Podcast
Questions and Answers
Which layer of an artery or vein is primarily responsible for vasodilation and vasoconstriction?
Which layer of an artery or vein is primarily responsible for vasodilation and vasoconstriction?
- Tunica externa (tunica adventitia)
- Tunica interna (tunica intima)
- Vasa vasorum
- Tunica media (correct)
A patient is diagnosed with a condition affecting the endothelium of their blood vessels. Which function is most likely to be impaired?
A patient is diagnosed with a condition affecting the endothelium of their blood vessels. Which function is most likely to be impaired?
- Preventing blood clotting and secreting chemicals for vasomotion. (correct)
- Anchoring the vessel to surrounding tissues.
- Supplying blood to the outer half of the vessel wall.
- Strengthening the vessel wall to prevent rupture.
Which characteristic distinguishes distributing arteries from conducting arteries?
Which characteristic distinguishes distributing arteries from conducting arteries?
- Conducting arteries primarily control blood flow to specific organs.
- Distributing arteries have a thicker tunica media relative to their size. (correct)
- Conducting arteries are smaller in diameter.
- Distributing arteries have a higher proportion of elastic tissue.
A buildup of collagen and elastic fibers characterizes the internal and external elastic laminae within which type of artery?
A buildup of collagen and elastic fibers characterizes the internal and external elastic laminae within which type of artery?
What is the primary role of the recoil mechanism in large arteries during diastole?
What is the primary role of the recoil mechanism in large arteries during diastole?
Which characteristic is associated with metarterioles?
Which characteristic is associated with metarterioles?
Why can aneurysms be life-threatening?
Why can aneurysms be life-threatening?
What is the main function of the carotid sinuses?
What is the main function of the carotid sinuses?
How do carotid bodies respond to increasing levels of carbon dioxide in the blood?
How do carotid bodies respond to increasing levels of carbon dioxide in the blood?
A researcher is studying a unique type of capillary that allows proteins and large molecules to enter the circulation. Which type of capillary is the researcher most likely observing?
A researcher is studying a unique type of capillary that allows proteins and large molecules to enter the circulation. Which type of capillary is the researcher most likely observing?
Why are capillaries sometimes referred to as 'exchange vessels'?
Why are capillaries sometimes referred to as 'exchange vessels'?
What role do pericytes play in the function of continuous capillaries?
What role do pericytes play in the function of continuous capillaries?
What structural adaptation is present in fenestrated capillaries that allows for rapid filtration and absorption?
What structural adaptation is present in fenestrated capillaries that allows for rapid filtration and absorption?
What is the function of precapillary sphincters?
What is the function of precapillary sphincters?
How do veins accommodate a large blood volume with relatively low pressure?
How do veins accommodate a large blood volume with relatively low pressure?
In postcapillary venules, what structural characteristic allows leukocytes to easily enter the surrounding tissues?
In postcapillary venules, what structural characteristic allows leukocytes to easily enter the surrounding tissues?
What is the significance of venous valves found in medium veins?
What is the significance of venous valves found in medium veins?
What feature distinguishes venous sinuses from other types of veins?
What feature distinguishes venous sinuses from other types of veins?
How does the skeletal muscle pump aid in venous return?
How does the skeletal muscle pump aid in venous return?
In the simplest and most common circulatory route, how many capillary beds does blood pass through before returning to the heart from the arteries?
In the simplest and most common circulatory route, how many capillary beds does blood pass through before returning to the heart from the arteries?
What is a portal system in the circulatory system?
What is a portal system in the circulatory system?
Which type of anastomosis allows blood to bypass capillaries?
Which type of anastomosis allows blood to bypass capillaries?
If an artery constricts, what immediate effect does this have on blood pressure upstream and downstream of the constriction?
If an artery constricts, what immediate effect does this have on blood pressure upstream and downstream of the constriction?
Which of the following best describes the term 'perfusion'?
Which of the following best describes the term 'perfusion'?
Why is Mean Arterial Pressure (MAP) considered a more relevant indicator of cardiovascular stress than systolic or diastolic pressure alone?
Why is Mean Arterial Pressure (MAP) considered a more relevant indicator of cardiovascular stress than systolic or diastolic pressure alone?
Since pressure varies across the cardiac cycle, how does blood flow in arteries differ from that in capillaries and veins?
Since pressure varies across the cardiac cycle, how does blood flow in arteries differ from that in capillaries and veins?
What is the primary cause of arteriosclerosis?
What is the primary cause of arteriosclerosis?
What is the clinical measure for hypertension?
What is the clinical measure for hypertension?
Which organ has the largest influence on blood pressure except for the heart?
Which organ has the largest influence on blood pressure except for the heart?
Which variable primarily stems from plasma proteins and red blood cells?
Which variable primarily stems from plasma proteins and red blood cells?
What happens to pressure and flow as liquid travels further?
What happens to pressure and flow as liquid travels further?
If the body needs widespread vasoconstriction, which control mechanisms would be activated?
If the body needs widespread vasoconstriction, which control mechanisms would be activated?
If blood pressure decreases, how does the baroreflex respond to restore homeostasis?
If blood pressure decreases, how does the baroreflex respond to restore homeostasis?
What is the role of aortic bodies?
What is the role of aortic bodies?
How does Angiotensin II impact blood pressure?
How does Angiotensin II impact blood pressure?
How do Natriuretic peptides impact blood pressure?
How do Natriuretic peptides impact blood pressure?
What affect does epinephrine and norepinephrine cause in most vessels?
What affect does epinephrine and norepinephrine cause in most vessels?
What does increased CO2 in the brain do to blood flow?
What does increased CO2 in the brain do to blood flow?
How does blood flow to skeletal muscles change from rest to exertion?
How does blood flow to skeletal muscles change from rest to exertion?
How do the pulmonary arteries respond to hypoxia?
How do the pulmonary arteries respond to hypoxia?
Which of the following is the correct sequence of blood flow in the most common circulatory route?
Which of the following is the correct sequence of blood flow in the most common circulatory route?
What is the key characteristic of a portal system in the circulatory system?
What is the key characteristic of a portal system in the circulatory system?
What is the primary purpose of the vasa vasorum found in larger blood vessels?
What is the primary purpose of the vasa vasorum found in larger blood vessels?
Which layer of the blood vessel wall primarily contributes to strengthening the vessel and preventing it from rupturing due to blood pressure?
Which layer of the blood vessel wall primarily contributes to strengthening the vessel and preventing it from rupturing due to blood pressure?
What structural characteristic of postcapillary venules allows leukocytes to easily migrate into the surrounding tissues during inflammation?
What structural characteristic of postcapillary venules allows leukocytes to easily migrate into the surrounding tissues during inflammation?
What is the main function of the arterial sense organs?
What is the main function of the arterial sense organs?
What is the primary function of chemoreceptors located in the carotid and aortic bodies?
What is the primary function of chemoreceptors located in the carotid and aortic bodies?
Which feature is unique to the tunica externa (tunica adventitia)?
Which feature is unique to the tunica externa (tunica adventitia)?
What is the primary structural difference between continuous capillaries and fenestrated capillaries?
What is the primary structural difference between continuous capillaries and fenestrated capillaries?
What best describes the role of pericytes in continuous capillaries?
What best describes the role of pericytes in continuous capillaries?
How do veins accommodate a large blood volume with relatively low pressure compared to arteries?
How do veins accommodate a large blood volume with relatively low pressure compared to arteries?
Why are arterioles considered the most significant point of control over peripheral resistance and blood flow?
Why are arterioles considered the most significant point of control over peripheral resistance and blood flow?
What is the role of the skeletal muscle pump in venous return?
What is the role of the skeletal muscle pump in venous return?
What is the significance of the blood velocity decreasing in capillaries from the aorta?
What is the significance of the blood velocity decreasing in capillaries from the aorta?
How does total blood flow to the brain respond to increased carbon dioxide levels?
How does total blood flow to the brain respond to increased carbon dioxide levels?
What immediate effect does increased sympathetic activity have on blood vessels?
What immediate effect does increased sympathetic activity have on blood vessels?
What is the primary factor that allows blood to be rerouted according to the needs of the body?
What is the primary factor that allows blood to be rerouted according to the needs of the body?
During exercise, how does blood flow to skeletal muscles change relative to blood flow to the digestive organs?
During exercise, how does blood flow to skeletal muscles change relative to blood flow to the digestive organs?
What is the main effect of antidiuretic hormone (ADH) on blood pressure?
What is the main effect of antidiuretic hormone (ADH) on blood pressure?
How does the pulmonary artery respond to hypoxia to optimize ventialtion?
How does the pulmonary artery respond to hypoxia to optimize ventialtion?
What condition is most likely to be present when a patient has significant edema?
What condition is most likely to be present when a patient has significant edema?
Which is the most common cause of circulatory shock?
Which is the most common cause of circulatory shock?
During exercise, which blood vessels dilate in response to muscle metabolites such as lactate, CO2, and H⁺?
During exercise, which blood vessels dilate in response to muscle metabolites such as lactate, CO2, and H⁺?
In the brain, how does cerebral blood vessel dialation and constriction help maintain blood flow?
In the brain, how does cerebral blood vessel dialation and constriction help maintain blood flow?
What causes an increase in blood viscosity?
What causes an increase in blood viscosity?
Low R B Cs (anemia) or albumin (hypoproteinemia) does what to blood viscosity?
Low R B Cs (anemia) or albumin (hypoproteinemia) does what to blood viscosity?
What is the main purpose of the Autoregulation?
What is the main purpose of the Autoregulation?
If a specific artery constricts, what effect can be expected?
If a specific artery constricts, what effect can be expected?
Which of the following statements is true about blood pressure in the pulmonary circuit compared to the systemic circuit?
Which of the following statements is true about blood pressure in the pulmonary circuit compared to the systemic circuit?
What is true about anaphylactic blood shock?
What is true about anaphylactic blood shock?
Which of the following is a condition that is not a cause of circulatory shock?
Which of the following is a condition that is not a cause of circulatory shock?
Why can long periods of standing cause dizziness and possible fainting?
Why can long periods of standing cause dizziness and possible fainting?
The Arteriosclerosis causes which effect?
The Arteriosclerosis causes which effect?
Flashcards
Arteries
Arteries
Vessels that carry blood away from the heart.
Veins
Veins
Vessels that carry blood back to the heart.
Capillaries
Capillaries
Connect smallest arteries to smallest veins, forming a circuit.
Tunica Interna
Tunica Interna
Signup and view all the flashcards
Tunica Media
Tunica Media
Signup and view all the flashcards
Tunica Externa
Tunica Externa
Signup and view all the flashcards
Vasa Vasorum
Vasa Vasorum
Signup and view all the flashcards
Conducting Arteries
Conducting Arteries
Signup and view all the flashcards
Distributing Arteries
Distributing Arteries
Signup and view all the flashcards
Arterioles
Arterioles
Signup and view all the flashcards
Metarterioles
Metarterioles
Signup and view all the flashcards
Aneurysm
Aneurysm
Signup and view all the flashcards
Arterial Sense Organs
Arterial Sense Organs
Signup and view all the flashcards
Carotid Sinuses
Carotid Sinuses
Signup and view all the flashcards
Chemoreceptors
Chemoreceptors
Signup and view all the flashcards
Capillaries
Capillaries
Signup and view all the flashcards
Microvasculature
Microvasculature
Signup and view all the flashcards
Continuous Capillaries
Continuous Capillaries
Signup and view all the flashcards
Basal Lamina
Basal Lamina
Signup and view all the flashcards
Pericytes
Pericytes
Signup and view all the flashcards
Fenestrated Capillaries
Fenestrated Capillaries
Signup and view all the flashcards
Sinusoids
Sinusoids
Signup and view all the flashcards
Capillary Beds
Capillary Beds
Signup and view all the flashcards
Precapillary Sphincters
Precapillary Sphincters
Signup and view all the flashcards
Veins
Veins
Signup and view all the flashcards
Postcapillary Venules
Postcapillary Venules
Signup and view all the flashcards
Muscular Venules
Muscular Venules
Signup and view all the flashcards
Large Veins
Large Veins
Signup and view all the flashcards
Simplest Circulatory Route
Simplest Circulatory Route
Signup and view all the flashcards
Portal System
Portal System
Signup and view all the flashcards
Anastomosis
Anastomosis
Signup and view all the flashcards
Arteriovenous Anastomosis (Shunt)
Arteriovenous Anastomosis (Shunt)
Signup and view all the flashcards
Venous Anastomosis
Venous Anastomosis
Signup and view all the flashcards
Arterial Anastomosis
Arterial Anastomosis
Signup and view all the flashcards
Hemodynamics
Hemodynamics
Signup and view all the flashcards
Blood Pressure (BP)
Blood Pressure (BP)
Signup and view all the flashcards
Systolic Pressure
Systolic Pressure
Signup and view all the flashcards
Diastolic Pressure
Diastolic Pressure
Signup and view all the flashcards
Pulse Pressure
Pulse Pressure
Signup and view all the flashcards
Mean Arterial Pressure (MAP)
Mean Arterial Pressure (MAP)
Signup and view all the flashcards
Arteriosclerosis
Arteriosclerosis
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
Hypertension
Hypertension
Signup and view all the flashcards
Hypotension
Hypotension
Signup and view all the flashcards
Peripheral Resistance
Peripheral Resistance
Signup and view all the flashcards
Vasomotion
Vasomotion
Signup and view all the flashcards
Autoregulation
Autoregulation
Signup and view all the flashcards
Baroreflex
Baroreflex
Signup and view all the flashcards
Chemoreflex
Chemoreflex
Signup and view all the flashcards
Angiotensin II
Angiotensin II
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Natriuretic Peptides
Natriuretic Peptides
Signup and view all the flashcards
Antidiuretic Hormone (ADH)
Antidiuretic Hormone (ADH)
Signup and view all the flashcards
Epinephrine and Norepinephrine
Epinephrine and Norepinephrine
Signup and view all the flashcards
Filtration and Reabsorption
Filtration and Reabsorption
Signup and view all the flashcards
Hydrostatic Pressure
Hydrostatic Pressure
Signup and view all the flashcards
Colloid Osmotic Pressure (COP)
Colloid Osmotic Pressure (COP)
Signup and view all the flashcards
Net Filtration Pressure (NFP)
Net Filtration Pressure (NFP)
Signup and view all the flashcards
Net Reabsorption Pressure
Net Reabsorption Pressure
Signup and view all the flashcards
Edema
Edema
Signup and view all the flashcards
Cardiogenic Shock
Cardiogenic Shock
Signup and view all the flashcards
Low Venous Return (LVR) Shock
Low Venous Return (LVR) Shock
Signup and view all the flashcards
Hypovolemic Shock
Hypovolemic Shock
Signup and view all the flashcards
Obstructed Venous Return Shock
Obstructed Venous Return Shock
Signup and view all the flashcards
Neurogenic Shock
Neurogenic Shock
Signup and view all the flashcards
Septic Shock
Septic Shock
Signup and view all the flashcards
Anaphylactic Shock
Anaphylactic Shock
Signup and view all the flashcards
Compensated Shock
Compensated Shock
Signup and view all the flashcards
Decompensated Shock
Decompensated Shock
Signup and view all the flashcards
Study Notes
The Circulatory System: Blood Vessels and Circulation
- The circulatory system anatomy and physiology are based on the unity of form and function.
General Anatomy of Blood Vessels
- Key learning outcomes include describing blood vessel structure, types of arteries/capillaries/veins, tracing blood flow from and back to the heart, and identifying route variations.
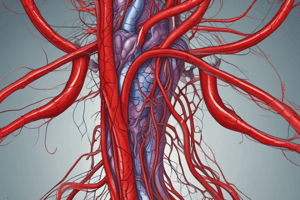
- Arteries carry blood away from the heart.
- Veins return blood to the heart.
- Capillaries connect the smallest arteries to the smallest veins, forming a circuit.
The Vessel Wall
- Arteries and veins possess walls with three layers called tunics.
- The tunica interna lines the blood vessel and has contact to blood.
- The tunica interna consists of endothelium which is simple squamous epithelium.
- It is a selectively permeable barrier.
- Chemicals for dilation or constriction are secreted.
- It normally repels blood cells and platelets to prevent clotting.
- When tissue is inflamed, it produces cell-adhesion molecules.
- Cell adhesion causes leukocytes to congregate where defensive actions are needed.
- The tunica media is the middle layer.
- It consists of smooth muscle, collagen, and elastic tissue.
- It strengthens vessels and prevents blood pressure from rupturing them.
- Muscle contraction controls blood vessel diameter.
- The tunica externa is the outermost layer.
- It has loose connective tissue which often merges with the tissue of nearby blood vessels, nerves, or organs.
- It anchors the vessel and provides passage for small nerves and lymphatic vessels.
- The vasa vasorum are small vessels supply blood to outer half of wall in the larger vessels.
Arteries
- Arteries divide into three classes based on size: conducting, distributing, and resistance arteries.
- Conducting arteries are the biggest.
- Examples include the aorta, common carotid, subclavian, pulmonary trunk, and common iliac arteries.
- They have an internal elastic lamina at the border between the tunica interna and media.
- They have an external elastic lamina at the border between the media and externa.
- They expand during systole and recoil during diastole.
- Expansion reduces pressure on downstream vessels.
- Recoil maintains pressure during relaxation to keep blood flowing.
- Distributing arteries distribute blood to specific organs.
- Examples are brachial, femoral, renal, and splenic arteries.
- Smooth muscle layers make up three-fourths of the thickness of its wall.
- Internal and external elastic laminae are thick.
- Resistance Arteries are small arteries.
- They have a thicker tunica media in proportion to their lumen, along with very little tunica externa.
- Arterioles are these arteries, and they are the smallest.
- They have a 200 mm diameter, with only one to three layers of smooth muscle.
- They control amount of blood to various organs.
- Metarterioles (thoroughfare channels) are short vessels that link arterioles directly to venules in some places (e.g., mesenteries).
- They provide shortcuts allowing blood to bypass capillary beds.
Aneurysm
- An aneurysm is a weak point in an artery or the heart wall.
- It forms a thin-walled, bulging sac that pulsates with each heartbeat and may rupture.
- In a dissecting aneurysm, blood accumulates between tunics of the artery, separating them, typically due to degeneration of the tunica media.
- Common locations include the abdominal aorta, renal arteries, and arterial circle at the base of the brain.
- Aneurysms can cause pain by putting pressure on surrounding structures, and can rupture, causing hemorrhage.
- They result from congenital blood vessel weakness, trauma, bacterial infections, or atherosclerosis and hypertension.
Arterial Sense Organs
- Sensory structures that monitor blood pressure and chemistry reside in the walls of major vessels.
- Information is transmitted to the brainstem to control heart rate, blood vessel diameter, and breathing.
- Carotid sinuses:
- Baroreceptors in the walls of internal carotid artery.
- They monitor blood pressure.
- Transmit signals through the glossopharyngeal nerve.
- Allow for baroreflex.
- Carotid bodies:
- Oval bodies near the common carotids where they divide.
- They are chemoreceptors, which monitor blood chemistry.
- They transmit signals through the glossopharyngeal nerve to the brainstem's respiratory centers.
- Adjust respiratory rate is adjusted to stabilize pH, CO2, and O2.
- Aortic bodies:
- One to three chemoreceptors in the walls of the aortic arch.
- They share same structure and function as carotid bodies, but innervation is by the vagus nerve.
Capillaries
- Capillaries are exchange vessels where gasses, nutrients, wastes, and hormones pass between the blood and tissue fluid.
- Capillaries are part of the microvasculature, which also includes arterioles and venules.
- Nearly every cell in the body is close to a capillary, except in tendons, ligaments, epithelia, cornea, and lens of the eye.
- Capillaries are composed of endothelium and basal lamina.
- There are three capillary types. They are distinguished by permeability: continuous, fenestrated, and sinusoidal.
- Continuous Capillaries are
- Found in most tissues.
- Endothelial cells held together by tight junctions; form a continuous tube with intercellular clefts separates the cells.
- Small solutes can pass through intercellular clefts, but not things like plasma protein and other large molecules can not.
- Have a basal lamina, which is a thin protein-carbohydrate layer surround endothelium.
- Have pericytes, which wrap around the capillaries.
- Pericytes contains the same contractile protein as muscle.
- Pericytes contract and regulate blood flow and can differentiate for growth and repair.
- Fenestrated Capillaries:
- Found in organs that require rapid absorption or filtration (e.g., kidneys, small intestine).
- Endothelial cells contain filtration pores (fenestrations) with a 20 to 100 nm diameter.
- These are spanned by very thin glycoprotein membrane, which is much thinner than cell’s plasma membrane.
- Allow passage of only small molecules.
- Proteins and larger particles generally stay in bloodstream.
- Sinusoids are
- Found in the liver, bone marrow, and spleen
- Irregular blood-filled spaces
- Endothelial cells are separated by wide gaps have large fenestrations with no basal lamina
- They allow proteins (albumin), clotting factors, and new blood cells to enter the circulation.
- Capillary beds are networks of 10-100 capillaries.
- Usually supplied by a single arteriole or metarteriole.
- Drain into a venule or the distal end of a metarteriole.
- 75% of body's capillaries are shut down at any given time.
- Control involves constriction of upstream arterioles.
- precapillary sphincters control flow.
- With relaxed sphincters, capillaries will have good blood flow.
- When sphincters contract, they constrict the entry to the capillary, and blood typically bypasses the capillary.
Veins
- Veins are the capacitance vessels of the cardiovascular system.
- They are thin-walled and flaccid.
- They collapse when empty and expand easily.
- Veins contain more blood than arteries. And their blood is easier to contain too.
- At rest, about 64% of blood is in veins while 13% if in the arteries.
- Blood flow is steady here, not pulsed as in arteries.
- They have a relatively low blood pressure.
- It Averages 10 mm Hg with little fluctuation.
- There are various types of veins, listed from smallest to largest: post capillary venules, muscular venules, medium veins, large veins, and venous sinuses.
- Postcapillary venules:
- Smallest veins with 10-20 um diameter.
- They consists of tunica interna with only a few fibroblasts around it and it has no muscle.
- More porous than capillaries, so they also exchange surrounding fluid.
- Leukocytes leave bloodstream through venule walls.
- Muscular venules
- Receive blood from postcapillary venules.
- Up to 1 mm in diameter.
- Consist of one or two layers of smooth muscle in the tunica media and thin tunica externa.
- Medium veins
- Up to 10 mm in diameter.
- Thin tunica media, thick tunica externa, and tunica interna form venous valves.
- Varicose veins may result from failure of these valves.
- Rely on skeletal muscle pump to propel venous blood back to heart
- Large veins
- Diameter >10 mm.
- Smooth muscle in all three tunics.
- Relatively thin tunica media with a moderate amount of smooth muscle.
- Tunica externa is the thickest layer with longitudinal bundles of smooth muscle.
- Examples: the venae cavae, pulmonary veins, internal jugular veins, and renal veins.
- Venous sinuses
- Occur in select locations.
- Modified veins with specially thin walls, large lumens, and no smooth muscle.
- They are not capable of vasoconstriction.
- Examples: dural sinuses form in the brain and coronary sinus found in heart.
Varicose Veins
- Blood pools in the lower legs of people who are standing for long periods, stretching the veins.
- Cusps of valves pull apart in enlarged superficial veins, which further weakens vessels.
- Blood backflows, further distending the vessels their walls grow weak and develop into varicose veins with dilation.
- Hereditary weakness, obesity, and pregnancy promote problems.
- Hemorrhoids are varicose veins of the anal canal.
Circulation Routes
- Blood travels a common route:
- Starting at the heart, it flows into the arteries, then arterioles, to the capillaries, and to the venules and then to the veins.
- In this route, blood passes through only one network of capillaries from the time it leaves the heart until it returns.
- There may be alternate pathways that involve two capillary beds or no capillary beds
- The portal system uses
- Portal system is a circulatory network where blood passes through two consecutive capillary networks before returning to the heart.
- Examples are
- In kidneys
- Between hypothalamus and anterior pituitary
- Between intestines and liver
- Anastomosis is convergence between two vessels.
- Arteriovenous anastomosis is when artery flows directly into vein, bypassing capillaries
- Venous anastomosis are common when one vein empties into another.
- Arterial anastomosis occur when two arteries merge with to provide collateral routes of blood supply.
Blood Pressure, Resistance, and Flow
- Key learning outcomes involve explaining the relationship between blood pressure, resistance, and flow; describing how to measure and express blood pressure; calculating pulse pressure and mean arterial pressure; detailing factors that determine resistance to blood flow; explaining how vessel diameter affects blood pressure and flow; and knowing local, neural, and hormonal influences on blood flow.
- Understanding the blood supply to a tissue it is expressed in terms of flow and perfusion.
- Flow is the amount of blood flowing through an organ, tissue, or blood vessel in a given time, measured in mL/min.
- Perfusion is the flow per given volume or mass of tissue in a given time, measured in mL/100g/min.
- Total flow at rest is constant and is to the cardiac output is about 5.25 L/min.
- Hemodynamics are physical principles of blood flow based on pressure and resistance.
- The greater the pressure difference between two points, the greater the flow. The greater the resistance, the less the flow.
Blood Pressure
-
Blood pressure (BP) is the force blood exerts against a vessel wall
-
Blood pressure is measured at the brachial artery using a sphygmomanometer.
- A close approximation of pressure at exit of left ventricle.
-
Two pressures are recorded during blood pressure measurement:
-
Systolic pressure is the peak arterial BP taken during ventricular contraction (ventricular systole).
-
Diastolic pressure is the minimum arterial BP taken during ventricular relaxation (diastole) between heart beats
-
A normal BP value for young adult is 120/75 mm Hg.
-
Stress of blood vessels is measured by pulse pressure.
- Pulse pressure is the difference between systolic and diastolic pressure.
- This is an Important measure of driving force on circulation and of stress exerted on small arteries by pressure surges generated by the heart.
- Pulse pressure is the difference between systolic and diastolic pressure.
-
Also measured is the mean arterial pressure:
- This is Diastolic pressure + (one-third of pulse pressure).
- Serves as average blood pressure that has the most influences risk level that affects one's kidney.
-
Since pressure varies across the cardiac cycle, blood flow in arteries is pulsatile.
- Speed surges from 40 cm/s to 120 cm/s.
- Blood spurts intermittently from an open artery.
-
In capillaries and veins, blood flows at a steady speed.
- Bleeding from veins tends to be slow and steady.
-
BP tends to rise with age.
- Arteriosclerosis is the stiffening of arteries due to deterioration of elastic tissues of artery walls.
- Atherosclerosis is the build up of lipid deposits that become plaques.
-
Systemic blood pressure decreases farther from heart.
-
Hypertension is
- Chronic resting blood pressure higher than 130/80
- Can weaken arteries, cause aneurysms, promote atherosclerosis.
-
Hypotension is
- Chronic low resting BP
- Caused by blood loss, dehydration, anemia.
- Includes no specific numerical criterion for hypotension.
-
BP is determined by three variables:
- Cardiac output
- Blood volume
- Resistance to flow
-
Blood volume is regulated mainly by kidneys, and this gives the the largest singular organ that affects blood pressure unless considering the heart.
Peripheral Resistance
- Peripheral resistance opposes the flow of blood in the vessels away from the heart.
- Resistance depends on three variables in blood:
- Blood viscosity from plasma protein and red blood cells.
- Low viscosity in red blood cells or plasma protein speeds the flow.
- dehydration declines of fluid in the body will hinder it.
- Pressure declines with distance of the liquid when it travels through a tube.
- Greatest control over blood flow is vessels radius.
- Greatest control over blood flow
- Blood viscosity from plasma protein and red blood cells.
- Blood exhibits laminar flow, so dilating helps vessels.
- Vasomotion controls vasoconstriction and vasodilation.
- Also, more blood volume will decrease the resistance, for example, larger radii and more cross sections from capillaries which all lower the resistance. Volume is further compliant by being further away also.
- Arterioles are most significant point of control due to its positioning and they outnumber other types of artery. They area also muscular to maintain the flow.
Regulation of Blood Pressure and Flow
- Vasomotion is a quick, powerful way to alter blood pressure and flow.
- Three ways of controlling vasomotor activity:
- Local control
- Neural control
- Hormonal control
- Local auto regulation:
- Autoregulation enables tissues to regulate their blood supply.
- If tissue is inadequately perfused(deoxygenated), then waste accumulates, stimulating perfusion.
- Autoregulation enables tissues to regulate their blood supply.
- Neural control;
- Remote control from vessel and neural system in center to automatic.
- Vasomotor's center provides the sympathetic controls such as baro and chemo.
- Hormonal control;
- Uses kidney processes such as aldosterone or angiotensin for increased absorption for higher blood volume.
Two Purposes of Vasomotion
- Serves to do the the overall.
- Selectively reroute region which required concentrated perfusion.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.