Podcast
Questions and Answers
Which layer of a blood vessel wall is primarily responsible for vasoconstriction and vasodilation?
Which layer of a blood vessel wall is primarily responsible for vasoconstriction and vasodilation?
- Tunica adventitia
- Tunica media (correct)
- Tunica intima
- Tunica externa
What is the primary function of the endothelium in the tunica interna of a blood vessel?
What is the primary function of the endothelium in the tunica interna of a blood vessel?
- To provide structural support to the vessel wall
- To act as a selectively permeable barrier and prevent platelet adhesion (correct)
- To facilitate gas exchange between blood and surrounding tissues
- To secrete chemicals that cause inflammation
Which type of artery is best suited to withstand the high pressure surges produced by the heart?
Which type of artery is best suited to withstand the high pressure surges produced by the heart?
- Elastic arteries (correct)
- Capillaries
- Arterioles
- Muscular arteries
Which type of blood vessel is primarily responsible for transporting blood away from the heart?
Which type of blood vessel is primarily responsible for transporting blood away from the heart?
What is the primary function of capillaries within the circulatory system?
What is the primary function of capillaries within the circulatory system?
What structural feature is unique to fenestrated capillaries that distinguishes them from continuous capillaries?
What structural feature is unique to fenestrated capillaries that distinguishes them from continuous capillaries?
Which of the following best describes the role of veins in the circulatory system?
Which of the following best describes the role of veins in the circulatory system?
Which of the following best describes the function of precapillary sphincters?
Which of the following best describes the function of precapillary sphincters?
Which of the following characteristics is NOT associated with veins?
Which of the following characteristics is NOT associated with veins?
If a patient's systolic blood pressure is 130 mmHg and diastolic blood pressure is 85 mmHg, what is their mean arterial pressure (MAP), rounded to the nearest whole number, given $MAP = \frac{1}{3}(Systolic + 2 \times Diastolic)$?
If a patient's systolic blood pressure is 130 mmHg and diastolic blood pressure is 85 mmHg, what is their mean arterial pressure (MAP), rounded to the nearest whole number, given $MAP = \frac{1}{3}(Systolic + 2 \times Diastolic)$?
Which of the following mechanisms is NOT directly involved in regulating blood pressure?
Which of the following mechanisms is NOT directly involved in regulating blood pressure?
What is the significance of the wide gaps and pores present in the sinusoids of organs like the liver and bone marrow?
What is the significance of the wide gaps and pores present in the sinusoids of organs like the liver and bone marrow?
A researcher is studying a newly discovered compound that selectively blocks the action of nitric oxide (NO) in the vasculature. What would be the expected effect of this compound on blood pressure and local blood flow?
A researcher is studying a newly discovered compound that selectively blocks the action of nitric oxide (NO) in the vasculature. What would be the expected effect of this compound on blood pressure and local blood flow?
A newly developed drug causes a significant increase in the number of intercellular clefts in the continuous capillaries of the brain. What is the most likely consequence of this?
A newly developed drug causes a significant increase in the number of intercellular clefts in the continuous capillaries of the brain. What is the most likely consequence of this?
In a hypothetical scenario, a toxin selectively destroys the venous valves in the lower extremities. What is the most likely immediate consequence of this condition?
In a hypothetical scenario, a toxin selectively destroys the venous valves in the lower extremities. What is the most likely immediate consequence of this condition?
A patient is diagnosed with a condition that impairs the function of pericytes in their capillaries. Which of the following is the MOST likely long-term effect of this condition?
A patient is diagnosed with a condition that impairs the function of pericytes in their capillaries. Which of the following is the MOST likely long-term effect of this condition?
Which characteristic distinguishes veins from arteries regarding blood flow?
Which characteristic distinguishes veins from arteries regarding blood flow?
What structural adaptation is present in many medium veins to counteract the lower pressure of blood?
What structural adaptation is present in many medium veins to counteract the lower pressure of blood?
What anatomical feature is characteristic of the smallest venules and facilitates the movement of white blood cells into tissues?
What anatomical feature is characteristic of the smallest venules and facilitates the movement of white blood cells into tissues?
Which of the following statements accurately describes the relative composition of tunica media and externa of medium veins?
Which of the following statements accurately describes the relative composition of tunica media and externa of medium veins?
What is the distinguishing feature of large veins compared to medium and small veins (venules)?
What is the distinguishing feature of large veins compared to medium and small veins (venules)?
What is a key characteristic of blood flow in veins?
What is a key characteristic of blood flow in veins?
What is the primary function of venous valves?
What is the primary function of venous valves?
In a portal system, how many capillary beds does blood flow through before returning to the heart?
In a portal system, how many capillary beds does blood flow through before returning to the heart?
Why are portal systems strategically located in the body?
Why are portal systems strategically located in the body?
Which of the following is NOT a primary distinction between veins and arteries?
Which of the following is NOT a primary distinction between veins and arteries?
Which of the following factors does NOT directly influence peripheral resistance?
Which of the following factors does NOT directly influence peripheral resistance?
Vasodilation, the widening of blood vessels, is achieved primarily through the:
Vasodilation, the widening of blood vessels, is achieved primarily through the:
Which of the following is an example of local control of blood pressure and flow?
Which of the following is an example of local control of blood pressure and flow?
Angiotensin-converting enzyme (ACE) inhibitors are often prescribed to treat hypertension because they:
Angiotensin-converting enzyme (ACE) inhibitors are often prescribed to treat hypertension because they:
A hypothetical scenario presents a patient with chronic kidney disease, experiencing both severely impaired erythropoietin production and significant proteinuria (protein loss in urine). Considering the interplay of viscosity, osmosis and hormonal regulation, which of the following accurately predicts the combined effect on capillary fluid dynamics at the venous end?
A hypothetical scenario presents a patient with chronic kidney disease, experiencing both severely impaired erythropoietin production and significant proteinuria (protein loss in urine). Considering the interplay of viscosity, osmosis and hormonal regulation, which of the following accurately predicts the combined effect on capillary fluid dynamics at the venous end?
What is the primary function of anastomoses in the circulatory system?
What is the primary function of anastomoses in the circulatory system?
Which of the following best describes 'perfusion' in the context of blood flow?
Which of the following best describes 'perfusion' in the context of blood flow?
Why can a smaller organ, such as the pituitary gland, have a higher perfusion rate but a lower overall blood flow compared to a larger organ like the thigh muscle?
Why can a smaller organ, such as the pituitary gland, have a higher perfusion rate but a lower overall blood flow compared to a larger organ like the thigh muscle?
According to the principles governing fluid flow, what primarily drives blood flow through the circulatory system?
According to the principles governing fluid flow, what primarily drives blood flow through the circulatory system?
Arterial blood pressure is expressed as a ratio. What do the two values in this ratio, such as 120/80 mmHg, represent?
Arterial blood pressure is expressed as a ratio. What do the two values in this ratio, such as 120/80 mmHg, represent?
A patient's blood pressure is consistently measured at 130/80 mmHg at rest. According to the information, this would be classified as:
A patient's blood pressure is consistently measured at 130/80 mmHg at rest. According to the information, this would be classified as:
Which of the following conditions could potentially result in chronic hypotension?
Which of the following conditions could potentially result in chronic hypotension?
Which of the following is NOT one of the 3 main principles that determine blood pressure?
Which of the following is NOT one of the 3 main principles that determine blood pressure?
Calculate the mean arterial pressure (MAP) given a blood pressure of 140/90 mmHg and a heart rate of 70 bpm if diastolic pressure remains normal but systolic pressure increases by 10%.
Calculate the mean arterial pressure (MAP) given a blood pressure of 140/90 mmHg and a heart rate of 70 bpm if diastolic pressure remains normal but systolic pressure increases by 10%.
A researcher is investigating the effects of a novel vasodilator drug on blood flow. If the drug reduces resistance to blood flow by 20% without significantly affecting cardiac output, what would be the expected change in mean arterial pressure (MAP), assuming initial MAP was 100 mmHg?
A researcher is investigating the effects of a novel vasodilator drug on blood flow. If the drug reduces resistance to blood flow by 20% without significantly affecting cardiac output, what would be the expected change in mean arterial pressure (MAP), assuming initial MAP was 100 mmHg?
Flashcards
Arteries
Arteries
Blood vessels carrying blood away from the heart.
Capillaries
Capillaries
Microscopic blood vessels facilitating exchange between blood and tissues.
Veins
Veins
Blood vessels carrying blood towards the heart.
Blood Pressure
Blood Pressure
Signup and view all the flashcards
Regulation of Blood Pressure
Regulation of Blood Pressure
Signup and view all the flashcards
Capillary Exchange
Capillary Exchange
Signup and view all the flashcards
Venous Return
Venous Return
Signup and view all the flashcards
Tunica Interna
Tunica Interna
Signup and view all the flashcards
Tunica Media
Tunica Media
Signup and view all the flashcards
Tunica Externa
Tunica Externa
Signup and view all the flashcards
Conducting Arteries
Conducting Arteries
Signup and view all the flashcards
Distributing Arteries
Distributing Arteries
Signup and view all the flashcards
Resistance Arteries
Resistance Arteries
Signup and view all the flashcards
Venules
Venules
Signup and view all the flashcards
Medium Veins
Medium Veins
Signup and view all the flashcards
Venous Valves
Venous Valves
Signup and view all the flashcards
Large Veins
Large Veins
Signup and view all the flashcards
Most Common Circulatory Route
Most Common Circulatory Route
Signup and view all the flashcards
Portal System
Portal System
Signup and view all the flashcards
Purpose of Portal Systems
Purpose of Portal Systems
Signup and view all the flashcards
Medium Vein Walls
Medium Vein Walls
Signup and view all the flashcards
Porous Venules
Porous Venules
Signup and view all the flashcards
Peripheral Resistance
Peripheral Resistance
Signup and view all the flashcards
Blood Viscosity
Blood Viscosity
Signup and view all the flashcards
Vasoconstriction
Vasoconstriction
Signup and view all the flashcards
Vasodilation
Vasodilation
Signup and view all the flashcards
Baroreceptors
Baroreceptors
Signup and view all the flashcards
Anastomoses
Anastomoses
Signup and view all the flashcards
Blood Flow
Blood Flow
Signup and view all the flashcards
Perfusion
Perfusion
Signup and view all the flashcards
Systolic Pressure
Systolic Pressure
Signup and view all the flashcards
Diastolic Pressure
Diastolic Pressure
Signup and view all the flashcards
Sphygmomanometer
Sphygmomanometer
Signup and view all the flashcards
Hypertension
Hypertension
Signup and view all the flashcards
Hypotension
Hypotension
Signup and view all the flashcards
Blood Pressure Determinants
Blood Pressure Determinants
Signup and view all the flashcards
Study Notes
- Vasculature is the arrangement of blood vessels in the body.
Outline of Vasculature
- General anatomy of blood vessels
- Arteries
- Capillaries
- Veins
- Physiology of circulation
- Blood pressure
- Regulation of blood pressure
- Capillary exchange
- Venous return
- Circulatory shock
General Anatomy of Blood Vessels
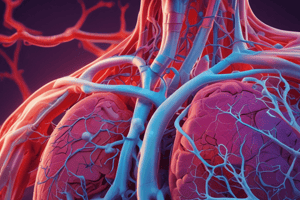
- Three categories of blood vessels are arteries, veins, and capillaries.
- The categories differ by direction of blood flow, pressure they withstand, and histological structure of their walls.
- Arteries and veins have three tissue layers: tunica interna, tunica media, and tunica externa.
- Capillaries consist of only the tunica interna, the innermost layer.
- Tunica interna is the inner lining of the vessel and creates the borders of the lumen, being in direct contact with blood.
- It consists of simple squamous epithelium called the endothelium, which acts as a selectively permeable barrier.
- Tunica interna also secretes chemicals to prevent adhesion and platelet aggregation.
- Tunica interna also secretes chemicals that dilate or constrict blood vessels, regulating blood flow.
- Tunica media is the middle layer, usually the thickest which consists of smooth muscle, collagen, and elastic tissue.
- Smooth muscle carries out vasoconstriction and vasodilation.
- Tunica externa is the outermost layer which consists of loose connective tissue, anchoring the vessel to surrounding tissues.
- The tunica externa provides passage for small nerves, lymphatic vessels, and other smaller blood vessels.
- Arteries carry blood away from the heart.
- Veins carry blood back to the heart.
- Capillaries are microscopic vessels connecting the smallest arteries to the smallest veins.
Arteries: Qualities
- Arteries have a resilient structure, endure a surge in pressure with each heartbeat.
- The vessel retains a round shape when empty because arteries are more muscular than veins.
- Three types categorized by size exist: conducting (large), distributing (medium), and resistance (small).
- Large arteries branch into smaller arteries.
Arteries: Conducting (elastic or large)
- Includes the largest arteries like the aorta and pulmonary trunk.
- They can be up to 1 inch in diameter.
- The tunica media is dominated by layers of perforated elastic sheets of tissue.
- Smooth muscle and collagen are also present but less visible.
- Arteries expand during systole and recoil during diastole due to the abundance of elastic tissues.
- Elasticity protects smaller vessels downstream by reducing pressure surge during ejection from the heart as well as preventing blood pressure from dropping, which propels blood.
Arteries: Distributing (muscular or medium)
- Distributing arteries are smaller than elastic ones, distributing blood to specific organs.
- Think of conducting arteries as interstate highways and distributing arteries as exit ramps/state highways.
- The tunica media is dominated by smooth muscle with less elastic tissue.
- Examples include the femoral, brachial, or renal arteries.
Arteries: Resistance (small)
- These are too variable in number and location to have individual names.
- The tunica media is primarily smooth muscle with very little elastic tissue.
- Arterioles are the smallest of the resistance arteries.
- They are the initial point of control over how much blood an organ/tissue receives.
Capillaries
- Materials (wastes, hormones, nutrients) must pass through vessel walls to reach tissues.
- This process occurs primarily in capillaries, often called exchange vessels.
- There are an estimated 1 billion capillaries in the body, placing each cell within 4-6 cell widths of the nearest capillary.
- Capillaries are composed of an endothelium and a basement membrane, with walls as thin at 0.2-0.4 μm.
- They range in diameter from 5-9 μm, but cells can stretch to 7.5 μm
- Three types of capillaries are continuous, fenestrated, and sinusoids.
Capillaries: Continuous
- These are the most common type.
- The tubes of endothelial cells rolled up like a burrito and held together by tight junctions, with gaps between cells called intercellular clefts.
- Intercellular clefts allow small solutes to pass through.
- Pericytes can differentiate into new muscle and endothelial cells to help repair the capillaries, or other vessels.
Capillaries: Fenestrated
- Fenestrated capillaries have large filtration pores.
- Intercellular clefts are about 4 nm wide, with the filtration pores much larger, at 20-200 nm wide.
- They allow much larger molecules to pass through and are located where rapid filtration is needed like the kidneys.
Capillaries: Sinusoids
- These conform to the shape of the surrounding tissue.
- Their passages are 30-40 μm wide and the endothelial cells are separated by wide gaps, with large pores to pass large cells.
- Proteins and blood cells can pass through the pores of sinusoids.
- Sinusoids location include the liver, allowing albumin and clotting factors to enter, as well as bone narrow, allowing newly formed cells to enter circulation.
Capillary Beds
- The capillaries are organized in capillary beds, webs of 10-100 vessels per arteriole.
- Each capillary has a precapillary sphincter at the beginning which can dilate to let blood into a capillary, or constrict to prevent blood flow.
- Capillary beds blood flow is regulated to match the tissues needs.
- There is not enough blood to fill the vascular system at once, with ~75% shut down at any given time.
Veins
- Veins are regarded as capacitance vessels because they are relatively thin-walled, flaccid.
- Easy to accommodate increased blood volume, the have a greater capacity for blood than arteries.
- At rest, ~64% of blood is in systemic veins, and only 15% is in the arteries.
- Veins are distant from the ventricles of the heart, so are subjected to lower pressure, with steady blood flow.
- Veins do not require a muscular walls to withstand pressure surges.
- Small veins merge to form larger and larger veins.
- Three are types of vein, categorized on the basis of their size, including venules, medium sized veins and large veins.
Veins: Venules
- Venules receive blood from capillaries.
- Venules range up to 1mm in diameter.
- The smallest venules have no tunica media and are porous.
- White blood cells leave bloodstream to migrate into tissues via venules.
Veins: Medium Veins
- Medium veins range up to 10mm in diameter.
- They have a thicker tunica media and externa compared to venules.
- Many medium veins have individual names, such as the brachial vein.
- Many have venous valves, because under less pressure, blood movement requires skeletal muscle.
- Valves prevent backflow.
Veins: Large Veins
- Diameter is greater than 10mm.
- Includes veins that empty into the heart with two vena cava and four pulmonary veins.
Variations in Circulatory Routes
- Most common route is where oxygenated heart leaves via arteries through the capillary bed then deoxygenated blood returns via the veins.
- The variation to this blood pattern is portal system, where blood flows through two capillary system before returning to the heart.
- Portal systems are found where a substance is to be picked up by one capillary bed, then immediately given off by another.
- Anastomoses are another variation which involve routes that bypass the capillaries and goes directly from an artery to a vein or from one vein to another or from one artery to another.
Physiology of Circulation
- Blood flow refers to the amount of blood passing any given point.
- Perfusion is the flow relative to a given mass of tissue (ml/min per 100 grams of tissue).
- A small organ can therefore have greater relative perfusion but lower overall flow than a larger organ.
- Blood flow is governed by the fundamental principles that govern fluid flow: pressure and resistance.
Blood Pressure
- Blood pressure is the force exerted by blood on a vessel wall.
- Blood always flows down a pressure gradient (high to low).
- The greater the pressure gradient, the greater the flow.
- Arterial blood pressure is expressed as a ratio of systolic pressure to diastolic pressure.
- Systolic pressure is the pressure generated by left ventricle contraction, and diastolic pressure is the minimum blood pressure falls when ventricles relax.
- Blood pressure is measured with a sphygmomanometer, with readings expressed in millimeters of mercury (mmHg).
- A typical healthy adult is 120/80.
- Persistent high BP is associated with cardiovascular disease.
- A persistent resting blood pressure of 130/80 is considered hypertension.
- It does not include temporary elevations due to emotions or exercise.
- Chronic low blood pressure is called hypotension.
- Hypotension could result from blood loss, dehydration, or inability to regulate blood pressure fluctuation in old age.
- There is no defined numerical criteria for hypotension.
Regulation of Blood Pressure
- Determined by 3 principles:
- Cardiac output (stroke volume x heart rate)
- Blood volume
- Regulated mainly by kidneys
- Resistance to flow
Peripheral Resistance
- Peripheral resistance is the measure of difficulty of blood flowing through a vessel, caused by friction with vessel walls.
- It is the opposition to flow in vessels away from the heart.
- An higher resistance decreases flow, unless the heart pumps harder to compensate
- Resistance is determined by:
- Viscosity
- Length
- Radius
Peripheral Resistance: Viscosity
- Viscosity is the "thickness" of the blood.
- Higher viscosity increases resistance, impeding flow.
- Blood viscosity is determined by concentration of erythrocytes and albumin.
Peripheral Resistance: Vessel Length
- The farther a liquid travels through a vessel, the more cumulative resistance encounters.
- Both pressure and flow accordingly decline distally.
Peripheral Resistance: Vessel Radius
- It is is most important variable in flow as vessel length and blood viscosity usually don't change rapidly.
- Regulation can be accomplished by adjusting radius of blood vessels.
- Vasoconstriction- narrowing of vessel
- Vasodilation- widening of vessel
- Achieved by contraction or relaxation of smooth muscle in the tunica media.
Regulation of Blood Pressure and Flow: Hormonal
- Perfusion adapts to ever-changing demand.
- Mechanisms controlling perfusion are local, neural, and hormonal.
Regulation of Blood Pressure and Flow: Local Control
- A tissue with a high metabolic rate has an increased need of oxygen and nutrients and produces more by-products, such as CO₂, lactic acid, etc.
- Vessels dilate and perfusion increases when this high metabolic rate exists.
- Long-term high metabolic demand causes angiogenesis, generating a denser capillary network.
- Long-term muscular conditions and cancerous tissues can cause local control.
Regulation of Blood Pressure and Flow: Neural Control
- Blood vessel diameter is also regulated by autonomic nervous system.
- Vessels have sensory nerve endings called baroreceptors, which monitor BP, sending signals to the medulla oblongata.
- When BP rises above normal, the vasomotor center of the medulla oblongata sends a signal to dilate blood vessels, decreasing resistance/BP falls.
- When BP falls below normal, the vasomotor center sends a signal to constrict blood vessels, increasing resistance raising the BP rise.
- These reactions are called baroreflexes.
- BP is constantly adjusted to respond to a variety of circumstances, such as gravity drawing pooling blood when standing up quickly.
Regulation of Blood Pressure and Flow: Hormonal Control
- Hormones can affect blood pressure by constricting or dilating blood vessels.
- Epinephrine and Norepinephrine are released from the adrenal medulla and sympathetic nerves, respectively.
- Epinephrine and Norepinephrine dilate some vessels and constrict other vessels.
- Angiotensin II is produced through collaboration of the liver, kidneys, and lungs.
- It is a potent which raises BP, for which angiotensin-converting enzyme (ACE) is necessary.
- Hypertension is often treated with ACE inhibitors, lowering Angiotensin levels.
- Natriuretic peptides are other hormonal mechanisms affecting blood pressure, by regulating urinary loss, and in turn affects blood volume.
- They are secreted by the heart when BP is too high.
- Stimulate kidneys to secrete more sodium; water then follows by osmosis, excreted by the body, lowering overall blood and BP.
- Aldosterone promotes Na and water retention in the body, raising blood volume and BP in turn.
- Antidiuretic hormone does the same, promoting retention and water.
Capillary Fluid Exchange
- Facilitated by diffusion, filtration, and osmosis.
Capillary Fluid Exchange: Diffusion
- If a substance is more concentrated in blood compared to surrounding tissue and is capable of crossing the wall, then it can cross the capillary via the substance
- Diffuses through the plasma membrane:
- Oxygen
- Carbon dioxide
- Steroid hormones
Capillary Fluid Exchange: Filtration
- Blood pressure forces fluid through the capillary wall, carrying solutes from coffee.
Capillary Fluid Exchange: Osmosis
- Osmosis is a high concentration of Na, protein, and erythrocytes in the blood. Water moves from areas of low solute concentration to areas of high concentration.
- Capillaries tend to absorb water from surrounding tissues.
- Some solutes may be dissolved in the water and follow the blood into the capillaries known as solvent drag.
Exchange Summary
- Arterial end of the capillary primarily gives off fluid to tissues and delivers nutrients/oxygen.
- Venous end of capillary primarily absorbs fluid and picks up materials like metabolic waste and excess water.
- Blood entering the capillary from the arteriole is under higher pressure, so filtration override osmosis, so fluid leaves the capillary.
- As blood reaches venous end due to the low pressure level there, osmosis overrides pressure and absorbs more fluid than it gives off at venous end due to the low-pressure level.
Venous Return
- After the blood exchanges materials, it's time for it to return.
- Flow back to the heart is called venous return which can be aided by gravity but anything below the heart opposes it.
- Contributing factors are gravity aids and opposes.
- Blood pressure helps but much less than the arteries and still insufficient to move blood so skeletal and thoracic pumps assist in maintaining bloodflow.
- The skeletal muscle pump, involving the relaxation and flexing of muscle on limbs causes the squeezing of blood vessels through and maintenance of blood flow.
Venous Return: Skeletal Muscle Pump
- As lower and upper limbs are exercised, veins are squeezed in effect and blood flow is encouraged through relaxation.
- Medium veins on limbs have valves that enable the process and the regulation of blood, preventing return.
- Muscles contracting force blood up and the valves prevent backflow.
Venous Return: Thoracic Pump
- When you inhale, your chest expands, creating a squeezing effect for blood flow.
- Pressure in the thoracic cavity drops below the pressure in the abdominal cavity.
- This pressure difference squeezes the abdominal portion of the inferior vena cava, pushing blood up.
- This, and the skeletal pump, are partly why exercise and deep breathing are good for blood circulation.
Circulatory Shock
- Circulatory shock is when the heart fails to pump enough blood to meet the demands of organs.
- This can be a result of a major blood loss, compressing of vessels by tumors, and blood flow blocking of venous pooling.
- Venous pooling can result from allergic reactions.
- Standing can result from venous pooling via the skeletal muscle and if it occurs for too long, fainting occurs as a result.
- Most of the time the body can recover from circulatory shock, with severe cases leading to death.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.