Podcast
Questions and Answers
What is the approximate length of the human small intestine?
What is the approximate length of the human small intestine?
- 10 meters
- 4-5 meters (correct)
- 6 meters
- 1.5 meters
What is the primary role of the stomach in drug absorption?
What is the primary role of the stomach in drug absorption?
- Breakdown of food into chyme (correct)
- Production of enzymes for digestion
- Storage and compaction of feces
- Absorption of most drugs
What is the typical pH range of the small intestine?
What is the typical pH range of the small intestine?
- 1-2
- 7-8
- 4-5
- 6-7 (correct)
What is the primary function of villi in the small intestine?
What is the primary function of villi in the small intestine?
What is the approximate ratio of surface area between the stomach and the small intestine?
What is the approximate ratio of surface area between the stomach and the small intestine?
Which of the following is NOT transported by the paracellular pathway?
Which of the following is NOT transported by the paracellular pathway?
Which of the following statements about the paracellular pathway is TRUE?
Which of the following statements about the paracellular pathway is TRUE?
Which of the following factors can INFLUENCE the bioavailability of a drug?
Which of the following factors can INFLUENCE the bioavailability of a drug?
What is the MAXIMUM molecular weight of a drug that can be efficiently transported by the paracellular pathway?
What is the MAXIMUM molecular weight of a drug that can be efficiently transported by the paracellular pathway?
How does the presence of food in the GI tract affect drug absorption?
How does the presence of food in the GI tract affect drug absorption?
Which of these best describes the movement of molecules in active transport?
Which of these best describes the movement of molecules in active transport?
What is a defining characteristic of carrier-mediated transport?
What is a defining characteristic of carrier-mediated transport?
Which of these are NOT transported via active transport? (Select all that apply)
Which of these are NOT transported via active transport? (Select all that apply)
Which of the following is a key difference between active and facilitated diffusion?
Which of the following is a key difference between active and facilitated diffusion?
Which transport mechanism(s) require(s) a concentration gradient for driving force?
Which transport mechanism(s) require(s) a concentration gradient for driving force?
What is the primary function of active transport in drug absorption?
What is the primary function of active transport in drug absorption?
Which of the following statements about active transport is TRUE?
Which of the following statements about active transport is TRUE?
Which type of endocytosis is considered non-specific and low efficiency?
Which type of endocytosis is considered non-specific and low efficiency?
What is the relationship between gastric emptying time and the nature of the dosage form?
What is the relationship between gastric emptying time and the nature of the dosage form?
How does the fed state affect gastric emptying?
How does the fed state affect gastric emptying?
What dosage form is expected to remain in the fed stomach longer?
What dosage form is expected to remain in the fed stomach longer?
What is the primary goal of the migrating myoelectric complex (MMC)?
What is the primary goal of the migrating myoelectric complex (MMC)?
In what manner should drugs be taken to reach the intestine quickly?
In what manner should drugs be taken to reach the intestine quickly?
Which of the following drugs is typically administered via enteric-coated tablets to influence absorption?
Which of the following drugs is typically administered via enteric-coated tablets to influence absorption?
How long does small intestinal transit typically take?
How long does small intestinal transit typically take?
Which physiological factor does NOT influence the absorption of drugs in the gastrointestinal tract?
Which physiological factor does NOT influence the absorption of drugs in the gastrointestinal tract?
Which of the following is NOT a factor that influences the rate of passive diffusion?
Which of the following is NOT a factor that influences the rate of passive diffusion?
Which of the following statements accurately describes the significance of the gastrointestinal membrane in drug absorption?
Which of the following statements accurately describes the significance of the gastrointestinal membrane in drug absorption?
Which type of transport mechanism is primarily responsible for the absorption of the majority of drugs across the gastrointestinal membrane?
Which type of transport mechanism is primarily responsible for the absorption of the majority of drugs across the gastrointestinal membrane?
In the equation dC/dt = k(Cg-Cb), what does Cb represent?
In the equation dC/dt = k(Cg-Cb), what does Cb represent?
Which of the following is a characteristic of passive diffusion?
Which of the following is a characteristic of passive diffusion?
What form of a weak electrolyte drug is generally more readily absorbed via passive diffusion?
What form of a weak electrolyte drug is generally more readily absorbed via passive diffusion?
Which of the following drugs is mentioned in the text as being affected by food-induced changes in presystemic metabolism?
Which of the following drugs is mentioned in the text as being affected by food-induced changes in presystemic metabolism?
Which of the following statements is TRUE regarding the environment within the lumen of the gastrointestinal tract?
Which of the following statements is TRUE regarding the environment within the lumen of the gastrointestinal tract?
What role does mucus play in the gastrointestinal epithelium?
What role does mucus play in the gastrointestinal epithelium?
What effect does the pyloric sphincter have on gastric residence time?
What effect does the pyloric sphincter have on gastric residence time?
Which factor can greatly influence the rate of passive diffusion in drug absorption?
Which factor can greatly influence the rate of passive diffusion in drug absorption?
Under what conditions are 'sink conditions' maintained during drug absorption?
Under what conditions are 'sink conditions' maintained during drug absorption?
What describes the absorption of small lipophilic molecules in the GI tract?
What describes the absorption of small lipophilic molecules in the GI tract?
Which statement is true about active transport mechanisms in the GI membrane?
Which statement is true about active transport mechanisms in the GI membrane?
What is the primary impact of food and gastrointestinal pH on drug absorption?
What is the primary impact of food and gastrointestinal pH on drug absorption?
Which mechanism is primarily responsible for drug absorption across the gastrointestinal membrane?
Which mechanism is primarily responsible for drug absorption across the gastrointestinal membrane?
Flashcards
Absorption in the small intestine
Absorption in the small intestine
The process of absorbing nutrients (e.g., drugs) from the small intestine.
Villi
Villi
Finger-like projections in the small intestine that increase surface area for absorption.
Chyme
Chyme
A creamy mixture of partially digested food in the stomach, ready to move to the small intestine.
Stomach's role in absorption
Stomach's role in absorption
Signup and view all the flashcards
Small intestine as primary absorption site
Small intestine as primary absorption site
Signup and view all the flashcards
Colon's microbial ecosystem
Colon's microbial ecosystem
Signup and view all the flashcards
Gastric emptying time
Gastric emptying time
Signup and view all the flashcards
Migrating myoelectric complex (MMC)
Migrating myoelectric complex (MMC)
Signup and view all the flashcards
Peristalsis in the fed state
Peristalsis in the fed state
Signup and view all the flashcards
Pyloric sphincter
Pyloric sphincter
Signup and view all the flashcards
Retropulsion
Retropulsion
Signup and view all the flashcards
Gastrointestinal pH and drug absorption
Gastrointestinal pH and drug absorption
Signup and view all the flashcards
Luminal enzymes and drug absorption
Luminal enzymes and drug absorption
Signup and view all the flashcards
Prodrug
Prodrug
Signup and view all the flashcards
Metabolism
Metabolism
Signup and view all the flashcards
Oral drug
Oral drug
Signup and view all the flashcards
Absorption
Absorption
Signup and view all the flashcards
Passive Diffusion
Passive Diffusion
Signup and view all the flashcards
Transcellular Transport
Transcellular Transport
Signup and view all the flashcards
Paracellular Transport
Paracellular Transport
Signup and view all the flashcards
Lipophilic molecule
Lipophilic molecule
Signup and view all the flashcards
Active transport
Active transport
Signup and view all the flashcards
Active transport examples
Active transport examples
Signup and view all the flashcards
Facilitated diffusion
Facilitated diffusion
Signup and view all the flashcards
Endocytosis
Endocytosis
Signup and view all the flashcards
Pinocytosis
Pinocytosis
Signup and view all the flashcards
Receptor-mediated endocytosis
Receptor-mediated endocytosis
Signup and view all the flashcards
Phagocytosis
Phagocytosis
Signup and view all the flashcards
Paracellular Pathway
Paracellular Pathway
Signup and view all the flashcards
Tight Junctions and Paracellular Pathway
Tight Junctions and Paracellular Pathway
Signup and view all the flashcards
Paracellular Pathway and Digestion
Paracellular Pathway and Digestion
Signup and view all the flashcards
P-glycoprotein and Drug Absorption
P-glycoprotein and Drug Absorption
Signup and view all the flashcards
Food & Drug Absorption
Food & Drug Absorption
Signup and view all the flashcards
Advantages of Oral Route
Advantages of Oral Route
Signup and view all the flashcards
GI Mucus: Role, Components, Turnover
GI Mucus: Role, Components, Turnover
Signup and view all the flashcards
Stomach: Volume, Roles, pH, MMC
Stomach: Volume, Roles, pH, MMC
Signup and view all the flashcards
Small Intestine and Colon: Roles, Length, pH
Small Intestine and Colon: Roles, Length, pH
Signup and view all the flashcards
Gastric Motility: Fasting, Fed States, Residence Time
Gastric Motility: Fasting, Fed States, Residence Time
Signup and view all the flashcards
Gastric Residence Time: Dosage Form, Food
Gastric Residence Time: Dosage Form, Food
Signup and view all the flashcards
GI Membrane: Characteristics, Transport Mechanisms
GI Membrane: Characteristics, Transport Mechanisms
Signup and view all the flashcards
Active Transport: Carriers, Energy, Saturation
Active Transport: Carriers, Energy, Saturation
Signup and view all the flashcards
Study Notes
Biopharmaceutics Part A
- Aulton chapter 19, 20
- Topics covered include GI tract physiology, drug absorption, pharmaceutical transit, GI barriers, and drug transport mechanisms.
- Oral route is the most common drug administration method.
Objectives
- Students should understand the GI tract physiology for drug absorption.
- Students should understand the transit of pharmaceuticals in the GI tract.
- Students should understand barriers to drug absorption in the GI tract.
- Students should know GI membrane structures and drug transport mechanisms.
GI Tract - Physiology and Drug Absorption
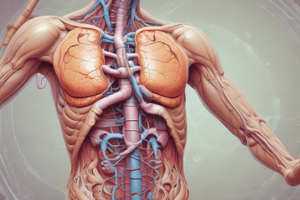
- GI Tract is 6 meters long and has four main segments: esophagus, stomach, small intestine, and large intestine.
- Mucous lining covers the GI epithelium and acts as a viscoelastic aqueous gel, composed of large glycoproteins called mucins. The average thickness is 80 µm (ranging from 5 to 500 µm).
Stomach
- Stomach's volume under fasting conditions.
- Chyme is the uniform creamy consistency in the stomach.
- Absorption? (Question, with no definite answer in provided information)
- Stomach pH and secretions: acid, gastrin, pepsin, and mucus.
- The pyloric sphincter is crucial in regulating stomach emptying.
Small Intestine
- Length is 4-5 meters.
- pH? (Question, with no specific pH value).
- Villi are finger-like projections into the lumen, roughly 0.5-1.5 mm in length and 0.1 mm in diameter. Each villus has 600-1000 microvilli.
- Roles of the small intestine: major site of nutrient absorption.
- Duodenum, jejunum, and ileum are the sections of the small intestine, relevant for absorption.
- Ratio of stomach to small intestine surface area is 1 to 3800.
Colon
- Length is approximately 1.5 meters.
- Roles of the colon: absorption of sodium ions, chloride ions, and water; storage and compaction of feces; presence of bacteria.
- Colon is colonized by bacteria. The bacteria in the colon can affect certain medications.
Transit of Pharmaceuticals in GI Tract
- Gastric emptying time is equal to gastric residence time, which is highly variable, and is dependent on the nature of the dosage form and the fed/fasting state.
- The presence of food can significantly impact the transit time of pharmaceuticals.
Interdigestive Myoelectric Cycle
- Also known as the migrating myoelectric complex (MMC).
- Occurs in the fasting state.
- Describes the stages of the myoelectric cycle (e.g. phases I-III).
- MMC plays a role in removing undigested food and preventing bacterial overgrowth.
Fed State
- Peristalsis—contraction of the distal stomach
- Mixes and breaks down food and moves towards pyloric sphincter.
- Emptying and retropulsing into the stomach's antrum (The action of retropulsing)
- Which dosage form stays in the stomach for longer if fed? Extended release dosage forms are the answer.
Gastric Emptying of Drugs
- For rapid intestinal drug delivery, dosage form should be taken without food and/or water.
Small Intestinal and Colonic Transit
- Small intestinal transit is relatively constant, at around 3-4 hours.
- Colonic transit can range from 2-48 hours.
Barriers to Drug Absorption
- Barriers to drug absorption in the GI tract include unstirred water layer, presystemic metabolism, chemical degradation, enzymatic degradation, complexation to mucus, adsorption, water and mucus diffusion, and efflux.
- Gastrointestinal pH.
Environment within the Lumen
- GI pH can influence drug absorption (enteric coated tablets can be used to target pH).
- Importance of drugs with examples.
- GI lumen enzymes may affect drugs, with example of sulfasalazine.
- Food components (food-drug interactions) can affect drug absorption, with example of tetracycline.
- Disease state and physiological disorders (e.g., local diseases, gastric surgery) can alter drug absorption.
GI Membrane and Mechanisms of Drug Transport
- GI membrane is the major cellular barrier to drug absorption and is semi-permeable.
Mechanisms of Drug Transport Across the Membrane
- Several transport mechanisms exist: Paracellular (between cells), Transcellular (across cells), Passive diffusion, carrier mediated transport (active transport, facilitated diffusion), and Endocytosis (pinocytosis and phagocytosis).
Passive Diffusion
- Drugs move from higher to lower concentration across GI membrane.
- Rate of transport depends on physicochemical properties of the drug, nature of the membrane, and concentration gradient.
- Factors like the diffusion coefficient, surface area, and membrane thickness affect the rate.
Carrier-mediated Transport: Active Transport
- Energy-dependent process.
- Transport can occur against concentration gradients.
- Transporters show specificity towards particular compounds (e.g., nutrients, amino acids, sugars, electrolytes, vitamins B1, B2, B12, bile salts); these transporters are vital for absorption.
Carrier-mediated Transport: Facilitated Diffusion
- No energy input.
- Similar to active transport, shows dependence on specific chemical structures.
- Plays a minor role in drug absorption.
Review Questions
- Small intestine's material transit is relatively constant.
- Food's presence might increase or reduce drug absorption.
- The transit of materials through the small intestine is relatively constant.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz focuses on the gastrointestinal tract's physiology and its essential role in drug absorption. Key topics include the anatomy of the GI tract, drug transport mechanisms, and barriers to absorption. Understanding these principles is crucial for mastering pharmaceutical studies.