Podcast
Questions and Answers
Which cell type is primarily responsible for the breakdown of bone tissue?
Which cell type is primarily responsible for the breakdown of bone tissue?
- Chondrocytes
- Osteocytes
- Osteoclasts (correct)
- Osteoblasts
What is the main function of collagen in the extracellular matrix of connective tissue?
What is the main function of collagen in the extracellular matrix of connective tissue?
- Facilitate nerve signal transmission
- Act as the main component of blood
- Provide flexibility and elasticity
- Offer strength and structural support (correct)
The Haversian system is primarily associated with which aspect of bone?
The Haversian system is primarily associated with which aspect of bone?
- The storage of calcium in the blood
- The organization of vascular structures within bone (correct)
- The growth process of tendons
- The fibrous composition of cartilage
Which of the following best describes the purpose of the skeletal system in vertebrates?
Which of the following best describes the purpose of the skeletal system in vertebrates?
Which component is NOT part of the extracellular matrix in connective tissues?
Which component is NOT part of the extracellular matrix in connective tissues?
What role do osteocytes play in bone structure?
What role do osteocytes play in bone structure?
Which of the following accurately describes woven bone?
Which of the following accurately describes woven bone?
What is the composition of the inorganic matrix in bone?
What is the composition of the inorganic matrix in bone?
During which growth period does the increase in growth hormone release primarily occur?
During which growth period does the increase in growth hormone release primarily occur?
What does the periosteum mainly serve as?
What does the periosteum mainly serve as?
Flashcards
Osteoblasts
Osteoblasts
Specialized cells that are responsible for bone formation. They synthesize and secrete the organic matrix of bone, called osteoid.
Osteocytes
Osteocytes
Mature bone cells that reside within lacunae in the bone matrix. They maintain bone tissue and help regulate calcium exchange.
Osteoclasts
Osteoclasts
Large, multinucleated cells that are responsible for bone resorption. They break down bone tissue, releasing calcium into the bloodstream.
Osteoid
Osteoid
Signup and view all the flashcards
Bone Minerals
Bone Minerals
Signup and view all the flashcards
Hydroxyapatite
Hydroxyapatite
Signup and view all the flashcards
Woven Bone
Woven Bone
Signup and view all the flashcards
Lamellar Bone
Lamellar Bone
Signup and view all the flashcards
Study Notes
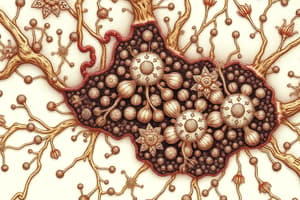
Bone Structure and Function
- Bone is a type of connective tissue, along with ligaments and tendons.
- Bone is comprised of specialized cells and extracellular matrix (ECM).
Bone Tissue Structure
- Bone tissue has three main components: cells, fibrous elements (e.g., collagen fibers), and ground substance (special proteins).
- Cells are not tightly packed, separated by abundant ECM.
- ECM variations give bone its structure and function (e.g. fluid, solid, or gel).
- Various cell types are embedded within bone tissue.
- Bone: osteo- (cytes, blasts, clasts)
- Cartilage: chondro-
- Muscle: myo-
- Tendons: teno-
Extracellular Matrix (ECM)
- ECM of bone is comprised of osteoid.
- Osteoid is an organic material rich in mucopolysaccharides and collagen fibers.
- Osteoid is produced by osteoblasts and secreted onto existing bone surfaces.
- Osteoid provides tensile strength to bone.
Components of Osteoid
- Collagen type I forms about 90% of osteoid (with trace amounts of type V).
- Collagen provides tensile strength and structure.
- Glycoproteins (osteonectin, osteocalcin) bind collagen and minerals.
- Proteoglycans (biglycan, decorin) bind growth factors.
- Bone sialoproteins (osteopontin, thrombospondin) are associated with cell adhesion.
Inorganic Minerals in Bone
- Bone contains inorganic hydroxyapatite (Ca10(PO4)6(OH)2).
- Hydroxyapatite minerals are normally dissolved in extracellular fluid (ECF).
- These minerals crystallize around collagen fibers, hardening bone.
- Minerals make bone radio-opaque and provide compressional strength whilst being relatively lightweight (60-70% of dry weight).
Types of Bone
- Woven bone: Random arrangement of collagen fibers, formed quickly (e.g. during growth or fracture repair).
- Lamellar bone: Regular, parallel bands of collagen fibers, stronger and more resilient than woven bone.
Gross Structure of a Long Bone
- Diaphysis: The long, cylindrical shaft.
- Epiphysis: The flared, articulating ends.
- Bone marrow fills the central cavity (for blood cell production).
- Periosteum: Connective tissue sheath covering the outside of the bone.
Gross Bone Morphology
- Compact (Lamellar) bone: dense outer layer.
- Spongy (Trabecular) bone: "lacy" inner core.
- Epiphyseal plate: Cartilage layer between epiphysis and diaphysis.
Bone Growth Periods
- Postnatal growth spurt: In early life, mainly skeletal muscle increase.
- Pubertal growth spurt: Increased growth hormone (GH) release leading to increase in size (hypertrophy) and number (hyperplasia) of cells in soft tissue. Promotes lengthening and thickening of long bones.
Growth in Length (Ossification)
- Chondrocytes (cartilage cells) proliferate in the outer edge of epiphyseal plates next to epiphysis.
- Old chondrocytes enlarge on epiphyseal border and die as matrix calcifies.
- Osteoblasts replace cartilage with bone.
- Process leads to temporary widening of epiphyseal plate.
- Osteoclasts remove dead chondrocytes and calcified matrix.
- Osteoblasts create new bone.
- Epiphyseal plate maintains original thickness.
Growth in Thickness
- New bone is added by osteoblasts in the periosteum to the outer surface of existing bone.
- Osteoclasts concurrently remove bone tissue on the inside, adjacent to the marrow cavity.
- Marrow cavity increases proportionally with bone circumference.
Bone Remodeling
- Bone constituents are constantly renewed through concurrent bone deposition and resorption.
- This maintains mechanical effectiveness and plasma calcium levels.
- Osteoclasts attach to osteoid (ECM), forming ruffled membranes to increase surface area for contact with bone.
- Osteoclasts secrete organic acids and enzymes, dissolving hydroxyapatite and breaking down ECM.
- Osteoblasts migrate into cavities and create new bone.
- Formation and resorption rates are about equal, maintaining consistent bone mass in adults.
- Remodeling facilitates changes in shape, material, damage repair, and mineral ion release.
RANK Ligand and Osteoprotegerin
- RANK ligand stimulates osteoclast activity.
- Osteoprotegerin suppresses osteoclast activity.
- Balance between these factors determines bone density.
Haversian System (Osteons)
- Compact bone is comprised of units called osteons.
- Osteons have concentric layers (lamellae) of osteocytes.
- A central canal contains blood vessels and nerves.
- Osteoblasts line the outer and inner surfaces of the central canal.
- Osteoclasts are located on surfaces where absorption is occurring.
- Osteons run parallel to the long axis of bone.
Osteocytic-Osteoblastic Bone Membrane (OOBM)
- Network of fluid-filled canals (canaliculi) allows exchange of substances between osteocytes and circulation.
- Cytoplasmic extensions of osteoblasts and osteocytes connect via gap junctions.
- This network separates mineralized bone from blood vessels.
Maintenance of Plasma Calcium Levels
- Bone has a stable mineral pool and a readily available labile pool in bone fluid.
- Ca2+ is exchanged quickly via PTH-activated pumps between labile pool and plasma (fast exchange).
- Ca2+ is exchanged slowly via PTH-induced dissolution of mineralized bone (slow exchange).
Further Reading
- References are provided for further study.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.