Podcast
Questions and Answers
Which translocation is most characteristically associated with Burkitt lymphoma?
Which translocation is most characteristically associated with Burkitt lymphoma?
- t(11;14)(q13;q32)
- t(9;22)(q34;q11)
- t(8;14)(q24;q32) (correct)
- t(14;18)(q32;q21)
What is the typical appearance observed in Burkitt Lymphoma (BL) due to its rapid cell turnover and apoptosis?
What is the typical appearance observed in Burkitt Lymphoma (BL) due to its rapid cell turnover and apoptosis?
- Starry sky appearance (correct)
- Cobblestone pattern
- Mosaic pattern
- Swiss cheese pattern
A 35-year-old patient is diagnosed with sporadic Burkitt lymphoma. Which clinical presentation aligns with this diagnosis?
A 35-year-old patient is diagnosed with sporadic Burkitt lymphoma. Which clinical presentation aligns with this diagnosis?
- Mediastinal mass with pleural effusion and respiratory distress.
- Jaw tumor with >90% EBV association.
- Abdominal mass, often with ascites, and approximately 20% EBV association. (correct)
- Predominant organ and nodal involvement with 30-40% EBV association.
Which statement accurately reflects the impact of CNS involvement in Burkitt lymphoma (BL)?
Which statement accurately reflects the impact of CNS involvement in Burkitt lymphoma (BL)?
In the Murphy staging system for Burkitt lymphoma, which criterion defines Stage IV?
In the Murphy staging system for Burkitt lymphoma, which criterion defines Stage IV?
Which of the following is a critical consideration in treating HIV-positive patients with Burkitt lymphoma (BL) in the highly active antiretroviral therapy (HAART) era?
Which of the following is a critical consideration in treating HIV-positive patients with Burkitt lymphoma (BL) in the highly active antiretroviral therapy (HAART) era?
Why is the risk of tumor lysis syndrome (TLS) particularly high in patients with Burkitt lymphoma (BL)?
Why is the risk of tumor lysis syndrome (TLS) particularly high in patients with Burkitt lymphoma (BL)?
How does age at presentation primarily influence the overall survival (OS) in Burkitt lymphoma?
How does age at presentation primarily influence the overall survival (OS) in Burkitt lymphoma?
What is the significance of ID3 mutations in the pathogenesis of Burkitt lymphoma?
What is the significance of ID3 mutations in the pathogenesis of Burkitt lymphoma?
What is the primary rationale for employing a dose-intense, short-duration treatment strategy in patients with Burkitt lymphoma?
What is the primary rationale for employing a dose-intense, short-duration treatment strategy in patients with Burkitt lymphoma?
Which of the following best describes the role and timing of relapses in Burkitt lymphoma?
Which of the following best describes the role and timing of relapses in Burkitt lymphoma?
Which of the following distinguishes endemic Burkitt lymphoma in Sub-Saharan Africa from other variants regarding etiology?
Which of the following distinguishes endemic Burkitt lymphoma in Sub-Saharan Africa from other variants regarding etiology?
What is the significance of serum lactic acid dehydrogenase (LDH) levels in Burkitt lymphoma?
What is the significance of serum lactic acid dehydrogenase (LDH) levels in Burkitt lymphoma?
Which statement reflects the role of allopurinol or rasburicase in the management of Burkitt lymphoma?
Which statement reflects the role of allopurinol or rasburicase in the management of Burkitt lymphoma?
A patient’s Burkitt lymphoma cells test negative for CD5 and CD23. What implications does this have in understanding the cell lineage and behavior in Burkitt Lymphoma (BL)?
A patient’s Burkitt lymphoma cells test negative for CD5 and CD23. What implications does this have in understanding the cell lineage and behavior in Burkitt Lymphoma (BL)?
What would be the primary immunophenotypic markers expressed in Burkitt lymphoma cells?
What would be the primary immunophenotypic markers expressed in Burkitt lymphoma cells?
How does intrathecal chemotherapy play a vital role in the treatment of Burkitt Lymphoma (BL)?
How does intrathecal chemotherapy play a vital role in the treatment of Burkitt Lymphoma (BL)?
How does "Burkitt-like lymphoma with 11q aberration” differ from classical Burkitt lymphoma, and what implications does this have for diagnosis?
How does "Burkitt-like lymphoma with 11q aberration” differ from classical Burkitt lymphoma, and what implications does this have for diagnosis?
Which cellular characteristic distinguishes Burkitt lymphoma from other lymphomas when examining bone marrow involvement?
Which cellular characteristic distinguishes Burkitt lymphoma from other lymphomas when examining bone marrow involvement?
How do MYC and TP53 mutations cooperate to drive lymphomagenesis in Burkitt lymphoma?
How do MYC and TP53 mutations cooperate to drive lymphomagenesis in Burkitt lymphoma?
In distinguishing between the clinical features of endemic and sporadic Burkitt lymphoma, which factor is most critical?
In distinguishing between the clinical features of endemic and sporadic Burkitt lymphoma, which factor is most critical?
How does the chromosomal translocation t(8;14)(q24;q32) lead to oncogenesis in Burkitt lymphoma?
How does the chromosomal translocation t(8;14)(q24;q32) lead to oncogenesis in Burkitt lymphoma?
Which feature would be most suggestive of Burkitt lymphoma rather than diffuse large B-cell lymphoma (DLBCL) based on morphology?
Which feature would be most suggestive of Burkitt lymphoma rather than diffuse large B-cell lymphoma (DLBCL) based on morphology?
Why is the addition of granulocyte colony-stimulating factors (G-CSF) necessary in the treatment regimens for Burkitt lymphoma?
Why is the addition of granulocyte colony-stimulating factors (G-CSF) necessary in the treatment regimens for Burkitt lymphoma?
What biological consequence determines that Burkitt lymphomas are among the fastest-growing human tumors?
What biological consequence determines that Burkitt lymphomas are among the fastest-growing human tumors?
Which factor primarily dictates the consideration between using allopurinol vs. rasburicase for management of tumor lysis syndrome (TLS) in cancer treatment, and how does it influence the specific context of Burkitt lymphoma management?
Which factor primarily dictates the consideration between using allopurinol vs. rasburicase for management of tumor lysis syndrome (TLS) in cancer treatment, and how does it influence the specific context of Burkitt lymphoma management?
How might novel activating mutations in CCND3 (encoding cyclin D3) in Burkitt Lymphoma impact cellular processes?
How might novel activating mutations in CCND3 (encoding cyclin D3) in Burkitt Lymphoma impact cellular processes?
What is the crucial role of continuous veno-venous hemofiltration (CVVH) in managing patients undergoing intensive chemotherapy for Burkitt lymphoma?
What is the crucial role of continuous veno-venous hemofiltration (CVVH) in managing patients undergoing intensive chemotherapy for Burkitt lymphoma?
What is the primary rationale behind utilizing rituximab in combination chemotherapeutic programs for treating Burkitt lymphoma (BL)?
What is the primary rationale behind utilizing rituximab in combination chemotherapeutic programs for treating Burkitt lymphoma (BL)?
Flashcards
Burkitt Lymphoma (BL)
Burkitt Lymphoma (BL)
A highly aggressive mature B-cell lymphoma, representing 30-50% of pediatric lymphomas.
Clinical Variants of BL
Clinical Variants of BL
Endemic, sporadic, and immunodeficiency-associated.
Endemic Burkitt Lymphoma
Endemic Burkitt Lymphoma
Most common pediatric malignancy in sub-Saharan Africa, with a median age of 4-7 years and 95% EBV association.
Sporadic Burkitt Lymphoma
Sporadic Burkitt Lymphoma
Signup and view all the flashcards
Immunodeficiency-associated BL
Immunodeficiency-associated BL
Signup and view all the flashcards
Etiology of Burkitt Lymphoma
Etiology of Burkitt Lymphoma
Signup and view all the flashcards
Pathology of Burkitt Lymphoma
Pathology of Burkitt Lymphoma
Signup and view all the flashcards
Lab Features of Burkitt Lymphoma
Lab Features of Burkitt Lymphoma
Signup and view all the flashcards
Treatment strategy
Treatment strategy
Signup and view all the flashcards
Murphy Stage I BL
Murphy Stage I BL
Signup and view all the flashcards
Murphy Stage II Burkitt Lymphoma
Murphy Stage II Burkitt Lymphoma
Signup and view all the flashcards
Murphy Stage III BL
Murphy Stage III BL
Signup and view all the flashcards
Murphy Stage IV BL
Murphy Stage IV BL
Signup and view all the flashcards
Common Chemotherapeutic Agents for BL
Common Chemotherapeutic Agents for BL
Signup and view all the flashcards
Risk of Tumor Lysis Syndrome (TLS)
Risk of Tumor Lysis Syndrome (TLS)
Signup and view all the flashcards
Management of Tumor Lysis Syndrome (TLS)
Management of Tumor Lysis Syndrome (TLS)
Signup and view all the flashcards
c-MYC in Burkitt Lymphoma
c-MYC in Burkitt Lymphoma
Signup and view all the flashcards
Burkitt-like lymphoma
Burkitt-like lymphoma
Signup and view all the flashcards
Burkitt lymphoma Immunophenotype
Burkitt lymphoma Immunophenotype
Signup and view all the flashcards
Study Notes
Introduction to Burkitt Lymphoma
- Highly aggressive mature B-cell lymphoma (non-Hodgkin's).
- Accounts for less than 2% of all NHL diagnoses in the UK.
- Most frequent B-cell lymphoma in children, representing 30–50% of pediatric lymphomas.
- Three clinical variants: endemic, sporadic, and immunodeficiency-associated.
Types of Burkitt Lymphoma
- Endemic BL: Most common pediatric malignancy in sub-Saharan Africa, predominantly in equatorial Africa and Papua New Guinea.
- Median age of 4-7 years.
- Epstein-Barr virus (EBV) association about 95%.
- Presents characteristically as a jaw or facial bone tumor.
- Sporadic BL: More commonly seen in pediatric patients (20-30% of lymphomas), rare in adults (~1% of NHL cases in the US).
- Is distributed worldwide
- Median age of 30 years.
- EBV association in 20% of cases.
- Occurs predominantly as an abdominal mass in ~65% of cases, often with ascites.
- Immunodeficiency-associated BL: Linked to immunodeficiency, such as HIV or post-organ transplant scenarios with inherited immune deficiencies.
- Associated with the AIDS epidemic.
- Median age of 10-19 years
- EBV association of 30-40%.
- Manifests with organ and nodal involvement.
Etiology
- Idiopathic
- EBV
- Malaria (especially endemic type)
- HIV
- Chromosomal abnormalities: t(8,14), t(8,2), t(8,22).
- Oncogene involvement includes c-myc, TP53, CCND3, and TCF3 aberrations.
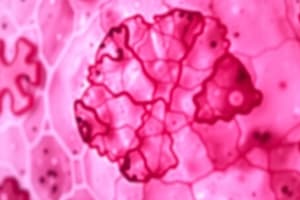
Pathology
- Displays a diffuse, monomorphic population of medium-sized cells featuring:
- Round nuclei
- Multiple nucleoli
- Prominent vacuoles
- Basophilic cytoplasm, effacing normal nodal architecture.
- High rate of spontaneous apoptosis, creating a characteristic "starry sky" appearance.
- Burkitt lymphoma cells are mature B cells typically expressing CD19, CD20, CD22, CD79a, BCL6, BCL10, and surface IgM.
- BL cells lack expression of CD5 or CD23, Mum-1, and terminal deoxynucleotidyl transferase (TdT).
Laboratory Features
- Patients with bulky disease show BL cells in marrow and blood, coupled with suppressed normal blood counts.
- Marrow involvement is characteristically extensive.
- Burkitt-type lymphoblasts with very high nuclear:cytoplasmic ratio.
- Deep blue rim of cytoplasm.
- Frequent prominent cellular vacuolization.
- Rare cases, often in males, present primarily with marrow and blood involvement, termed Burkitt cell leukemia.
- Serum lactic acid dehydrogenase is frequently elevated, reflecting the high cell turnover, particularly in patients with bulky disease.
CNS Involvement
- Is a poor prognostic factor in BL.
- High risk of CNS involvement
- Up to 20% of patients presenting with CNS involvement at diagnosis
- Leptomeningeal involvement more common than parenchymal disease.
- Without prophylaxis, 30-50% develop CNS disease.
- CNS involvement correlates with poorer outcomes.
Diagnosis of High-Grade Lymphoma
- Diagnosis is based on a combination of clinical features, histological findings, and molecular confirmation.
- Key Translocations:
- t(8;14)(q24;q32): Involves c-MYC and IgH, accounting for 100% of cases with these translocations.
- t(8;2)(p11/q24): Involves c-MYC and Igκ.
- t(8;22)(q24; q11): Involves c-MYC and Igλ,.
- All three result in cell proliferation, differentiation, and apoptosis alteration.
- IG-MYC translocation is thought to occur early in lymphomagenesis.
- Subsequent MYC and TP53 mutations occur in approximately 60% and 40% of BL cases.
- Recent studies show novel activating mutations in TCF3 and inactivating mutations in ID3 (negative regulator), affecting up to 70% of cases.
- Activating mutations in CCND3 (encoding cyclin D3) found in 38% of sporadic BL cases.
- Recurrent oncogenic mutations cooperate with MYC to promote proliferation, survival, and growth of BL cells.
- An aggressive lymphoma type, lacking MYC gene rearrangement.
- Morphologically and immunophenotypically similar to BL.
- With recurrent gains/losses of chromosome 11.
- Recognized in the WHO 2022 classification (5th edition).
- Provisionally named "Burkitt-like lymphoma with 11q aberration".
Murphy Staging System for Burkitt Lymphoma
- Stage I: Single nodal or extranodal site, excluding mediastinum or abdomen.
- Stage II: Single extranodal tumor with regional nodal involvement.
- Two extranodal tumors on one side of the diaphragm.
- Primary gastrointestinal tumor with or without associated mesenteric nodes.
- Two+ nodal areas on one side of the diaphragm.
- Stage IIR: Completely resected intra-abdominal disease.
- Stage III: Two single extranodal tumors on opposite sides of the diaphragm.
- All primary intrathoracic tumors.
- All paraspinal or epidural tumors.
- Extensive primary intra-abdominal disease.
- Two+ nodal areas on both sides of the diaphragm.
- Stage IIIA: Localized, nonresectable abdominal disease.
- Stage IIIB: Widespread multi-organ abdominal disease.
- Stage IV: Initial central nervous system or marrow involvement (<25%).
Differential Diagnosis
- Burkitt Lymphoma:
- Clinical features: Occurs in children and adults with male predominance, presenting bulky, rapidly growing masses predominantly in extranodal sites.
- Morphology: Uniform or slightly pleomorphic medium-sized cells with a starry sky appearance.
- Immunophenotype: CD19+, CD20+, CD10+, BCL6+, BCL2-, TDT-, Ki67~100%, monotypic sIg+.
- Genotype: Characterized by t(8,14), t(8,2), t(8,22), without bcl2 or bcl6 translocation.
- Diffuse Large B-Cell Lymphoma:
- Clinical features: more common in adults than children, with nodal or extranodal large masses that are often localized.
- Morphology: Large oval, irregular, or lobated nuclei with scant cytoplasm.
- Immunophenotype: CD20+, CD10-/+, BCL6+/-, BCL2+/-, monotypic sIg+.
- Genotype: Often associated with BCL2 and BCL6 abnormalities, and sometimes MYC abnormalities in minority.
- B-Lymphoblastic Lymphoma:
- Clinical features: More common in children than adults, associated with leukemia.
- Morphology: Small to medium-sized cells of variable size and shape.
- Immunophenotype: CD19+, CD20-/+, TDT+.
- Genotype: Variable, often hyperdiploidy.
- T-Lymphoblastic Lymphoma:
- Clinical features: More common in adolescents and young adults and older adults, with male predominance and mediastinum involvement.
- Morphology: Small to medium-sized cells of variable size and shape.
- Immunophenotype: CD3+, TDT+.
- Genotype: Variable.
- Mantle Cell Lymphoma:
- Clinical features: Occurs mostly in middle-aged and older adults, male to female ratio, widespread disease.
- Morphology: Medium to large-sized lymphoblastic-like cells with scanty cytoplasm.
- Immunophenotype: CD20+, CD5+, CD10-, BCL6-, BCL2+, CCD1+, monotypic sIg+.
- Genotype: Characterized by t(11,14) involving bcl1 and IGH.
- Florid Follicular Hyperplasia:
- Clinical Features: Can occur in children and adults,
- Morphology: large irregular follicles
- Immunophenotype: , CD20+,CD10+,BCL6+,BCL2+
- Genotype: No clonal Abnormalities
Treatment
- Burkitt Lymphoma: Highly aggressive, but responds well to multi-agent chemotherapeutic programs, leading to excellent long-term survival.
- Rituximab: Commonly used with combination chemotherapy because of high CD20 expression on BL cells.
- Chemotherapy Regimens: Most regimens include:
- Cyclophosphamide
- Doxorubicin
- Vincristine
- Methotrexate
- Ifosfamide
- Etoposide
- High-dose cytarabine -Rituximab in combination with intrathecal chemotherapy.
- Dose-Intense, Short-Duration Strategy: Used due to high tumor proliferation.
- This minimizes rapid growth and resistance development between cycles.
- G-CSF (Granulocyte Colony-Stimulating Factors): It helps to keep the dose high and treat severe neutropenia.
- HIV-Positive Patients: Should be treated like immunocompetent patients in the era of highly active antiretroviral therapy.
- Tumor Lysis Syndrome (TLS): High risk due to high tumor cell proliferation and levels acid dehydrogenase
- Manage with careful hydration (~3 L of saline per day).
- Allopurinol or rasburicase (for rapid onset of action in high-risk and spontaneous cases).
- Short-term continuous veno-venous hemofiltration to allow concomitant full-dose chemotherapy, preventing lysis syndrome and renal failure.
Prognosis
- Overall, intensive chemotherapy regimens can cure approximately 50–80% of adult patients.
- Cure rates higher in pediatric populations.
- Overall survival is age-dependent.
- OS in children is approximately 90%.
- OS in adults less than 70 years is approximately 50%.
- OS in adults greater than 70 years is 25% to 30%.
- Rituximab-Containing Regimens:
- Complete response (CR) rates: 80–94%.
- 3-year progression-free survival (PFS) rates: 70–90%.
- Relapses: Typically occur within the first 12 months post-treatment; rare after 1 year.
- Prognosis for relapsed or refractory BL is poor.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.