size of the left ventricle and a decrease in the number of heart muscle cells.
Amyloid Deposition in the Heart
Amyloid Deposition in the Heart
Signup and view all the flashcards
Valvular Heart Disease
Valvular Heart Disease
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
Cardiac Conduction Disorders
Cardiac Conduction Disorders
Signup and view all the flashcards
Frank-Starling Mechanism
Frank-Starling Mechanism
Signup and view all the flashcards
Cardiac Hypertrophy
Cardiac Hypertrophy
Signup and view all the flashcards
Cardiac Dilation
Cardiac Dilation
Signup and view all the flashcards
Concentric Hypertrophy
Concentric Hypertrophy
Signup and view all the flashcards
Eccentric Hypertrophy
Eccentric Hypertrophy
Signup and view all the flashcards
Neurohumoral System Activation
Neurohumoral System Activation
Signup and view all the flashcards
Congestive Heart Failure (CHF)
Congestive Heart Failure (CHF)
Signup and view all the flashcards
Pressure Overload
Pressure Overload
Signup and view all the flashcards
Volume Overload
Volume Overload
Signup and view all the flashcards
Myocyte Hypertrophy
Myocyte Hypertrophy
Signup and view all the flashcards
Renin-Angiotensin-Aldosterone System (RAAS)
Renin-Angiotensin-Aldosterone System (RAAS)
Signup and view all the flashcards
Atrial Natriuretic Peptide (ANP)
Atrial Natriuretic Peptide (ANP)
Signup and view all the flashcards
Vascular Resistance
Vascular Resistance
Signup and view all the flashcards
Pressure Hypertrophy
Pressure Hypertrophy
Signup and view all the flashcards
Pressure Hypertrophy with Dilation
Pressure Hypertrophy with Dilation
Signup and view all the flashcards
Causes of Cardiac Hypertrophy
Causes of Cardiac Hypertrophy
Signup and view all the flashcards
Dilation
Dilation
Signup and view all the flashcards
What is Myocardial Ischemia?
What is Myocardial Ischemia?
Signup and view all the flashcards
What is Stable Angina?
What is Stable Angina?
Signup and view all the flashcards
What is Unstable Angina?
What is Unstable Angina?
Signup and view all the flashcards
What is a Myocardial Infarction (heart attack)?
What is a Myocardial Infarction (heart attack)?
Signup and view all the flashcards
What is Sudden Cardiac Death?
What is Sudden Cardiac Death?
Signup and view all the flashcards
What is the main cause of Coronary Artery Disease (CAD)?
What is the main cause of Coronary Artery Disease (CAD)?
Signup and view all the flashcards
How does age affect heart attacks?
How does age affect heart attacks?
Signup and view all the flashcards
How does gender affect heart attacks?
How does gender affect heart attacks?
Signup and view all the flashcards
Who is most vulnerable to coronary artery disease (CAD)?
Who is most vulnerable to coronary artery disease (CAD)?
Signup and view all the flashcards
What are the causes of myocardial ischemia?
What are the causes of myocardial ischemia?
Signup and view all the flashcards
Myocardial Ischemia's Impact on Contractility
Myocardial Ischemia's Impact on Contractility
Signup and view all the flashcards
Myocardial Ischemia: Cause and Effect
Myocardial Ischemia: Cause and Effect
Signup and view all the flashcards
Ischemia Severity and Duration
Ischemia Severity and Duration
Signup and view all the flashcards
Lactic Acid in Ischemia
Lactic Acid in Ischemia
Signup and view all the flashcards
Importance of Early Intervention
Importance of Early Intervention
Signup and view all the flashcards
Study Notes
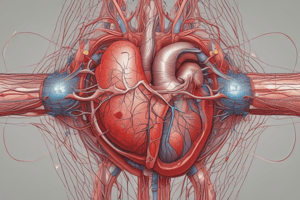
Blood Vessels
- Heart weight varies with body habitus, averaging approximately 0.4% to 0.5% of body weight (250 to 320 g in the average adult female and 300 to 360 g in the average adult male).
- Increased heart weight or ventricular thickness indicates hypertrophy. An enlarged chamber size implies dilation. Both reflect compensatory changes in response to volume and/or pressure overloads.
- Increased cardiac weight or size (or both) is called cardiomegaly.
- Cardiac myocytes (the myocardium) are responsible for the heart's pumping function.
- Left ventricular myocytes are arranged in a spiral circumferential orientation.
- Right ventricular myocytes have a less structured organization.
- Both atrial and ventricular myocytes contain protein hormones that promote arterial vasodilation and stimulate renal salt and water elimination (natriuresis and diuresis).
Cardiac Structure and Specializations
- Valvular function depends on the mobility, pliability, and structural integrity of the leaflets.
- The four cardiac valves are tricuspid, pulmonary, mitral, and aortic.
- Dilation of the aortic root can lead to valvular regurgitation.
- Mitral valve insufficiency can arise from dilatation, rupture of chordae tendineae, or papillary muscle dysfunction.
- Cardiac valves are lined by endothelium.
- Fibrosa, spongiosa, and ventricularis (or atrialis) are the three layers of cardiac valves.
Cardiac Development
- The heart and vasculature are the first fully functional organ system in utero, at roughly 8 weeks gestation.
- Without a vascular supply and a beating heart, further development cannot occur and fetal demise is inevitable.
- Cardiovascular disease is the number-one cause of worldwide mortality.
- In the US, cardiovascular disease accounts for 1 in 4 deaths (about 610,000 annually), and are more than all forms of cancer combined.
Overview of Cardiac Pathophysiology
- Heart failure (CHF) is a progressive condition with a poor prognosis.
- Each year in the US, CHF affects over 5 million people (approximately 2% of the population).
- Roughly half of CHF patients die within five years of diagnosis.
- Heart failure is characterized by inability to pump blood adequately, leading to elevated filling pressures.
- CHF arises from chronic work overload or IHD (e.g., after an myocardial infarction – MI).
Ischemic Heart Disease (IHD)
- IHD represents an imbalance between myocardial supply and demand.
- It is frequently referred to as coronary artery disease (CAD).
- IHD is frequently initiated by obstructive atherosclerotic lesions in epicardial coronary arteries.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.