Podcast
Questions and Answers
During which kind of potentials do significant quantities of calcium ions enter the fibers and cause most of the contraction?
During which kind of potentials do significant quantities of calcium ions enter the fibers and cause most of the contraction?
- Synaptic potentials
- Action potentials
- Slow wave potentials
- Spike potentials (correct)
What is the term for the nervous system that lies entirely in the wall of the gut?
What is the term for the nervous system that lies entirely in the wall of the gut?
- Central nervous system
- Enteric nervous system (correct)
- Sympathetic nervous system
- Parasympathetic nervous system
How many plexuses make up the enteric nervous system?
How many plexuses make up the enteric nervous system?
- One
- Three
- Two (correct)
- Four
What is the primary function of the myenteric plexus?
What is the primary function of the myenteric plexus?
What is the function of some neurons in the myenteric plexus?
What is the function of some neurons in the myenteric plexus?
What is the function of the submucosal plexus?
What is the function of the submucosal plexus?
What is the origin of many sensory signals in the GI tract?
What is the origin of many sensory signals in the GI tract?
How is the parasympathetic supply to the gut divided?
How is the parasympathetic supply to the gut divided?
What is the primary function of the alimentary tract?
What is the primary function of the alimentary tract?
What is the correct order of the layers of the GIT wall from outside towards the lumen?
What is the correct order of the layers of the GIT wall from outside towards the lumen?
What is the typical range of voltage of slow waves in the GI smooth muscle?
What is the typical range of voltage of slow waves in the GI smooth muscle?
What is the normal resting membrane potential in the smooth muscle fibers of the gut?
What is the normal resting membrane potential in the smooth muscle fibers of the gut?
What happens when the resting membrane potential of the GI smooth muscle becomes more positive than about -40 millivolts?
What happens when the resting membrane potential of the GI smooth muscle becomes more positive than about -40 millivolts?
What is the effect of NE or EP on the smooth muscle fiber membrane?
What is the effect of NE or EP on the smooth muscle fiber membrane?
What is the effect of acetylcholine on the smooth muscle fiber membrane?
What is the effect of acetylcholine on the smooth muscle fiber membrane?
What ions enter the smooth muscle fiber during slow waves?
What ions enter the smooth muscle fiber during slow waves?
What triggers the relaxation of the internal anal sphincter?
What triggers the relaxation of the internal anal sphincter?
What is the primary function of secretory glands in the GIT?
What is the primary function of secretory glands in the GIT?
What stimulates the secretion of digestive enzymes in the GIT?
What stimulates the secretion of digestive enzymes in the GIT?
What is the effect of sympathetic stimulation on GIT glandular secretion?
What is the effect of sympathetic stimulation on GIT glandular secretion?
What is the composition of esophageal secretions?
What is the composition of esophageal secretions?
What is the location of the glands that secrete mucus for lubrication in the esophagus?
What is the location of the glands that secrete mucus for lubrication in the esophagus?
What is the parasympathetic reflex involved in?
What is the parasympathetic reflex involved in?
What is the role of the pelvic parasympathetic nerve fibers?
What is the role of the pelvic parasympathetic nerve fibers?
How many phases of gastric secretion are there?
How many phases of gastric secretion are there?
What is the primary function of oxyntic glands?
What is the primary function of oxyntic glands?
What is the main function of pancreatic amylase?
What is the main function of pancreatic amylase?
What is the role of bile in fat digestion?
What is the role of bile in fat digestion?
What is the function of carboxypolypeptidase?
What is the function of carboxypolypeptidase?
What is the function of pancreatic lipase?
What is the function of pancreatic lipase?
What is the other important function of bile besides fat digestion?
What is the other important function of bile besides fat digestion?
What is the primary function of pancreatic juice?
What is the primary function of pancreatic juice?
What initiates enterogastric inhibitory reflexes?
What initiates enterogastric inhibitory reflexes?
What is the primary site of digestion and absorption?
What is the primary site of digestion and absorption?
What is the function of the enzymes secreted by the brush border of the villi?
What is the function of the enzymes secreted by the brush border of the villi?
What is the result of the intrinsic defecation reflex?
What is the result of the intrinsic defecation reflex?
What is the location of the myenteric plexus in the intrinsic defecation reflex?
What is the location of the myenteric plexus in the intrinsic defecation reflex?
What is the function of the peptidases in the small intestine?
What is the function of the peptidases in the small intestine?
What is the result of the stimulation of the pyloric pump by food in the duodenum?
What is the result of the stimulation of the pyloric pump by food in the duodenum?
What is the surface area of the small intestine comparable to?
What is the surface area of the small intestine comparable to?
Flashcards are hidden until you start studying
Study Notes
Gastrointestinal Physiology
- The alimentary tract provides the body with a continual supply of water, electrolytes, vitamins, and nutrients through:
- Movement of food through the GIT
- Secretion of digestive juices and digestion of food
- Absorption of water, electrolytes, vitamins, and digestive products
- Circulation of blood through the GI organs to carry away absorbed substances
- Control of all these functions by local, nervous, and hormonal systems
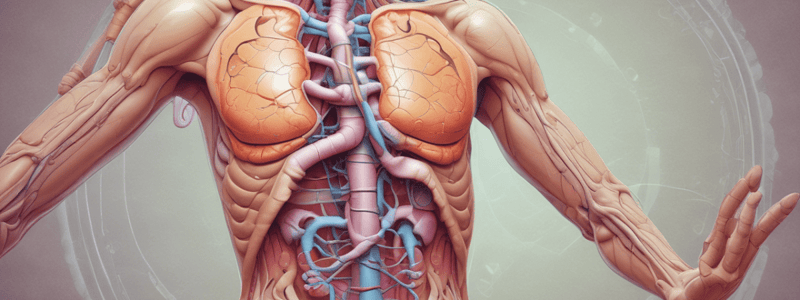
Physiologic Anatomy of the GI Wall
- The GI wall consists of five layers from outside to lumen:
- Serosa
- Longitudinal muscle layer
- Circular muscle layer
- Submucosa
- Mucosa
Electrical Activity of Gastrointestinal Smooth Muscle
- Slow waves:
- Are slow, undulating changes in resting membrane potential
- Intensity varies between 5 and 15 millivolts
- Spike potentials:
- Are true action potentials
- Occur automatically when resting membrane potential becomes more positive than about −40 millivolts
- Normal resting membrane potential in smooth muscle fibers is between −50 and −60 millivolts
- Factors that depolarize the membrane:
- Stretching of the muscle
- Stimulation by acetylcholine
- Stimulation by several GI hormones
- Factors that hyperpolarize the membrane:
- Effect of NE or EP on the fiber membrane
- Stimulation of the sympathetic nerves that secrete mainly NE at their endings
Neural Control of Gastrointestinal Function—Enteric Nervous System
- The GI has its own nervous system called the enteric nervous system (ENS)
- The ENS lies entirely in the wall of the gut, beginning in the esophagus and extending to the anus
- The ENS is composed of two plexuses:
- Myenteric plexus (outer plexus) lying between the longitudinal and circular muscle layers
- Submucosal plexus (inner plexus) lying in the submucosa
- The myenteric plexus controls mainly GI movements
- The submucosal plexus controls mainly GI secretion and local blood flow
- The ENS can function independently, but stimulation by the parasympathetic and sympathetic systems can greatly enhance or inhibit GI functions
Autonomic Control of the Gastrointestinal Tract
- The parasympathetic supply to the gut is divided into cranial and sacral divisions
- Powerful factors that inhibit stomach emptying (duodenal factors):
- Degree of distention of the duodenum
- Presence of any degree of irritation of the duodenal mucosa
- Degree of acidity of the chyme
- Degree of osmolality of the chyme
- Presence of certain breakdown products in the chyme
Small Intestine Function
- Digestion: enzymes are intracellular (disaccharidases and aminopeptidases)
- Absorption: completed in the small intestine, large surface area (as large as a tennis court area)
- Secretion: secretion of digestive enzymes by the brush border of the villi
- Motility: movement of food through the small intestine
Secretion of Digestive Enzymes
- The enterocytes of the mucosa, especially those that cover the villi, contain digestive enzymes that digest specific food substances while they are being absorbed through the epithelium
- These enzymes include:
- Peptidases for the splitting of small polypeptides into amino acids
- Disaccharidases that break down disaccharides into monosaccharides
- Small amounts of lipases for the digestion of fat
Defecation Reflexes
- There are two types of defecation reflexes:
- Intrinsic reflex mediated by the local enteric nervous system in the rectal wall
- Parasympathetic reflex that involves the sacral segments of the spinal cord
Secretory Functions of the GIT
- Secretory glands have two primary functions:
- Secrete digestive enzymes in most areas of the GIT
- Provide mucus for lubrication and protection of all parts of the GIT
Basic Mechanisms of Stimulation of the GIT Glands
- Contact of food with the epithelium stimulates secretion (direct contact stimulation of the surface glandular cells by the food)
- Parasympathetic stimulation increases the GIT glandular secretion rate
- Sympathetic stimulation has a dual effect (sympathetic stimulation alone decreases secretion, but parasympathetic stimulation increases the secretion)
Esophageal Secretions
- Esophageal secretions are entirely mucous and provide lubrication for swallowing
- The main body of the esophagus is lined with many simple mucous glands
Pancreatic Secretion
- The pancreatic digestive enzymes are secreted by pancreatic acini and large volumes of sodium bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini
- The combined product (enzymes + sodium bicarbonate) flows through a long pancreatic duct that joins the common bile duct
- Pancreatic enzymes for digesting proteins:
- Trypsin
- Chymotrypsin
- Carboxypolypeptidase
- Pancreatic enzymes for digesting carbohydrates:
- Pancreatic amylase
- Pancreatic enzymes for digesting fat:
- Pancreatic lipase
- Cholesterol esterase
- Phospholipase
Secretion of Bile by the Liver
- Bile serves two important functions:
- Aids in fat digestion and absorption by emulsifying fat particles and aiding in absorption of digested fat end products
- Serves as a means for excretion of several important waste products from the blood
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.