Podcast
Questions and Answers
What happens to the damaged vessel during vasoconstriction?
What happens to the damaged vessel during vasoconstriction?
- It constricts to reduce blood flow (correct)
- It becomes inflamed to promote healing
- It dilates to increase blood flow
- It ruptures to release blood clots
What is the first stage of wound healing?
What is the first stage of wound healing?
- Hemostasis (correct)
- Remodeling
- Proliferation
- Inflammation
What is the main purpose of blood clotting or coagulation?
What is the main purpose of blood clotting or coagulation?
- To reduce the amount of platelets in the blood
- To promote blood flow through the damaged area
- To increase blood pressure
- To prevent excessive bleeding when a blood vessel is injured (correct)
What promotes platelets to adhere to the injury site?
What promotes platelets to adhere to the injury site?
What is the result of platelet degranulation?
What is the result of platelet degranulation?
What is the opposite of hemostasis?
What is the opposite of hemostasis?
What is the sequence of events in blood clotting?
What is the sequence of events in blood clotting?
What is the primary function of platelets in hemostasis?
What is the primary function of platelets in hemostasis?
What is the primary function of platelets in the blood?
What is the primary function of platelets in the blood?
What is the shape of activated platelets?
What is the shape of activated platelets?
What substance attracts more platelets to the affected area during blood clotting?
What substance attracts more platelets to the affected area during blood clotting?
What is the term for the sequence of events that leads to the formation of fibrin from inactive fibrinogen?
What is the term for the sequence of events that leads to the formation of fibrin from inactive fibrinogen?
What is the average size of platelets in microns?
What is the average size of platelets in microns?
What is the term for the plug formed by the aggregation of platelets and the trapping of red and white blood cells?
What is the term for the plug formed by the aggregation of platelets and the trapping of red and white blood cells?
What is the primary function of Von Willebrand factor (vWF) in blood clotting?
What is the primary function of Von Willebrand factor (vWF) in blood clotting?
What type of cells produce platelets?
What type of cells produce platelets?
What is the average lifespan of platelets in the human body?
What is the average lifespan of platelets in the human body?
What is the normal range of platelets per cubic millimeter of blood?
What is the normal range of platelets per cubic millimeter of blood?
What is the purpose of platelet count in diagnosing bleeding disorders?
What is the purpose of platelet count in diagnosing bleeding disorders?
What is the dilution ratio of blood to diluting fluid in the manual method of platelet count?
What is the dilution ratio of blood to diluting fluid in the manual method of platelet count?
What is the purpose of waiting for 10-15 minutes after mixing blood with diluting fluid?
What is the purpose of waiting for 10-15 minutes after mixing blood with diluting fluid?
What is the formula to calculate the total platelet count?
What is the formula to calculate the total platelet count?
What is the term for an increase in platelet count?
What is the term for an increase in platelet count?
What is the instrument used to count platelets in the manual method?
What is the instrument used to count platelets in the manual method?
Flashcards are hidden until you start studying
Study Notes
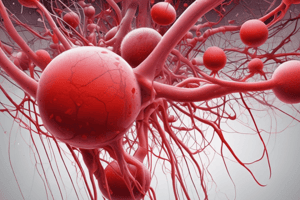
Blood Coagulation
- Blood clotting, or coagulation, prevents excessive bleeding when a blood vessel is injured.
- Platelets and proteins in plasma work together to stop the bleeding by forming a clot over the injury.
- Hemostasis, or haemostasis, is a process that causes bleeding to stop, meaning to keep blood within a damaged blood vessel.
Steps in Hemostasis
- Hemostasis has three major steps:
- Vasoconstriction (vascular spasm)
- Temporary blockage of a break by a platelet plug
- Blood coagulation, or formation of a fibrin clot
- These processes seal the hole until tissue is repaired.
Basic Events in Blood Clotting
- Vascular injury leads to vascular spasm, platelet plug formation, and blood coagulation.
- Vascular spasm (vasoconstriction) reduces blood flow through the area and limits blood loss.
Platelet Plug Formation
- Platelets adhere to damaged endothelium to form a platelet plug (primary hemostasis) and then degranulate.
- Plug formation is activated by a glycoprotein called Von Willebrand factor (vWF).
- Platelets express certain receptors, which are used for adhesion to collagen.
- When platelets are activated, they express glycoprotein receptors that interact with other platelets, producing aggregation and adhesion.
Clot Formation
- Once the platelet plug has been formed, clotting factors are activated in a sequence of events known as the 'coagulation cascade'.
- This leads to the formation of fibrin from inactive fibrinogen plasma protein.
- A fibrin mesh is produced around the platelet plug to hold it in place, a step called "Secondary Hemostasis".
Platelets
- Platelets are not cells, but small, irregularly shaped, non-nucleated fragments produced from large cells called megakaryocytes.
- Function: Platelets play an important role in stopping bleeding, so they are important in blood clotting.
- Shape: Platelets are spherical or rod-shaped and become oval or disc-shaped when inactivated.
- Size: The average size of platelets is 2-4 μm (microns).
- Life Span: The average lifespan of platelets is 3-10 days.
- Normal Range: About 150,000-450,000 cells are present per cubic millimeter (cmm) of blood.
Platelet Count
- The calculated number of platelets in a volume of blood, usually expressed as platelets per cubic millimeter (cmm) of whole blood.
- Platelet count is of great importance in helping to diagnose bleeding disorders.
- Methods: Automated method, blood smear, and manual method are used to count platelets.
Manual Method of Platelet Count
- Materials and instruments: whole fresh blood, RBC pipettes, haemocytometer, diluting fluid (ammonium oxalate 1%), microscope, petridish, filter paper, and lancet.
- Procedure: 1. Prick the finger and draw blood, then mix with diluting fluid. 2. Wait for 10-15 minutes for RBC hemolysis. 3. Discard the first 3-4 drops and fill the counting chamber. 4. Leave the chamber for 20 minutes to allow platelets to settle. 5. Count platelets under a microscope using lens power 10x and 40x.
- Calculations: Total platelet count = Total no. of platelets counted x 1000
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.