Podcast
Questions and Answers
Bone functions include support, protection, and movement.
Bone functions include support, protection, and movement.
True (A)
Calcium homeostasis is mainly regulated by sodium and magnesium.
Calcium homeostasis is mainly regulated by sodium and magnesium.
False (B)
Type 1 collagen fibers make up approximately 90-95% of the bone matrix.
Type 1 collagen fibers make up approximately 90-95% of the bone matrix.
True (A)
Osteoporosis is a condition that strengthens bones.
Osteoporosis is a condition that strengthens bones.
Proteoglycans provide tensile strength to bones.
Proteoglycans provide tensile strength to bones.
PTH promotes the reabsorption of Ca2+ in the proximal tubule of the kidney.
PTH promotes the reabsorption of Ca2+ in the proximal tubule of the kidney.
Active vitamin D is also known as calcitriol.
Active vitamin D is also known as calcitriol.
The kidney is not a regulatory site for the activation of vitamin D.
The kidney is not a regulatory site for the activation of vitamin D.
1α-hydroxylase is essential for the synthesis of active vitamin D.
1α-hydroxylase is essential for the synthesis of active vitamin D.
Bone mineral is composed of hydroxyapatite, which has the formula Ca10(PO4)6(OH)2.
Bone mineral is composed of hydroxyapatite, which has the formula Ca10(PO4)6(OH)2.
Active vitamin D promotes calcium absorption from the gut.
Active vitamin D promotes calcium absorption from the gut.
PTH stimulates phosphate reabsorption in the kidneys.
PTH stimulates phosphate reabsorption in the kidneys.
Vitamin D undergoes 25-hydroxylation in the liver as a rate-limiting step in its activation.
Vitamin D undergoes 25-hydroxylation in the liver as a rate-limiting step in its activation.
The ionised form of calcium is represented as Ca+.
The ionised form of calcium is represented as Ca+.
Acidosis results in an increase in free calcium levels.
Acidosis results in an increase in free calcium levels.
PTH is released from the parathyroid glands when plasma calcium levels are high.
PTH is released from the parathyroid glands when plasma calcium levels are high.
Negative feedback controls PTH secretion.
Negative feedback controls PTH secretion.
The gastrointestinal tract absorbs approximately 350 mg of calcium daily.
The gastrointestinal tract absorbs approximately 350 mg of calcium daily.
PTH stimulates osteoblasts to promote bone reabsorption.
PTH stimulates osteoblasts to promote bone reabsorption.
Vitamin D3 is also known as 1,25 dihydroxycholecalciferol.
Vitamin D3 is also known as 1,25 dihydroxycholecalciferol.
The normal plasma calcium concentration is 2.5mmol/L.
The normal plasma calcium concentration is 2.5mmol/L.
PTH decreases calcium levels in the blood.
PTH decreases calcium levels in the blood.
The daily dietary intake of calcium is around 1000 mg.
The daily dietary intake of calcium is around 1000 mg.
Vitamin D increases the absorption of calcium and phosphate in the gut.
Vitamin D increases the absorption of calcium and phosphate in the gut.
Osteoporosis is characterized by an increase in bone mass and strength.
Osteoporosis is characterized by an increase in bone mass and strength.
Women are more likely to suffer a hip fracture than develop breast cancer after age 50.
Women are more likely to suffer a hip fracture than develop breast cancer after age 50.
Vitamin D deficiency primarily affects children and leads to a condition called osteomalacia.
Vitamin D deficiency primarily affects children and leads to a condition called osteomalacia.
The fusing of the epiphyseal plate marks the end of bone growth.
The fusing of the epiphyseal plate marks the end of bone growth.
Vitamin D and PTH are responsible for regulating plasma calcium levels.
Vitamin D and PTH are responsible for regulating plasma calcium levels.
Calcium excretion through urine amounts to 800 mg daily.
Calcium excretion through urine amounts to 800 mg daily.
Bone turnover involves cells called osteoblasts and osteoclasts.
Bone turnover involves cells called osteoblasts and osteoclasts.
Compressive strength resists tension.
Compressive strength resists tension.
Compact bone has a high porosity of 70%.
Compact bone has a high porosity of 70%.
Trabecular bone is also known as spongy bone.
Trabecular bone is also known as spongy bone.
The diaphysis is located at the ends of long bones.
The diaphysis is located at the ends of long bones.
Growth plates in long bones fuse around the age of 18.
Growth plates in long bones fuse around the age of 18.
Osteoclasts promote bone formation.
Osteoclasts promote bone formation.
Osteocytes are derived from osteoblasts and can sense mechanical load.
Osteocytes are derived from osteoblasts and can sense mechanical load.
Hydroxyapatite is the mineral found in osteoid.
Hydroxyapatite is the mineral found in osteoid.
Bone turnover in adults happens every 10 years.
Bone turnover in adults happens every 10 years.
PTH stimulates osteoclast activity indirectly through osteoblasts.
PTH stimulates osteoclast activity indirectly through osteoblasts.
Calcium is found in three forms in body fluids, including ionized and protein-bound forms.
Calcium is found in three forms in body fluids, including ionized and protein-bound forms.
A high calcium level in the body can stimulate neurotransmitter release.
A high calcium level in the body can stimulate neurotransmitter release.
Osteoblasts can lay down osteoid, which is a mineralized bone tissue.
Osteoblasts can lay down osteoid, which is a mineralized bone tissue.
During bone remodeling, growth factors stimulate the formation of osteoclasts.
During bone remodeling, growth factors stimulate the formation of osteoclasts.
The biological functions of bones do not include serving as a store for calcium and phosphate.
The biological functions of bones do not include serving as a store for calcium and phosphate.
Collagen provides compressive strength to bones while proteoglycans provide tensile strength.
Collagen provides compressive strength to bones while proteoglycans provide tensile strength.
PTH is released from the parathyroid glands when plasma calcium levels are low.
PTH is released from the parathyroid glands when plasma calcium levels are low.
Vitamin D deficiency leads to a condition called osteomalacia primarily in adults.
Vitamin D deficiency leads to a condition called osteomalacia primarily in adults.
The diaphysis is the central portion of long bones, not located at their ends.
The diaphysis is the central portion of long bones, not located at their ends.
Acidosis promotes the binding of Ca2+ to proteins, decreasing free [Ca2+].
Acidosis promotes the binding of Ca2+ to proteins, decreasing free [Ca2+].
PTH is secreted by chief cells in the parathyroid glands when plasma calcium levels are low.
PTH is secreted by chief cells in the parathyroid glands when plasma calcium levels are low.
The gastrointestinal tract secretes 150 mg of calcium daily.
The gastrointestinal tract secretes 150 mg of calcium daily.
PTH primarily stimulates osteoclasts to promote bone reabsorption.
PTH primarily stimulates osteoclasts to promote bone reabsorption.
High plasma [Ca2+] levels trigger the release of PTH.
High plasma [Ca2+] levels trigger the release of PTH.
A normal plasma calcium concentration is approximately 2.0 mmol/L.
A normal plasma calcium concentration is approximately 2.0 mmol/L.
PTH decreases the concentration of free calcium in the blood.
PTH decreases the concentration of free calcium in the blood.
The major controller of free Ca2+ in the body is parathyroid hormone (PTH).
The major controller of free Ca2+ in the body is parathyroid hormone (PTH).
Vitamin D3 has the same chemical structure as 1,25 dihydroxycholecalciferol.
Vitamin D3 has the same chemical structure as 1,25 dihydroxycholecalciferol.
The daily dietary intake of calcium in adults is approximately 800 mg.
The daily dietary intake of calcium in adults is approximately 800 mg.
Vitamin D promotes the absorption of phosphate in the gut.
Vitamin D promotes the absorption of phosphate in the gut.
Rickets in children is characterized by bowing of long leg bones due to unmineralised osteoid.
Rickets in children is characterized by bowing of long leg bones due to unmineralised osteoid.
Bone growth continues indefinitely in adulthood after the epiphyseal plates have fused.
Bone growth continues indefinitely in adulthood after the epiphyseal plates have fused.
Women are less likely to suffer a hip fracture than develop breast cancer after the age of 50.
Women are less likely to suffer a hip fracture than develop breast cancer after the age of 50.
PTH inhibits the reabsorption of Ca2+ in the thick ascending limb of the loop of Henle.
PTH inhibits the reabsorption of Ca2+ in the thick ascending limb of the loop of Henle.
Vitamin D deficiency primarily impacts adults and leads to rickets.
Vitamin D deficiency primarily impacts adults and leads to rickets.
Osteoporosis is characterized by low bone mass and increased bone fragility.
Osteoporosis is characterized by low bone mass and increased bone fragility.
The liver is responsible for the 1α-hydroxylation of vitamin D, which activates it.
The liver is responsible for the 1α-hydroxylation of vitamin D, which activates it.
The gastrointestinal tract absorbs approximately 800 mg of calcium daily.
The gastrointestinal tract absorbs approximately 800 mg of calcium daily.
Active vitamin D plays a role in promoting the mineralization of bone.
Active vitamin D plays a role in promoting the mineralization of bone.
PTH promotes phosphate excretion in the proximal and distal tubules of the kidney.
PTH promotes phosphate excretion in the proximal and distal tubules of the kidney.
Vitamin D and parathyroid hormone work together to regulate plasma Ca2+ levels.
Vitamin D and parathyroid hormone work together to regulate plasma Ca2+ levels.
Calcium absorption occurs in the stomach primarily through Ca2+ channels.
Calcium absorption occurs in the stomach primarily through Ca2+ channels.
The production of active vitamin D begins with UV-stimulated synthesis of vitamin D in the skin.
The production of active vitamin D begins with UV-stimulated synthesis of vitamin D in the skin.
25-hydroxylation is considered the rate-limiting step in the production of active form of vitamin D.
25-hydroxylation is considered the rate-limiting step in the production of active form of vitamin D.
The main function of the active form of vitamin D is to maximize excretion of calcium from the body.
The main function of the active form of vitamin D is to maximize excretion of calcium from the body.
Compact bone is also known as cancellous bone.
Compact bone is also known as cancellous bone.
Osteoblasts promote bone reabsorption by liberating calcium and phosphate.
Osteoblasts promote bone reabsorption by liberating calcium and phosphate.
Trabecular bone has a low porosity of approximately 5-25%.
Trabecular bone has a low porosity of approximately 5-25%.
The epiphyseal growth plate fuses around the age of 18, marking the end of long bone growth.
The epiphyseal growth plate fuses around the age of 18, marking the end of long bone growth.
Collagen deposition in bone is regulated by osteoclasts.
Collagen deposition in bone is regulated by osteoclasts.
The main function of osteocytes is to promote bone formation.
The main function of osteocytes is to promote bone formation.
PTH increases bone mineralization by directly activating osteoclasts.
PTH increases bone mineralization by directly activating osteoclasts.
Bone remodeling involves a balance between the activity of osteoblasts and osteocytes.
Bone remodeling involves a balance between the activity of osteoblasts and osteocytes.
Micronutrients such as calcium and phosphate are primarily regulated by the activity of osteocytes.
Micronutrients such as calcium and phosphate are primarily regulated by the activity of osteocytes.
The resorption phase of bone remodeling lasts for approximately 2 weeks.
The resorption phase of bone remodeling lasts for approximately 2 weeks.
Osteoblasts are derived from the macrophage lineage of cells.
Osteoblasts are derived from the macrophage lineage of cells.
The mineral found in bone tissue is hydroxyapatite, which aids in the hardness of bones.
The mineral found in bone tissue is hydroxyapatite, which aids in the hardness of bones.
Bone turnover in adults involves the continuous formation and reabsorption of bone.
Bone turnover in adults involves the continuous formation and reabsorption of bone.
Calcium is only found in the body in its ionized form.
Calcium is only found in the body in its ionized form.
The primary type of collagen in bone matrix contributes to compressive strength.
The primary type of collagen in bone matrix contributes to compressive strength.
Defective remodeling of bones can lead to a condition called osteoporosis.
Defective remodeling of bones can lead to a condition called osteoporosis.
PTH increases the storage of calcium in bones by stimulating the activity of osteoblasts.
PTH increases the storage of calcium in bones by stimulating the activity of osteoblasts.
The mineral composition of bone includes a significant presence of magnesium phosphates.
The mineral composition of bone includes a significant presence of magnesium phosphates.
Vitamin D is essential for the absorption of calcium from dietary sources in the intestine.
Vitamin D is essential for the absorption of calcium from dietary sources in the intestine.
Acidosis promotes Ca2+ binding to proteins, thereby decreasing free [Ca2+].
Acidosis promotes Ca2+ binding to proteins, thereby decreasing free [Ca2+].
The primary role of Parathyroid Hormone (PTH) is to lower the plasma levels of calcium.
The primary role of Parathyroid Hormone (PTH) is to lower the plasma levels of calcium.
Citrate, phosphate, and oxalate are the main regulators of ionized calcium (Ca2+) in the body.
Citrate, phosphate, and oxalate are the main regulators of ionized calcium (Ca2+) in the body.
PTH functions by stimulating osteoclasts, leading to enhanced bone reabsorption.
PTH functions by stimulating osteoclasts, leading to enhanced bone reabsorption.
A decrease in plasma calcium levels triggers the release of Parathyroid Hormone (PTH).
A decrease in plasma calcium levels triggers the release of Parathyroid Hormone (PTH).
Calcium is absorbed from the gastrointestinal tract at a rate of approximately 150 mg daily.
Calcium is absorbed from the gastrointestinal tract at a rate of approximately 150 mg daily.
Vitamin D enhances the binding of calcium to proteins in the bloodstream.
Vitamin D enhances the binding of calcium to proteins in the bloodstream.
The normal plasma calcium concentration is approximately 3.5 mmol/L.
The normal plasma calcium concentration is approximately 3.5 mmol/L.
The secretion of Parathyroid Hormone (PTH) is inhibited by high levels of plasma calcium.
The secretion of Parathyroid Hormone (PTH) is inhibited by high levels of plasma calcium.
Bone reabsorption primarily occurs in the diaphysis of long bones.
Bone reabsorption primarily occurs in the diaphysis of long bones.
Trabecular bone has a lower density compared to compact bone, characterized by high porosity.
Trabecular bone has a lower density compared to compact bone, characterized by high porosity.
The epiphyseal growth plate fuses at approximately age 12.
The epiphyseal growth plate fuses at approximately age 12.
Osteoblasts decrease in number after laying down osteoid and are not removed.
Osteoblasts decrease in number after laying down osteoid and are not removed.
Osteoclasts are associated with the lineage of fibroblasts and play a role in bone formation.
Osteoclasts are associated with the lineage of fibroblasts and play a role in bone formation.
Bone remodeling does not occur after reaching maturity.
Bone remodeling does not occur after reaching maturity.
Calcium movement across membranes is crucial for various physiological processes including heart muscle contraction.
Calcium movement across membranes is crucial for various physiological processes including heart muscle contraction.
The resorption phase of bone remodeling is the longest phase occurring for 26 weeks.
The resorption phase of bone remodeling is the longest phase occurring for 26 weeks.
Bone mineralization is solely achieved through the action of osteoclasts.
Bone mineralization is solely achieved through the action of osteoclasts.
PTH does not influence osteoblast activity but directly stimulates osteoclasts.
PTH does not influence osteoblast activity but directly stimulates osteoclasts.
Hydroxyapatite is formed from collagen fibers and is present in the osteon structure.
Hydroxyapatite is formed from collagen fibers and is present in the osteon structure.
During the reversal phase of bone remodeling, osteoblasts are attracted to the resorption sites to prepare for bone deposition.
During the reversal phase of bone remodeling, osteoblasts are attracted to the resorption sites to prepare for bone deposition.
Collagen contributes to the tensile strength of bones, while proteoglycans provide compressive strength.
Collagen contributes to the tensile strength of bones, while proteoglycans provide compressive strength.
PTH and Vitamin D work together to decrease plasma calcium levels.
PTH and Vitamin D work together to decrease plasma calcium levels.
Osteocytes are the only cells in bone that do not directly contribute to the bone formation process.
Osteocytes are the only cells in bone that do not directly contribute to the bone formation process.
Calcium can exist in the body in an ionized form, as well as bound to proteins and small anions.
Calcium can exist in the body in an ionized form, as well as bound to proteins and small anions.
Phosphate reabsorption is promoted by PTH in the distal tubule of the kidney.
Phosphate reabsorption is promoted by PTH in the distal tubule of the kidney.
The synthesis of active vitamin D involves a rate-limiting step during 25-hydroxylation in the liver.
The synthesis of active vitamin D involves a rate-limiting step during 25-hydroxylation in the liver.
Active vitamin D, known as calcitriol, is produced in the liver.
Active vitamin D, known as calcitriol, is produced in the liver.
The main action of active vitamin D is to enhance calcium absorption in the duodenum.
The main action of active vitamin D is to enhance calcium absorption in the duodenum.
The hydroxyapatite formula is represented as Ca12(PO4)6(OH)2.
The hydroxyapatite formula is represented as Ca12(PO4)6(OH)2.
The reabsorption of bone minerals decreases plasma phosphate concentration.
The reabsorption of bone minerals decreases plasma phosphate concentration.
Vitamin D is a steroid-like structure that acts on intracellular receptors.
Vitamin D is a steroid-like structure that acts on intracellular receptors.
PTH promotes the excretion of calcium in the kidneys.
PTH promotes the excretion of calcium in the kidneys.
Vitamin D promotes the synthesis of Ca2+ channels and phosphate absorption in the kidney tubules.
Vitamin D promotes the synthesis of Ca2+ channels and phosphate absorption in the kidney tubules.
Osteoporosis is characterized by increased bone mass and structural integrity.
Osteoporosis is characterized by increased bone mass and structural integrity.
Vitamin D deficiency can lead to the condition known as rickets in adults.
Vitamin D deficiency can lead to the condition known as rickets in adults.
The daily calcium absorption from the gastrointestinal tract is estimated to be around 350 mg.
The daily calcium absorption from the gastrointestinal tract is estimated to be around 350 mg.
Women are less likely to suffer a hip fracture than develop breast cancer after the age of 50.
Women are less likely to suffer a hip fracture than develop breast cancer after the age of 50.
Bone growth stops when the epiphyseal plate fuses, but bone turnover continues throughout life.
Bone growth stops when the epiphyseal plate fuses, but bone turnover continues throughout life.
Calcium excretion through feces is estimated to be more than urinary excretion daily.
Calcium excretion through feces is estimated to be more than urinary excretion daily.
PTH primarily increases phosphate levels in the blood.
PTH primarily increases phosphate levels in the blood.
Flashcards are hidden until you start studying
Study Notes
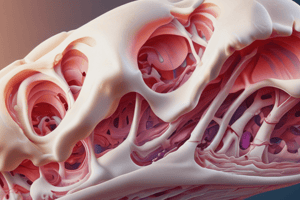
Bone Structure & Function
- Bone provides structural support and protection, enables movement, acts as a storage site for calcium and phosphate, and contains bone marrow
- The bone matrix consists mainly of collagen type 1 fibers and proteoglycans
- Collagen contributes to tensile strength, proteoglycans to compressive strength
- Two main types of bone exist : compact (cortical) and trabecular (cancellous)
- The combination of compact and trabecular bone provides mechanical strength while remaining lightweight
- Compact bone is dense, stiff, with low porosity, comprising ~80% of human bone
- Trabecular bone is spongy, light, with high porosity
- Long bones feature cortical bone in the shaft (diaphysis) and trabecular bone at the ends (epiphysis/metaphysis)
- The epiphyseal growth plate separates the epiphysis from the metaphysis
- Growth in long bones occurs at the growth plate until approximately 18 years of age, when it fuses with the metaphysis
- During fetal development, bones are initially modeled in cartilage, then mineralized through ossification
- Cartilage proliferation at the growth plate contributes to longitudinal bone growth during childhood and adolescence, controlled by growth hormone and IGF-1
- Once the growth plate fuses, cartilage proliferation ceases and bone ossification occurs
- Osteons form the basic unit of cortical bone growth, characterized by concentric circles of collagen deposition around a central blood vessel in Haversian canals
- Osteoid, an unmineralized collagen matrix, is laid down by osteoblasts
- During ossification, hydroxyapatite, a calcium phosphate mineral, is deposited within the collagen matrix
Bone Cells
- Three main cell types exist in bone: osteoblasts, osteoclasts, and osteocytes
- Osteoblasts promote bone formation by laying down osteoid and initiating mineralization
- Osteoclasts promote bone resorption by removing mineral and liberating calcium and phosphate
- Osteocytes transfer mineral from the bone interior towards growth surfaces, and sense mechanical load on the bone
Bone Remodelling
- Bone remodeling occurs throughout life, replacing bone tissue every 10 years, with approximately 1 million bone metabolic units (BMU) active at any given time
- Osteoblasts and osteoclasts maintain a balance by removing and adding bone mineral constantly
- This process enables adaptation to mechanical loading, fracture healing, and prevention of "bone fatigue"
- Osteocytes signal osteoblasts in response to mechanical strain, PTH/vitamin D signalling, and other growth factors
- Osteoblasts activate circulating monocytes to become osteoclasts which then resorb the bone
- The resorption process lasts approximately 2 weeks, followed by a reversal phase lasting 2 weeks for preparation of subsequent bone deposition
- The final phase, formation, lasts 13 weeks, where osteoblasts deposit osteoid, which then mineralizes, completing the cycle
Calcium Homeostasis
- Calcium movement across membranes is critical for various physiological processes, including neurotransmitter release, muscle contraction, hormone secretion, and enzymatic activity
- Calcium exists in three forms: ionized (free), bound to protein, and bound to small anions
- Physiological processes are primarily mediated by the ionized (free) form of calcium
- Parathyroid hormone (PTH) plays a key role in regulating free calcium levels in the body
- Chief cells within the parathyroid glands release PTH in response to low plasma calcium concentrations
- A G-protein receptor coupled to cAMP detects calcium levels
- PTH promotes both calcium and phosphate release from bone by stimulating bone reabsorption through the activation of osteoclasts to break down the mineralized bone matrix
- PTH actions on the kidneys help modulate calcium and phosphate levels
- PTH increases calcium reabsorption in the thick ascending limb of the loop of Henle, and inhibits phosphate reabsorption in the proximal and distal tubules
Vitamin D
- Active vitamin D, 1,25-dihydroxycholecalciferol (DHCC), is synthesized in the liver and kidney
- The liver performs 25-hydroxylation, while the kidney carries out the key step of 1α-hydroxylation, making the kidney a crucial regulatory site
- Vitamin D promotes calcium absorption from the gut by increasing the synthesis of calcium channels and binding proteins such as calbindin
- In the kidney tubules, vitamin D also promotes calcium and phosphate reabsorption
- The overall effect of vitamin D is to increase calcium and phosphate flux into bone
Osteoporosis
- Defined as systemic skeletal disease characterized by low bone mass and deterioration of bone tissue
- Results in bone fragility and increased fracture risk, particularly in post-menopausal women
- The aging population and increasing life expectancy contribute to a higher incidence of osteoporotic fractures
- Women are more likely to suffer a hip fracture than develop breast cancer
Vitamin D Deficiency
- Deficiency in vitamin D leads to rickets in children, characterized by excessive unmineralized osteoid and potentially leading to bone deformities, like bowing of long leg bones
- Osteomalacia, affecting adults, is another consequence of vitamin D deficiency, resulting in bone weakness due to unmineralized osteoid, but without bowing of the legs as longitudinal growth is complete
Functions of Bone
- Bone provides support, protection, movement, calcium and phosphate storage, and houses bone marrow.
- Bone is a mineralised organic matrix composed of Type 1 collagen (90-95%) and proteoglycans (5%).
- Collagen provides tensile strength, and proteoglycans provide compressive strength.
Types of Bone
- Compact bone, also known as cortical bone, is dense, stiff, and has low porosity (5-25%).
- Trabecular bone, also known as cancellous or spongy bone, is spongy, light, and has high porosity (up to 70%).
- The combination of compact and trabecular bone provides mechanical strength while remaining lightweight.
Bone Structure
- Long bones have a diaphysis (shaft) composed of cortical bone and epiphysis/metaphysis (ends) composed of trabecular bone.
- The epiphyseal growth plate is present between the epiphysis and metaphysis.
- Long bone growth occurs at the growth plate until about 18 years old, when it fuses with the metaphysis.
Bone Growth
- During fetal life, bones are modelled in cartilage (Type 1 collagen) and then mineralised through ossification.
- During childhood/adolescence, cartilage proliferates at the growth plate, elongating the bones.
- Elongation is controlled by growth hormone (GH) and insulin-like growth factor-1 (IGF-1).
- After growth plate fusion, cartilage proliferation and elongation stop, and vascularisation and ossification take over.
Microstructure of Cortical Bone
- The osteon is the unit of bone growth, consisting of concentric circles of collagen deposition around a blood vessel.
- Blood vessels are located in Haversian canals.
- Collagen is mineralized with hydroxyapatite (Ca10(PO4)6(OH)2) during ossification.
Cells of Bone
- Three main cell types: Osteoblasts, osteoclasts, and osteocytes.
- Osteoblasts promote bone formation by laying down osteoid and initiating mineralization.
- Osteoclasts promote bone reabsorption by removing mineralization and liberating calcium and phosphate.
- Osteocytes transfer mineral from inner regions of the bone to the growth surfaces.
Osteoblasts
- Osteoblasts are modified fibroblasts derived from mesenchymal stem cells.
- They lay down osteoid (Type 1 collagen matrix) and facilitate its ossification.
- Some osteoblasts become embedded in the lining of new bone and become osteocytes.
Osteocytes
- Osteocytes are derived from osteoblasts.
- They transfer mineral from the inner regions of the bone to the growth surfaces.
- Osteocytes have cytoplasmic projections into the bone that sense mechanical load and relay this information to osteoblasts.
Osteoclasts
- Osteoclasts are derived from the macrophage lineage of cells.
- They are attracted to and resorb mineralized bone, creating resorption pits.
- They solubilize the mineral at low pH and phagocytose the organic matrix.
- They require factors from osteoblasts to function and are indirectly stimulated by PTH.
Bone Remodelling
- From maturity, bone growth stops but bone turnover continues, with the entire skeleton being remodelled every 10 years.
- Bone turnover maintains a balance between mineralization and resorption.
- It enables adaptation to mechanical loading, fracture healing, and prevents "bone fatigue" by continually renewing the bone matrix.
- The cycle involves osteoblast and osteoclast activation in response to osteocyte signalling, PTH/vitamin D signalling, and other growth factors.
Bone Remodelling Phases
- Resorption (2 weeks): Bone lining cells detach from bone surfaces, osteoclasts are attracted, and bone is resorbed by osteoclasts, creating resorption pits.
- Reversal (2 weeks): Resorption pits are prepared for bone deposition, and a cement line is formed.
- Formation (13 weeks): Osteoblasts are attracted to resorption sites, deposit osteoid which mineralizes, and some become osteocytes or bone lining cells.
Calcium and Phosphate Regulation
- Calcium movement across membranes is crucial for many physiological processes: neurotransmitter release, muscle contraction, hormone secretion, and gut enzyme secretion.
- Calcium in body fluids exists in three forms: ionised (free), bound to protein, and bound to small anions.
- Ionised calcium is responsible for physiological function, and its levels are affected by acid-base status.
Daily Calcium Regulation
- Calcium is ingested, absorbed from the gastrointestinal tract, and excreted through urine and feces.
- The skeleton acts as a calcium reservoir.
Parathyroid Hormone (PTH)
- PTH is the primary regulator of free calcium in the body.
- It is released from chief cells in the parathyroid glands when plasma calcium levels are low.
- PTH is detected by a membrane-bound G-protein receptor coupled to cAMP, which inhibits PTH release when calcium levels are high.
PTH Action on the Kidney
- PTH promotes calcium reabsorption in the thick ascending limb of the loop of Henle.
- PTH inhibits phosphate reabsorption in the proximal and distal tubules, promoting its excretion.
- PTH also stimulates 1α-hydroxylase, the key enzyme in the synthesis of active vitamin D.
Active Vitamin D Production
- The active form of vitamin D is 1,25 dihydroxycholecalciferol (DHCC, also known as calcitriol).
- Vitamin D undergoes 25-hydroxylation in the liver, followed by 1α-hydroxylation in the kidney, which is the rate-limiting step.
Actions of Vitamin D on Calcium
- Vitamin D promotes calcium absorption in the duodenum by increasing the synthesis of calcium channels and binding proteins.
- It also promotes phosphate absorption in the gut.
- In kidney tubules, vitamin D promotes calcium and phosphate reabsorption.
Osteoporosis
- A systemic skeletal disease with low bone mass and deterioration of bone tissue, leading to fragility and fracture risk.
- 33% of females will suffer a fracture after age 50, compared to 20% of males.
- Risk increases with an aging population.
Vitamin D Deficiency
- Rickets (in children): Abnormal amounts of unmineralized osteoid, leading to bowing of long bones.
- Osteomalacia (in adults): Bone weakness due to unmineralized osteoid.
Summary
- Bone growth stops with the fusion of the epiphyseal plate in long bones.
- Bone turnover continues throughout life, mediated by osteoblasts, osteoclasts, and osteocytes.
- Vitamin D and PTH regulate plasma calcium levels and bone mineralization.
- Vitamin D deficiency can alter calcium availability and decrease bone mineralization.
Bone Structure & Function
- Bones play crucial roles in support, protection, movement, calcium storage, and housing bone marrow.
- The bone matrix, a combination of organic and inorganic components, provides strength and resilience.
- Collagen fibers, composing 90-95% of the matrix, offer tensile strength, while proteoglycans contribute compressive strength.
Bone Types
- Compact Bone (cortical bone): Dense, stiff, low porosity.
- Approximately 80% of human bone is compact.
- Trabecular Bone (cancellous or spongy bone): Spongy, light, high porosity (up to 70%).
Bone Macrostructure
- Long bones consist of a diaphysis (shaft) composed of cortical bone and epiphyses (ends) containing trabecular bone.
- The epiphyseal growth plate, located between the epiphysis and metaphysis, is responsible for longitudinal bone growth until fusion occurs around age 18.
Bone Growth
- Begins with cartilaginous models during fetal development, followed by ossification (mineralization).
- Cartilage growth at the growth plate elongates long bones, regulated by growth hormone and IGF-1.
- After plate fusion, growth ceases, replaced by vascularization and ossification.
Bone Microstructure
- The osteon, the functional unit of bone growth, consists of concentric rings of collagen deposited around blood vessels, housed in Haversian canals.
- Mineralization of collagen with hydroxyapatite (Ca10(PO4)6(OH)2) facilitates bone formation.
Cells of Bone
- Osteoblasts: Promote bone formation, lay down osteoid (unmineralized matrix), and initiate mineralization.
- Osteoclasts: Promote bone resorption, remove mineralized bone, liberate calcium and phosphate, and create resorption pits.
- Osteocytes: Contribute to mineral transfer from inner regions to growth surfaces, sense mechanical load, and communicate with osteoblasts.
Bone Remodelling
- A continuous, lifelong process of bone turnover, with 1 million bone metabolic units (BMUs) active at any given time.
- The balance between osteoblast and osteoclast activity allows adaptation to mechanical loading, fracture healing, and renewal of bone matrix.
- Occurs over a 120 day cycle divided into: Resorption (~2 weeks), Reversal (~2 weeks), and Formation (~13 weeks).
Calcium regulation
- Calcium plays a vital role in various physiological processes, including neurotransmitter release, muscle contraction, and hormonal secretion.
- Exists in three forms: Ionized (free) Ca2+ (45%), protein-bound Ca2+ (45%), and Ca2+ bound to small anions (10%).
- Acid-base status affects bound Ca2+ levels, with acidosis increasing free Ca2+ and alkalosis decreasing it.
Parathyroid Hormone (PTH)
- The primary regulator of free Ca2+ in the body, secreted by parathyroid glands in response to low plasma Ca2+.
- Acts through G-protein coupled receptors, increasing cAMP production and inhibiting PTH release when Ca2+ levels rise.
- Stimulates bone resorption, increasing plasma Ca2+ and phosphate levels.
- Promotes Ca2+ reabsorption in the kidneys and inhibits phosphate reabsorption, leading to increased phosphate excretion.
- Activates 1α-hydroxylase, the key enzyme in active vitamin D synthesis.
Vitamin D
- Synthesized in the skin through UV exposure or obtained through dietary sources.
- Converted to its active form (1,25-dihydroxycholecalciferol, calcitriol) through 25-hydroxylation (liver) and 1α-hydroxylation (kidney).
- Acts on intracellular receptors to promote Ca2+ and phosphate absorption in the gut.
- Enhances Ca2+ reabsorption in the kidneys, ultimately increasing Ca2+ and phosphate flux into bone.
Osteoporosis
- A skeletal disease characterized by low bone mass and microarchitectural deterioration, leading to bone fragility and fracture susceptibility.
- Affects 33% of women after age 50 and 20% of men.
- Increasing lifespan in the elderly population increases risk.
Vitamin D Deficiency
- Rickets: Abnormal amounts of unmineralized osteoid, leading to bowing of long bones in growing children.
- Osteomalacia: Bone weakness due to unmineralized osteoid in adults, but without bowing due to completed longitudinal bone growth.
Summary
- Bone growth ceases after epiphyseal plate fusion, but bone remodeling persists throughout life, mediated by osteoblasts, osteoclasts, and osteocytes.
- PTH and vitamin D control plasma Ca2+ levels, impacting bone mineralization.
- Vitamin D deficiency alters Ca2+ availability and hinders bone mineralization.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.