Podcast
Questions and Answers
Which hormone is released by S-cells and is responsible for reducing motility during digestion?
Which hormone is released by S-cells and is responsible for reducing motility during digestion?
- Glucagon
- Pancreatic peptide YY
- Secretin (correct)
- Somatostatin
What type of digestion involves physically cutting and crushing food to increase its surface area?
What type of digestion involves physically cutting and crushing food to increase its surface area?
- Biological digestion
- Chemical digestion
- Metabolic digestion
- Mechanical digestion (correct)
What is the primary function of cholecystokinin in the digestive process?
What is the primary function of cholecystokinin in the digestive process?
- Absorbing nutrients
- Inhibiting stomach acid secretion
- Stimulating gastric motility
- Triggering the release of pancreatic enzymes (correct)
Which statement accurately describes somatostatin?
Which statement accurately describes somatostatin?
What effect do peptides or free fatty acids have on digestion?
What effect do peptides or free fatty acids have on digestion?
What is the primary function of the gastrointestinal tract?
What is the primary function of the gastrointestinal tract?
Which component is NOT involved in regulating gut motility?
Which component is NOT involved in regulating gut motility?
Which function does the gut microbiome primarily serve?
Which function does the gut microbiome primarily serve?
Which of the following statements about gut dysbiosis is true?
Which of the following statements about gut dysbiosis is true?
Which types of substances does the gastrointestinal tract help absorb?
Which types of substances does the gastrointestinal tract help absorb?
Which vitamins require the incorporation into micelles for absorption?
Which vitamins require the incorporation into micelles for absorption?
The relationship between dietary factors and the microbiome suggests that:
The relationship between dietary factors and the microbiome suggests that:
In which part of the intestine is the majority of vitamin B12 absorbed?
In which part of the intestine is the majority of vitamin B12 absorbed?
What is the role of enteric hormones in GI function?
What is the role of enteric hormones in GI function?
What is a significant consequence of taking antibiotics on the gut microbiome?
What is a significant consequence of taking antibiotics on the gut microbiome?
How is iron transported into enterocytes during absorption?
How is iron transported into enterocytes during absorption?
What is the approximate number of cells in the human microbiome?
What is the approximate number of cells in the human microbiome?
What term is used to describe the collection of all organisms living in and on the human body?
What term is used to describe the collection of all organisms living in and on the human body?
What can happen if food is transported too quickly through the digestive system?
What can happen if food is transported too quickly through the digestive system?
Which hormone is released by I-cells in response to certain stimuli during digestion?
Which hormone is released by I-cells in response to certain stimuli during digestion?
What is a potential consequence of food staying in the stomach for too long?
What is a potential consequence of food staying in the stomach for too long?
What type of cells respond to mechanical stimulation such as distention in the gastrointestinal tract?
What type of cells respond to mechanical stimulation such as distention in the gastrointestinal tract?
What is one effect of the presence of peptides or free fatty acids in the digestive system?
What is one effect of the presence of peptides or free fatty acids in the digestive system?
What is the main function of the muscularis layer in the GI tract?
What is the main function of the muscularis layer in the GI tract?
Which type of epithelium is typically found in high-absorption areas of the small intestine?
Which type of epithelium is typically found in high-absorption areas of the small intestine?
What role do goblet cells play in the GI tract?
What role do goblet cells play in the GI tract?
Which structure is responsible for the majority of secretion in the submucosa layer of the GI tract?
Which structure is responsible for the majority of secretion in the submucosa layer of the GI tract?
What is a key function of the serosa/adventitia layer in the GI tract?
What is a key function of the serosa/adventitia layer in the GI tract?
How do microvilli contribute to the function of the mucosa in the GI tract?
How do microvilli contribute to the function of the mucosa in the GI tract?
Which layer of the GI tract wall contains a large plexus of neurons and plays an immune role?
Which layer of the GI tract wall contains a large plexus of neurons and plays an immune role?
What type of cell is primarily responsible for the endocrine functions in the mucosa of the GI tract?
What type of cell is primarily responsible for the endocrine functions in the mucosa of the GI tract?
What is a key function of the gut microbiome related to immune health?
What is a key function of the gut microbiome related to immune health?
Which of the following influences the development of an infant's gut microbiome the most?
Which of the following influences the development of an infant's gut microbiome the most?
What change is observed in the gut microbiota of formula-fed infants compared to breastfed infants?
What change is observed in the gut microbiota of formula-fed infants compared to breastfed infants?
By what age does the composition of a child's gut microbiome become similar to that of an adult?
By what age does the composition of a child's gut microbiome become similar to that of an adult?
Which factor is NOT mentioned as influencing the composition of the gut microbiota?
Which factor is NOT mentioned as influencing the composition of the gut microbiota?
What percentage of AAD cases is accounted for by C.difficile?
What percentage of AAD cases is accounted for by C.difficile?
Which condition is NOT associated with antibiotic use in childhood?
Which condition is NOT associated with antibiotic use in childhood?
Which component is reduced in the gut microbiome due to dysbiosis?
Which component is reduced in the gut microbiome due to dysbiosis?
What is a symptom of pseudomembranous colitis caused by C.difficile?
What is a symptom of pseudomembranous colitis caused by C.difficile?
Which of the following indicates an increase in white blood cells in the context of C.difficile infections?
Which of the following indicates an increase in white blood cells in the context of C.difficile infections?
In which condition is a dysbiotic gut microbiome primarily thought to play a role?
In which condition is a dysbiotic gut microbiome primarily thought to play a role?
What is the effect of reduced richness in gut microbiome diversity?
What is the effect of reduced richness in gut microbiome diversity?
Which of the following best describes the primary effect of antibiotics on the gut microbiome?
Which of the following best describes the primary effect of antibiotics on the gut microbiome?
What is the primary function of the hepatic portal vein?
What is the primary function of the hepatic portal vein?
Which veins combine to form the hepatic portal vein?
Which veins combine to form the hepatic portal vein?
What is the correct order of blood flow involving the hepatic portal vein?
What is the correct order of blood flow involving the hepatic portal vein?
Which structure primarily receives blood from the hepatic portal vein?
Which structure primarily receives blood from the hepatic portal vein?
Which statement accurately describes the blood supplied by the hepatic portal vein?
Which statement accurately describes the blood supplied by the hepatic portal vein?
What type of diet is associated with a higher percentage of Prevotella in the infant microbiota?
What type of diet is associated with a higher percentage of Prevotella in the infant microbiota?
Which short-chain fatty acid is produced during fermentation of indigestible carbohydrates?
Which short-chain fatty acid is produced during fermentation of indigestible carbohydrates?
How do short-chain fatty acids (SCFAs) contribute to intestinal health?
How do short-chain fatty acids (SCFAs) contribute to intestinal health?
What is a potential risk factor associated with trimethylamine oxide (TMAO)?
What is a potential risk factor associated with trimethylamine oxide (TMAO)?
What metabolic function does the gut microbiome influence related to appetite?
What metabolic function does the gut microbiome influence related to appetite?
What is a key role of bile acids modified by the gut microbiome?
What is a key role of bile acids modified by the gut microbiome?
Which bacterial activity is responsible for producing indoles that influence the immune response?
Which bacterial activity is responsible for producing indoles that influence the immune response?
What correlation exists between the presence of different bacterial species and intestinal integrity?
What correlation exists between the presence of different bacterial species and intestinal integrity?
Which hormone is primarily responsible for increasing stomach acid secretion?
Which hormone is primarily responsible for increasing stomach acid secretion?
What is the main function of secretin in the gastrointestinal system?
What is the main function of secretin in the gastrointestinal system?
Which type of enteroendocrine cell is located in the stomach and releases histamine?
Which type of enteroendocrine cell is located in the stomach and releases histamine?
Closed enteroendocrine cells differ from open cells in that they:
Closed enteroendocrine cells differ from open cells in that they:
How do motilin's main functions contribute to digestive processes?
How do motilin's main functions contribute to digestive processes?
Which hormone is involved in regulating satiety and also promotes insulin secretion?
Which hormone is involved in regulating satiety and also promotes insulin secretion?
What role does the muscularis mucosa serve in the gastrointestinal tract?
What role does the muscularis mucosa serve in the gastrointestinal tract?
Enteroendocrine cells generally serve what primary role in the digestive system?
Enteroendocrine cells generally serve what primary role in the digestive system?
Which statement accurately describes open enteroendocrine cells?
Which statement accurately describes open enteroendocrine cells?
Which type of enteroendocrine cell is primarily responsible for stimulating enzyme secretion in the pancreas?
Which type of enteroendocrine cell is primarily responsible for stimulating enzyme secretion in the pancreas?
Which type of movement is specifically responsible for the propulsion of food through the gastrointestinal tract?
Which type of movement is specifically responsible for the propulsion of food through the gastrointestinal tract?
What is the primary role of Enteric Nervous System (ENS) in the gut?
What is the primary role of Enteric Nervous System (ENS) in the gut?
Which statement best describes the relationship between bacteria in the gut microbiome and human physiology?
Which statement best describes the relationship between bacteria in the gut microbiome and human physiology?
Which of the following factors is least likely to influence the composition of the gut microbiota?
Which of the following factors is least likely to influence the composition of the gut microbiota?
What role do hormones play in gastrointestinal motility?
What role do hormones play in gastrointestinal motility?
Which condition is primarily linked to an imbalance in the gut microbiome?
Which condition is primarily linked to an imbalance in the gut microbiome?
Which structure in the GI tract is most involved in nutrient absorption?
Which structure in the GI tract is most involved in nutrient absorption?
What is a potential consequence of prolonged antibiotic use on gut health?
What is a potential consequence of prolonged antibiotic use on gut health?
What is the primary role of interstitial cells of Cajal (ICC) in the gastrointestinal tract?
What is the primary role of interstitial cells of Cajal (ICC) in the gastrointestinal tract?
Which movement is characterized by waves of smooth muscle contractions that propel food bolus through the GI tract?
Which movement is characterized by waves of smooth muscle contractions that propel food bolus through the GI tract?
In what part of the gastrointestinal tract does segmentation primarily occur?
In what part of the gastrointestinal tract does segmentation primarily occur?
What is a suspected function of the migrating motor complex (MMC)?
What is a suspected function of the migrating motor complex (MMC)?
Which system is primarily involved in autonomically regulating GI motility?
Which system is primarily involved in autonomically regulating GI motility?
What effect does norepinephrine have on the excitability of smooth muscle in the gastrointestinal tract?
What effect does norepinephrine have on the excitability of smooth muscle in the gastrointestinal tract?
Which structure is responsible for facilitating communication between the CNS and the ENS?
Which structure is responsible for facilitating communication between the CNS and the ENS?
What is stimulated by the distention of smooth muscle cells in the gastrointestinal tract?
What is stimulated by the distention of smooth muscle cells in the gastrointestinal tract?
How does the sympathetic nervous system generally affect gastrointestinal motility?
How does the sympathetic nervous system generally affect gastrointestinal motility?
Which cell type is primarily responsible for the regulatory processes within the submucosal plexus?
Which cell type is primarily responsible for the regulatory processes within the submucosal plexus?
What is the primary bacterial species composition in the microbiota of infants on a starch, fiber, and plant diet?
What is the primary bacterial species composition in the microbiota of infants on a starch, fiber, and plant diet?
Which short-chain fatty acid (SCFA) is produced through the fermentation of dietary fibers by gut microbiota?
Which short-chain fatty acid (SCFA) is produced through the fermentation of dietary fibers by gut microbiota?
What impact do short-chain fatty acids (SCFAs) have on intestinal integrity?
What impact do short-chain fatty acids (SCFAs) have on intestinal integrity?
Which of the following metabolites is produced from the metabolism of choline, phosphatidylcholine, and L-carnitine?
Which of the following metabolites is produced from the metabolism of choline, phosphatidylcholine, and L-carnitine?
What is a consequence of the absence of Prevotella in the microbiota of infants with a diet high in sugar, starch, and animal protein?
What is a consequence of the absence of Prevotella in the microbiota of infants with a diet high in sugar, starch, and animal protein?
How do bile acids modified by the gut microbiome influence metabolism?
How do bile acids modified by the gut microbiome influence metabolism?
What role do indoles play in the gut microbiome?
What role do indoles play in the gut microbiome?
What primary effect do SCFAs have on epithelial cells in the gut?
What primary effect do SCFAs have on epithelial cells in the gut?
What is the primary function of salivary amylase in the digestive process?
What is the primary function of salivary amylase in the digestive process?
What role does the Na+/K+ pump play in carbohydrate absorption?
What role does the Na+/K+ pump play in carbohydrate absorption?
Which transporter is responsible for the absorption of dipeptides and tripeptides into enterocytes?
Which transporter is responsible for the absorption of dipeptides and tripeptides into enterocytes?
What characterizes the absorption of fat greater than 10-12 carbons long?
What characterizes the absorption of fat greater than 10-12 carbons long?
What is the consequence of overly rapid transit of chyme through the digestive system?
What is the consequence of overly rapid transit of chyme through the digestive system?
Which molecule can pass through enterocytes without modification?
Which molecule can pass through enterocytes without modification?
Which active transporters are involved in the absorption of nucleic acids?
Which active transporters are involved in the absorption of nucleic acids?
How are absorbed amino acids released into the bloodstream?
How are absorbed amino acids released into the bloodstream?
What condition can result from impaired fat absorption, leading to excessive fat in the stool?
What condition can result from impaired fat absorption, leading to excessive fat in the stool?
Which carbohydrates can be transported across the epithelial cells of the small intestine?
Which carbohydrates can be transported across the epithelial cells of the small intestine?
What is the role of the swallowing center in the pharyngeal stage of swallowing?
What is the role of the swallowing center in the pharyngeal stage of swallowing?
What is the primary consequence of secondary peristalsis in the esophagus?
What is the primary consequence of secondary peristalsis in the esophagus?
What is the physiological mechanism of the lower esophageal sphincter (LES) during peristalsis?
What is the physiological mechanism of the lower esophageal sphincter (LES) during peristalsis?
What characterizes achalasia in terms of esophageal motility?
What characterizes achalasia in terms of esophageal motility?
Which condition results from impaired smooth muscle relaxation at the lower esophageal sphincter?
Which condition results from impaired smooth muscle relaxation at the lower esophageal sphincter?
What might cause dysphagia due to obstructive disorders?
What might cause dysphagia due to obstructive disorders?
Which disorder is characterized by high-amplitude contractions and intense chest pain?
Which disorder is characterized by high-amplitude contractions and intense chest pain?
What is the significance of barium swallow imaging in diagnosing esophageal conditions?
What is the significance of barium swallow imaging in diagnosing esophageal conditions?
Which type of esophagitis is often associated with immunosuppression?
Which type of esophagitis is often associated with immunosuppression?
What type of esophageal pathology results in difficulty swallowing due to muscular dysfunction?
What type of esophageal pathology results in difficulty swallowing due to muscular dysfunction?
What condition is often characterized by a grayish-white pseudomembrane on an erythematous base?
What condition is often characterized by a grayish-white pseudomembrane on an erythematous base?
What is the result of the relaxation of the lower esophageal sphincter (LES)?
What is the result of the relaxation of the lower esophageal sphincter (LES)?
Which nerve is primarily responsible for sending afferent sensory input during swallowing?
Which nerve is primarily responsible for sending afferent sensory input during swallowing?
What is a key characteristic of diffuse esophageal spasm?
What is a key characteristic of diffuse esophageal spasm?
Study Notes
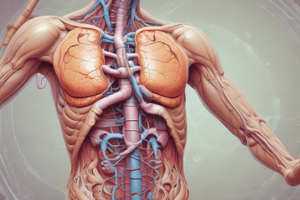
Overview of Gastrointestinal Tract
- The gastrointestinal (GI) tract manages food transport and nutrient absorption.
- Approximately 60 tonnes of food pass through the GI tract over a human lifetime.
- Functions include digestion, absorption, and immune responses to environmental factors.
Gut Physiology
- Gut motility is regulated by interstitial cells of Cajal (ICC), smooth muscle cells, and both enteric and central nervous systems.
- Hormonal secretions impacting motility include:
- Promoting motility: Cholecystokinin (I-cells), Serotonin (enterochromaffin cells), Gastrin (G-cells), Motilin (Mo-cells), Insulin (beta-pancreatic cells)
- Reducing motility: Secretin (S-cells), Somatostatin (D-cells), Pancreatic peptide YY (pancreatic cells), Glucagon (alpha-pancreatic cells)
Digestion
- Digestion entails breaking down macromolecules via mechanical (chewing, churning) and chemical processes.
- Mechanical Digestion: Involves reduction of food particles to increase the surface area for chemical digestion.
- Chemical Digestion: Enzymatic breakdown that allows nutrient absorption.
Absorption Processes
- Fat-soluble vitamins (A, D, E, K) require micelle formation for absorption, mainly occurring in the duodenum; Vitamin B12 is absorbed in the ileum.
- B-vitamins and Vitamin C are absorbed using Na+ cotransporters.
- Iron absorption takes place in the duodenum through the divalent metal transporter 1 (DMT1).
The Human Microbiome
- The microbiome comprises ~10^14 cells, including bacteria, viruses, and fungi, with a virus-to-bacteria ratio of ~5:1.
- It plays a significant role in digestion, nutrient absorption, and overall intestinal health.
- A balanced microbiome is crucial for preventing gut dysbiosis and associated health issues.
General GI Tract Histology
- The GI tract's structure includes four main layers:
- Mucosa: Responsible for absorption and secretion, contains epithelial cells, goblet cells (mucus secretion), and enteroendocrine cells.
- Submucosa: Contains blood vessels and neurons (Meissner’s plexus).
- Muscularis: Composed of smooth muscle layers responsible for propulsion; contains Auerbach’s plexus.
- Serosa/Adventitia: Connective tissue providing support and mobility.
Pathological Implications
- Gut dysbiosis can lead to various digestive disorders and health issues, highlighting the importance of a balanced microbiome.
- Dietary factors and antibiotic use significantly influence microbiome composition and health.
Gut Microbiome Functions
- Harvests energy from undigested nutrients, aiding nutrient absorption.
- Strengthens gut integrity and shapes intestinal epithelium structure.
- Regulates immune function and intestinal motility.
- Offers protection against pathogenic microbes.
- Produces essential nutrients, including Vitamin K2 and short-chain fatty acids (SCFAs).
- Functions as an endocrine organ, influencing various bodily processes.
Gut Microbiome Development
- Birth method influences initial gut microbiota:
- C-section leads to lower Bacteroides and higher Clostridium species.
- Vaginal birth reflects maternal microbiota characteristics.
- Initial nutrition impacts gut flora:
- Breastfed infants show high levels of Bifidobacterium.
- Formula-fed infants exhibit lower Bifidobacterium and altered E. coli and Clostridium difficile ratios.
- Undernourished infants may have increases in enteropathogens like Enterobacteriaceae.
- By age 2.5, a child's gut flora resembles that of an adult, remaining stable with minor fluctuations throughout life.
Diet and Gut Microbiome
- Genetic, dietary, and medication factors influence gut microbiota composition.
- Dietary examples:
- Starch, fiber, and plant-rich diets yield 10.1% Actinobacteria and 57.7% Bacteroidetes in infants.
- A diet high in sugar, starch, and animal protein leads to lower Actinobacteria (6.7%) and Bacteroidetes (22.4%) with absent Prevotella.
Short-Chain Fatty Acids (SCFAs)
- Produced during fermentation of indigestible carbohydrates by gut microbiota.
- Key SCFAs include acetate, propionate, and butyrate.
- Promote intestinal integrity through regulating pH, mucus production, providing epithelial cell fuel, and modifying immune functions.
- Influence metabolism aspects such as appetite regulation, energy expenditure, glucose homeostasis, and immunomodulation.
Microbiome Metabolites
- Trimethylamine (TMA): Metabolized from choline and L-carnitine, linked to atherosclerosis and thrombosis risk via conversion to TMAO.
- Bile Acids: Liver-produced substances modified by gut microbiota, correlated with energy metabolism changes, including cholesterol and insulin sensitivity.
- Indoles: Derived from tryptophan metabolism, play a role in maintaining the intestinal barrier and influencing immune responses.
Gut Microbiome and Intestinal Integrity
- Bacterial diversity correlates with epithelial function and structure.
- Non-pathogenic E. difficile accounts for 10-25% of antibiotic-associated diarrhea (AAD) cases, with symptoms ranging from mild diarrhea to severe pseudomembranous colitis.
- Childhood antibiotic use is associated with various health issues (asthma, diabetes, IBD, mental illness) attributed to dysbiosis, resulting in reduced microbial richness and shifts in bacterial populations.
Enteroendocrine Cells (DNES)
- Located in the stomach and small intestine; involved in hormonal secretion.
- Open and closed cells regulate hormonal release through different mechanisms (e.g., sensing luminal contents vs. other stimuli).
- Key enteroendocrine cells and their functions include:
- D cells: Somatostatin release, inhibiting nearby hormone secretion.
- G cells: Gastrin secretion for increasing stomach acid release.
- I cells: CCK secretion, stimulating pancreatic enzymes and gallbladder contraction.
- L cells: Glucagon-like peptide for insulin secretion and satiety.
- S cells: Secretin for bicarbonate and water secretion from the pancreas.
Abdominal Venous Vasculature Overview
- Inferior mesenteric vein combines with splenic vein to form hepatic portal vein.
- Hepatic portal vein transports nutrient-rich blood from abdominal organs to the liver, facilitating nutrient metabolism and detoxification processes.
Swallowing and Esophageal Mechanics
- The trachea closes during swallowing, inhibiting respiration.
- Vocal cords approximate, the larynx raises, and the epiglottis covers the vocal cords.
- The upper esophageal sphincter (UES) relaxes during swallowing.
- Pharyngeal peristalsis moves food toward the stomach.
Nervous Control of Swallowing
- Swallowing is regulated by the swallowing center located in the medulla.
- Sensory input from the pharynx and esophagus activates the swallowing center.
- The swallowing center coordinates activities through vagal nuclei while inhibiting the respiratory center.
- Pharyngeal phase of swallowing occurs within 2 seconds, briefly interrupting respiration.
Esophageal Movements
- Secondary peristalsis occurs in response to retained food or reflux, continuing until the esophagus is cleared.
- Initiated by intrinsic neural circuits and vagal afferent fibers.
Lower Esophageal Sphincter (LES)
- The LES, located 1-2 cm below the diaphragm, remains tonically constricted.
- During peristalsis, the LES relaxes to allow food entry into the stomach, preventing reflux.
Esophageal Manometry Insights
- High resting pressure of the UES contrasts with low resting pressure of the LES.
- Post-food passage, the LES exhibits higher pressures due to activity of NO and VIP-secreting vagal branches.
Pathologies of the Esophagus
- Common conditions range from dysphagia (difficulty swallowing) to inflammatory, metaplastic/neoplastic, and vascular diseases.
- Motility disorders include nutcracker esophagus, resulting in intense chest pain, and achalasia, characterized by impaired LES relaxation.
Achalasia Features
- Achalasia presents with dysphagia, chest pain, and regurgitation.
- Primary achalasia: Idiopathic failure of inhibitory neurons leading to increased LES tone.
- Secondary achalasia: Caused by diabetes or infections like Trypanosoma cruzi, leading to esophageal dilatation and failure of peristalsis.
Imaging and Studies
- Barium swallow studies visualize motility disorders such as diffuse esophageal spasm and achalasia.
- Manometry studies provide insights into pressure variations in the esophagus.
Esophagitis
- Infectious esophagitis may indicate immunosuppression, commonly caused by HSV, CMV, or fungi like candidiasis.
- Autoimmune disorders like Crohn's disease or scleroderma can also impact the esophagus.
Gastrointestinal Tract Overview
- The GI tract transports approximately 60 tonnes of food over a lifetime, aiding in digestion and absorption.
- Functions include decontamination of food and maintaining non-human cell interactions with the immune system.
GI Motility
- Three primary movements in the GI tract: peristalsis (propels food), segmentation (mixes food for absorption), and migrating motor complex (cleanses intestines).
- Interstitial cells of Cajal serve as pacemakers, coordinating muscle contractions.
Enteric Nervous System (ENS)
- ENS composed of sensory, motor, and interneurons is organized into submucosal and myenteric plexuses, regulating GI motility and secretions.
- The CNS influences GI function through vagus and pelvic splanchnic nerves.
Nutrient Transport in the GI Tract
- Digestion and absorption occur primarily in the small intestine, where chemical digestion is crucial.
- Carbohydrates are absorbed as monosaccharides via specific transporters like SGLT1 and GLUT-5.
Absorption Mechanisms
- Proteins, nucleic acids, and fats undergo specific digestion to permit absorption via various mechanisms.
- Fats are absorbed as chylomicrons through passive diffusion, entering lymphatics.
Short-Chain Fatty Acids (SCFA)
- SCFAs, produced during fiber fermentation by gut microbiota, play roles in intestinal integrity, immune function, and metabolism.
Gut Microbiome Connections
- The balance of bacterial species affects epithelial function and overall health.
- Dietary factors shape the microbiome, influencing absorption and potential pathological conditions.
Dietary and Antibiotic Influences
- Diet impacts microbiome diversity and functionality.
- Antibiotics can disrupt microbial balance, influencing gut health.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the fundamentals of the gastrointestinal tract, including gut physiology, motility, digestion, absorption, and regulation. Additionally, it explores the microbiome's role in health and its relationship with human physiology. Prepare to test your understanding of these essential concepts.