Podcast
Questions and Answers
What is the result of alpha-adrenergic receptor stimulation in terms of cAMP levels and their effect on mast cells?
What is the result of alpha-adrenergic receptor stimulation in terms of cAMP levels and their effect on mast cells?
- Decreased cAMP leading to bronchodilation
- Increased cAMP leading to increased chemical mediator release
- Increased cAMP leading to decreased chemical mediator release
- Decreased cAMP leading to increased chemical mediator release (correct)
Which of the following comorbid conditions is NOT commonly associated with asthma?
Which of the following comorbid conditions is NOT commonly associated with asthma?
- Drug-induced asthma
- Gastroesophageal reflux
- Allergic bronchopulmonary aspergillosis
- Chronic obstructive pulmonary disease (correct)
What are the three most common symptoms of asthma?
What are the three most common symptoms of asthma?
- Cough, fatigue, and dyspnea
- Cough, nasal congestion, and wheezing
- Cough, dyspnea, and wheezing (correct)
- Chest tightness, wheezing, and fever
Which of the following factors is NOT typically considered an environmental trigger for asthma?
Which of the following factors is NOT typically considered an environmental trigger for asthma?
What is the significance of elevated IgE levels in asthma patients?
What is the significance of elevated IgE levels in asthma patients?
What is a primary characteristic of bronchiectasis in relation to lung tissue?
What is a primary characteristic of bronchiectasis in relation to lung tissue?
Which of the following conditions is least likely to contribute to the development of bronchiectasis?
Which of the following conditions is least likely to contribute to the development of bronchiectasis?
What diagnostic test is primarily used to establish the diagnosis of bronchiectasis?
What diagnostic test is primarily used to establish the diagnosis of bronchiectasis?
How does bronchiectasis typically affect alveoli distal to an obstruction?
How does bronchiectasis typically affect alveoli distal to an obstruction?
What is one of the primary objectives of medical management for bronchiectasis?
What is one of the primary objectives of medical management for bronchiectasis?
Flashcards are hidden until you start studying
Study Notes
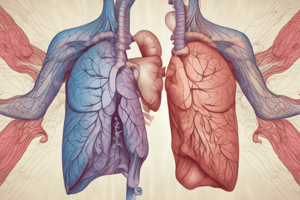
Bronchiectasis
- Bronchiectasis is a condition caused by a variety of factors, including airway obstruction, diffuse airway injury, pulmonary infections, genetic disorders like cystic fibrosis, and immune deficiencies.
- It is characterized by permanent dilation and distortion of the bronchial walls, leading to impaired mucociliary clearance.
- This condition typically affects a segment or a lobe of the lung, most commonly the lower lobes.
- Secretion retention and obstruction cause alveolar collapse, resulting in inflammatory scarring and fibrosis, replacing functional lung tissue.
- Bronchiectasis manifests with chronic cough, copious purulent sputum production, hemoptysis, finger clubbing, and recurrent pulmonary infections.
- Diagnosis is confirmed through a computed tomography (CT) scan, revealing bronchial dilation.
- Treatment aims to promote bronchial drainage, remove excessive secretions, and prevent or control infections.
- Postural drainage helps reduce secretions and infection by gravity.
- Medications like alpha-adrenergic receptor stimulants cause bronchoconstriction, while beta2-receptor stimulants promote bronchodilation.
Asthma
- Asthma is a chronic inflammatory disease affecting the airways, causing cough, dyspnea, and wheezing.
- Asthma attacks are frequent at night or early morning, potentially due to circadian rhythm variations.
- The condition can be triggered by various environmental factors including seasonal changes, pollen, mold, cold air, air pollution, and occupational chemicals.
- Asthma can be associated with gastroesophageal reflux, drug-induced asthma, and allergic bronchopulmonary aspergillosis.
- Diagnostic findings include eosinophilia and elevated IgE levels in cases of allergy.
- Blood gas analysis typically reveals hypoxemia and respiratory alkalosis.
Asthma Prevention
- Prevention focuses on identifying triggers and avoiding them.
- Patient education is crucial for managing asthma effectively, including proper inhalation techniques, peak flow monitoring, and action plan implementation.
- Patients require a calm approach to manage anxiety and fear associated with dyspnea.
- Medical interventions include monitoring respiratory status, administering prescribed medications, providing fluids for dehydration, antibiotics for infection, and assisting with intubation procedures in acute respiratory failure.
Peak Flow Monitoring
- Peak flow meters measure the highest airflow during forced expiration.
- Patients are instructed on proper technique for maximal effort.
- Personal best peak flow readings are determined after several weeks of optimal asthma therapy.
- Different zones (green, yellow, red) indicate severity levels, prompting specific actions for each zone.
Pulmonary Embolism
- Pulmonary embolism is an obstruction of a pulmonary artery or its branch by blood clots, air, fat, amniotic fluid, or septic thrombus.
- The obstructed area experiences reduced or absent blood flow, creating dead space where gas exchange is impaired.
- Inflammation causes regional blood vessel and bronchiole constriction, increasing pulmonary vascular resistance, pulmonary arterial pressure, and right ventricular workload.
- This leads to ventilation-perfusion imbalance, right ventricular failure, and potential shock.
Pulmonary Embolism Risk Factors
- Prolonged immobility contributes to venous stasis.
- Hypercoagulability increases the risk of clot formation.
- Venous endothelial disease, such as deep vein thrombosis (DVT) and thrombophlebitis, are significant risk factors.
- Certain disease states, including heart failure, trauma, postoperative conditions, diabetes mellitus, and COPD, increase the risk of pulmonary embolism.
- Other risk factors include advanced age, pregnancy, obesity, oral contraceptive use, constrictive clothing, and a history of pulmonary embolism, DVT, and thrombophlebitis.
Pulmonary Embolism Clinical Manifestations
- Symptoms vary depending on the thrombus size and the area affected.
- Common symptoms include dyspnea, tachypnea, sudden chest pain, anxiety, fever, tachycardia, cough, apprehension, hemoptysis, diaphoresis, and syncope.
Pulmonary Embolism Diagnostic Findings
- Chest x-ray may reveal infiltrate, atelectasis, elevated diaphragm on the affected side, and pleural effusion.
- ECG can show sinus tachycardia, PR interval depression, and ST segment changes.
- Arterial blood gases (ABG) may reveal hypoxemia and hypocapnia due to tachypnea.
- Ventilation-perfusion (V/Q) scan is used to evaluate different lung areas and compare V/Q in each region.
- CT scan of the lung is another diagnostic tool.
- D-dimer assay, a blood test for evidence of blood clots, may be elevated in cases of hypercoagulability.
- Pulmonary angiography, the gold standard for diagnosing pulmonary embolism, involves injecting dye through a catheter into the vena cava to identify the thrombus.
Pulmonary Embolism Prevention
- Exercising regularly to prevent venous stasis is crucial.
- Early ambulation after surgery or prolonged bed rest is recommended.
- Anticoagulant therapy (heparin, low molecular weight heparin) is a primary prevention tool.
- Sequential compression devices (SCDs) and elastic stockings help prevent venous stasis.
- Staying hydrated during travel and taking regular breaks is recommended for long journeys.
- Compression stockings and anticoagulant medication are advised before and after surgery.
- Maintaining a healthy lifestyle through exercise, balanced diet, and smoking cessation helps reduce the risk of pulmonary embolism.
Pulmonary Embolism Medical Management
- Treatment aims to lyse existing emboli and prevent new ones from forming.
- General measures include improving respiratory and vascular status.
- Anticoagulant therapy (heparin, warfarin) is essential.
- Thrombolytic therapy (streptokinase, urokinase) may be used for dissolving existing thrombi.
- Monitoring coagulation parameters like PTT, INR, hematocrit, and platelet count is important.
- Surgical intervention (embolectomy) may be required for patients unresponsive to medications or with contraindications for medication use.
Pulmonary Embolism Nursing Management
- Minimizing the risk of pulmonary embolism is a primary nursing concern.
- Preventing thrombus formation involves encouraging early ambulation, leg exercises, avoiding leg dangling, ensuring adequate foot support, proper care of intravenous devices, and assessing risk factors.
- Monitoring patients receiving thrombolytic therapy is critical.
- Managing oxygen therapy is important to address hypoxemia.
- Relieving anxiety and providing reassurance is essential.
- Postoperative care includes monitoring vital signs, urinary output, elevating legs, implementing isometric exercise, using elastic stockings, avoiding sitting to prevent hip flexion, and closely monitoring for complications.
Chronic Obstructive Pulmonary Disease (COPD)
- COPD is characterized by airflow limitation that is not fully reversible, encompassing diseases like emphysema and chronic bronchitis.
- COPD is a significant health concern, currently ranking as the fourth leading cause of death and the twelfth leading cause of disability in the United States.
- Asthma is now considered a separate condition but can coexist with COPD.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.