Podcast
Questions and Answers
What effect does aldosterone have on blood volume?
What effect does aldosterone have on blood volume?
- Increases water retention (correct)
- Increases vascular inflammation
- Decreases water retention
- Reduces sodium absorption
How does angiotensin II impact vasopressin release?
How does angiotensin II impact vasopressin release?
- Stimulates vasopressin release (correct)
- Has no effect on vasopressin release
- Inhibits vasopressin release
- Directly produces vasopressin
Which receptor does vasopressin primarily act on to promote water retention in the kidneys?
Which receptor does vasopressin primarily act on to promote water retention in the kidneys?
- V1 receptor
- Alpha-1 receptor
- V2 receptor (correct)
- Beta-2 receptor
What is one of the roles of mineralocorticoid receptors (MR) in the vasculature?
What is one of the roles of mineralocorticoid receptors (MR) in the vasculature?
Which of the following describes a consequence of increased cardiac output (CO)?
Which of the following describes a consequence of increased cardiac output (CO)?
What role do juxtaglomerular cells play in the renin-angiotensin system?
What role do juxtaglomerular cells play in the renin-angiotensin system?
How does angiotensin II affect sodium resorption in the kidneys?
How does angiotensin II affect sodium resorption in the kidneys?
Which mechanism allows angiotensin II to stimulate aldosterone release?
Which mechanism allows angiotensin II to stimulate aldosterone release?
What is the primary effect of antidiuretic hormone (ADH) on the kidneys?
What is the primary effect of antidiuretic hormone (ADH) on the kidneys?
In the context of homeostasis, what is the main function of antidiuretic hormone (ADH)?
In the context of homeostasis, what is the main function of antidiuretic hormone (ADH)?
What is the primary action of aldosterone in the kidney?
What is the primary action of aldosterone in the kidney?
Which of the following statements about ADH is correct?
Which of the following statements about ADH is correct?
Which mechanism is primarily responsible for vasoconstriction mediated by vasopressin?
Which mechanism is primarily responsible for vasoconstriction mediated by vasopressin?
What is the role of natriuretic peptides in cardiovascular homeostasis?
What is the role of natriuretic peptides in cardiovascular homeostasis?
What triggers the release of renin in the RAAS system?
What triggers the release of renin in the RAAS system?
How does the RAAS system affect blood pressure?
How does the RAAS system affect blood pressure?
Which type of natriuretic peptide is released in response to increased heart wall tension?
Which type of natriuretic peptide is released in response to increased heart wall tension?
What effect does ADH have on blood pressure?
What effect does ADH have on blood pressure?
Flashcards
What is the action of Antidiuretic Hormone (ADH) in the kidney?
What is the action of Antidiuretic Hormone (ADH) in the kidney?
A hormone produced by the pituitary gland that acts on the collecting duct of the nephron to increase water reabsorption by promoting the movement of aquaporin 2 (AQP2) water channels to the membrane.
How does ADH affect blood pressure?
How does ADH affect blood pressure?
ADH increases blood pressure by increasing blood volume and thus cardiac output (preload) as well as increasing peripheral resistance through vasoconstriction.
Describe the mechanism of action of ADH in the collecting duct.
Describe the mechanism of action of ADH in the collecting duct.
ADH binds to V2 receptors in the collecting duct, activating adenylate cyclase (AC) and producing cyclic adenosine monophosphate (cAMP). cAMP activates protein kinase A (PKA), which promotes the movement of AQP2 to the membrane.
Explain how ADH causes vasoconstriction.
Explain how ADH causes vasoconstriction.
Signup and view all the flashcards
What is the function of Aldosterone?
What is the function of Aldosterone?
Signup and view all the flashcards
Describe the renin-angiotensin-aldosterone system (RAAS) and its role in blood pressure regulation.
Describe the renin-angiotensin-aldosterone system (RAAS) and its role in blood pressure regulation.
Signup and view all the flashcards
How do Natriuretic Peptides affect blood volume and blood pressure?
How do Natriuretic Peptides affect blood volume and blood pressure?
Signup and view all the flashcards
What is the role of the sympathetic nervous system (SNS) in blood pressure regulation?
What is the role of the sympathetic nervous system (SNS) in blood pressure regulation?
Signup and view all the flashcards
Aldosterone - Role in BP Regulation
Aldosterone - Role in BP Regulation
Signup and view all the flashcards
Aldosterone's Action on Kidneys
Aldosterone's Action on Kidneys
Signup and view all the flashcards
Aldosterone's Effect on Heart
Aldosterone's Effect on Heart
Signup and view all the flashcards
Aldosterone's Impact on Blood Pressure
Aldosterone's Impact on Blood Pressure
Signup and view all the flashcards
Antidiuretic Hormone (ADH) - Role in BP Regulation
Antidiuretic Hormone (ADH) - Role in BP Regulation
Signup and view all the flashcards
What does renin do?
What does renin do?
Signup and view all the flashcards
How does Angiotensin II affect aldosterone?
How does Angiotensin II affect aldosterone?
Signup and view all the flashcards
How does Angiotensin II affect sodium reabsorption?
How does Angiotensin II affect sodium reabsorption?
Signup and view all the flashcards
What is the function of Antidiuretic hormone (ADH)?
What is the function of Antidiuretic hormone (ADH)?
Signup and view all the flashcards
How does Angiotensin II affect ADH?
How does Angiotensin II affect ADH?
Signup and view all the flashcards
Study Notes
ANS Control of Blood Pressure
- The autonomic nervous system (ANS) modulates blood pressure through both the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
- The SNS increases blood pressure by increasing vasoconstriction, heart rate, and cardiac contractility.
- The PNS decreases blood pressure by decreasing heart rate.
- Baroreceptors sense changes in blood pressure and signal the ANS to maintain homeostasis.
SNS Control of Blood Vessels
- SNS stimulation of most peripheral arteries results in vasoconstriction primarily mediated by alpha receptors.
- SNS stimulation of muscle and lung arteries, mostly mediated by epinephrine and norepinephrine from the adrenal gland, also results in vasoconstriction.
- SNS stimulation of veins predominately leads to decreased venous capacitance. This is mediated by alpha receptors increasing cardiac return, stroke volume, and cardiac output, producing a slight increase in pulse pressure.
- SNS innervation is minimal in most blood vessels.
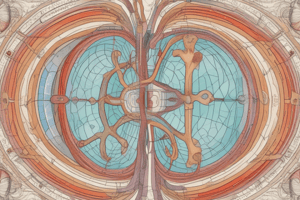
RAAS System
- The renin-angiotensin-aldosterone system (RAAS) is a crucial long-term regulator of blood pressure, aiming to regulate blood volume.
- The system consists of renin, angiotensinogen, angiotensin I, angiotensin II, and aldosterone.
- Renin, produced by the kidneys, cleaves angiotensinogen to angiotensin I.
- Angiotensin-converting enzyme (ACE), found in the lungs and kidneys, converts angiotensin I to angiotensin II, a powerful vasoconstrictor.
- Angiotensin II increases blood pressure and stimulates the release of aldosterone from the adrenal cortex.
- Aldosterone increases sodium reabsorption by the kidneys, which in turn leads to increased water retention, enhancing blood volume and furthering blood pressure regulation.
Short and Long-Term Responses to Low BP or Blood Volume
- Short-term responses include sympathetic activation and release of epinephrine and norepinephrine by the adrenal glands, increasing cardiac output and peripheral vasoconstriction.
- Long-term responses include renin and erythropoietin production by the kidneys and increased thirst, which boosts blood volume and restoration of homeostasis.
Baroreceptors and Blood Pressure
- Baroreceptors are pressure-sensitive nerve endings that detect changes in blood pressure.
- Decreases in blood pressure stimulate the baroreceptors to increase SNS activity to increase blood pressure.
- Elevations in blood pressure cause the opposite effect—increasing PNS activity to decrease blood pressure.
Aldosterone and Blood Pressure
-Aldosterone is a steroid hormone released by the adrenal cortex in response to renin-angiotensin II signaling.
- Aldosterone increases Na+ reabsorption and thereby water retention in the cortical collecting duct.
- Increased Na+ reabsorption from the cortex increases blood volume and thus increases blood pressure.
ADH/AVP and Blood Pressure
- Antidiuretic hormone (ADH), also known as vasopressin, is produced by the hypothalamus and released by the posterior pituitary gland.
- ADH acts on distal tubules and collecting ducts within the kidney to reinforce Na+ and water reabsorption. -This increases the volume of blood, therefore increasing blood pressure.
- ADH also has vasoconstricting effects by activating V1 receptors that will enhance vasoconstriction.
Natriuretic Peptides (NPs)
- NPs, such as ANP and BNP, are produced by the heart in response to increased blood volume and pressure.
- They act to decrease blood pressure and volume by inhibiting Na+ reabsorption and increasing natriuresis (excretion of sodium) in distal tubules and collecting ducts.
- Effects from NPs on blood pressure regulation are mediated through their guanylyl cyclase receptors.
- NPs counteract vasoconstriction and decrease blood pressure via their vasodilating effects.
- NPs act to decrease activation of the RAAS.
SNS Activity and Control
- SNS activity is regulated by receptor signaling, which includes alpha1 and alpha2 receptors that constrict vasculature and beta1 receptors that increase heart rate and contractility.
- Beta 2 receptors cause vasodilation.
- Norepinephrine and epinephrine cause the activation of SNS receptors.
- Phenylephrine is an alpha agonist that will cause vasoconstriction through the stimulation of alpha receptors.
Integration of ANS and CNS control
- Baroreceptors in the cardiovascular system and the CNS integrate to adjust heart rate and vascular tone.
- Autonomic nervous system activity to the vasculature and heart are regulated.
Important Clinical Considerations
- Orthostatic hypotension is a condition where blood pressure decreases significantly when moving from a supine to an upright position due to inadequate compensatory responses from the baroreflex arc and SNS.
- High blood pressure is a significant clinical concern for many people and is often associated with significant morbidity and mortality.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the role of the autonomic nervous system in regulating blood pressure through the sympathetic and parasympathetic nervous systems. It highlights the mechanisms of vasoconstriction, baroreceptor functions, and their effects on cardiac output and stroke volume.