Podcast
Questions and Answers
What is the primary function of the liver in relation to clinical biochemistry tests?
What is the primary function of the liver in relation to clinical biochemistry tests?
The liver plays a crucial role in detoxification, metabolism, and energy production, which is reflected in various clinical biochemistry tests.
What is the purpose of liver function tests in diagnosing liver disorders?
What is the purpose of liver function tests in diagnosing liver disorders?
Liver function tests are used to assess liver damage, detect liver disease, and monitor the progression of liver disorders.
What is the difference between cirrhosis and portal hypertension in terms of liver damage?
What is the difference between cirrhosis and portal hypertension in terms of liver damage?
Cirrhosis is a condition where liver tissue is replaced by scar tissue, leading to liver failure, while portal hypertension is a complication of cirrhosis characterized by high blood pressure in the portal vein.
What is the significance of a biochemical test profile in diagnosing liver disorders?
What is the significance of a biochemical test profile in diagnosing liver disorders?
How do selected pathological processes alter the biochemical profile in liver disorders?
How do selected pathological processes alter the biochemical profile in liver disorders?
What is the importance of comparing and contrasting various mechanisms of liver damage in understanding liver disorders?
What is the importance of comparing and contrasting various mechanisms of liver damage in understanding liver disorders?
What is the functional unit of the liver?
What is the functional unit of the liver?
What are the three zones of the liver acinus, in order of proximity to the portal triad?
What are the three zones of the liver acinus, in order of proximity to the portal triad?
Which zone of the liver acinus has the highest metabolic potential?
Which zone of the liver acinus has the highest metabolic potential?
What process occurs in Zone 3 of the liver acinus?
What process occurs in Zone 3 of the liver acinus?
Which zone of the liver acinus is most susceptible to hypoxia?
Which zone of the liver acinus is most susceptible to hypoxia?
What is the function of the urea cycle in Zone 1 of the liver acinus?
What is the function of the urea cycle in Zone 1 of the liver acinus?
What is the direction of blood flow in the 'classic' lobule of the liver?
What is the direction of blood flow in the 'classic' lobule of the liver?
What is the primary function of the sinusoidal capillary system in the liver?
What is the primary function of the sinusoidal capillary system in the liver?
What is the role of Zone 1 hepatocytes in the liver?
What is the role of Zone 1 hepatocytes in the liver?
What is the estimated number of functions served by the liver?
What is the estimated number of functions served by the liver?
What is the primary function of the bile canaliculi in the liver?
What is the primary function of the bile canaliculi in the liver?
What is the difference between liver function and integrity tests?
What is the difference between liver function and integrity tests?
What is the term for the organization of the liver into functional units that consider the sinusoidal and biliary systems?
What is the term for the organization of the liver into functional units that consider the sinusoidal and biliary systems?
What is the name of the hormone produced by the liver that regulates blood clotting?
What is the name of the hormone produced by the liver that regulates blood clotting?
What is the main source of bilirubin?
What is the main source of bilirubin?
What is necessary for bilirubin to be excreted?
What is necessary for bilirubin to be excreted?
What is the main function of albumin in relation to bilirubin?
What is the main function of albumin in relation to bilirubin?
What is the significance of elevated bilirubin levels in neonates?
What is the significance of elevated bilirubin levels in neonates?
What is the primary function of ALT in relation to liver biochemistry?
What is the primary function of ALT in relation to liver biochemistry?
What is the significance of GGT in relation to liver biochemistry?
What is the significance of GGT in relation to liver biochemistry?
What is the significance of bilirubin in relation to liver biochemistry?
What is the significance of bilirubin in relation to liver biochemistry?
What is the primary function of albumin in relation to liver biochemistry?
What is the primary function of albumin in relation to liver biochemistry?
What is the primary clinical indication of cholestasis?
What is the primary clinical indication of cholestasis?
In a patient with primary biliary cirrhosis, what is the expected laboratory profile?
In a patient with primary biliary cirrhosis, what is the expected laboratory profile?
What is the primary difference between the laboratory profiles of a patient with focal biliary tract obstruction and a patient with primary biliary cirrhosis?
What is the primary difference between the laboratory profiles of a patient with focal biliary tract obstruction and a patient with primary biliary cirrhosis?
In a patient with viral hepatitis, what is the primary mechanism of liver damage?
In a patient with viral hepatitis, what is the primary mechanism of liver damage?
What is the expected laboratory profile in a patient with chronic viral hepatitis?
What is the expected laboratory profile in a patient with chronic viral hepatitis?
What is the primary distinction between the laboratory profiles of a patient with acute viral hepatitis and a patient with chronic viral hepatitis?
What is the primary distinction between the laboratory profiles of a patient with acute viral hepatitis and a patient with chronic viral hepatitis?
In a patient with alcoholic hepatitis, what is the expected laboratory profile?
In a patient with alcoholic hepatitis, what is the expected laboratory profile?
What is the primary mechanism of liver damage in a patient with primary sclerosing cholangitis?
What is the primary mechanism of liver damage in a patient with primary sclerosing cholangitis?
In a patient with acute hepatitis, what is the primary laboratory indicator of liver damage?
In a patient with acute hepatitis, what is the primary laboratory indicator of liver damage?
What is the primary clinical indication of cirrhosis?
What is the primary clinical indication of cirrhosis?
What is the primary metabolite of heme that requires glucuronidation for excretion?
What is the primary metabolite of heme that requires glucuronidation for excretion?
What liver function test is more specific for hepatocyte injury?
What liver function test is more specific for hepatocyte injury?
What enzyme is indicative of both hepatocyte integrity and biliary tract patency?
What enzyme is indicative of both hepatocyte integrity and biliary tract patency?
What is the primary function of albumin in relation to bilirubin?
What is the primary function of albumin in relation to bilirubin?
What is the significance of elevated bilirubin levels in neonates?
What is the significance of elevated bilirubin levels in neonates?
What is the primary function of liver function tests?
What is the primary function of liver function tests?
What is the difference between liver function tests and liver integrity tests?
What is the difference between liver function tests and liver integrity tests?
What is the primary clinical indication of cholestasis?
What is the primary clinical indication of cholestasis?
In which zone of the liver acinus is gluconeogenesis primarily located, and what is the significance of this zone's metabolic function in liver disease diagnosis?
In which zone of the liver acinus is gluconeogenesis primarily located, and what is the significance of this zone's metabolic function in liver disease diagnosis?
How do the metabolic functions of Zone 1 and Zone 3 hepatocytes differ, and what are the implications for liver function tests?
How do the metabolic functions of Zone 1 and Zone 3 hepatocytes differ, and what are the implications for liver function tests?
What is the significance of hypoxia susceptibility in Zone 3 hepatocytes, and how does this impact liver disease diagnosis?
What is the significance of hypoxia susceptibility in Zone 3 hepatocytes, and how does this impact liver disease diagnosis?
What is the relationship between CYP450 metabolism in Zone 3 hepatocytes and liver disease diagnosis, particularly in cases of xenobiotic exposure?
What is the relationship between CYP450 metabolism in Zone 3 hepatocytes and liver disease diagnosis, particularly in cases of xenobiotic exposure?
How does the biliary tract patency impact liver function tests, and what are the implications for liver disease diagnosis?
How does the biliary tract patency impact liver function tests, and what are the implications for liver disease diagnosis?
What is the significance of hepatocyte integrity in liver disease diagnosis, particularly in cases of cirrhosis and portal hypertension?
What is the significance of hepatocyte integrity in liver disease diagnosis, particularly in cases of cirrhosis and portal hypertension?
What is the primary laboratory indicator of liver damage in a patient with cholestasis?
What is the primary laboratory indicator of liver damage in a patient with cholestasis?
How do you explain the lab profile of a patient with focal biliary tract obstruction?
How do you explain the lab profile of a patient with focal biliary tract obstruction?
What is the primary mechanism of liver damage in a patient with acute viral hepatitis?
What is the primary mechanism of liver damage in a patient with acute viral hepatitis?
What is the expected laboratory profile in a patient with chronic viral hepatitis?
What is the expected laboratory profile in a patient with chronic viral hepatitis?
What is the primary distinction between the laboratory profiles of a patient with acute viral hepatitis and a patient with chronic viral hepatitis?
What is the primary distinction between the laboratory profiles of a patient with acute viral hepatitis and a patient with chronic viral hepatitis?
What is the primary laboratory indicator of hepatocellular damage in a patient with liver disease?
What is the primary laboratory indicator of hepatocellular damage in a patient with liver disease?
How do you explain the lab profile of a patient with primary sclerosing cholangitis?
How do you explain the lab profile of a patient with primary sclerosing cholangitis?
What is the primary mechanism of liver damage in a patient with alcoholic hepatitis?
What is the primary mechanism of liver damage in a patient with alcoholic hepatitis?
What is the expected laboratory profile in a patient with cirrhosis?
What is the expected laboratory profile in a patient with cirrhosis?
What is the primary clinical indication of liver disease?
What is the primary clinical indication of liver disease?
Study Notes
Objectives
- Present the clinical significance of blood and urine laboratory tests in relation to liver disorders
- Explain how selected pathological processes alter the biochemical profile
- Review a spectrum of liver disorders emphasizing the derangements in the biochemistry test profile
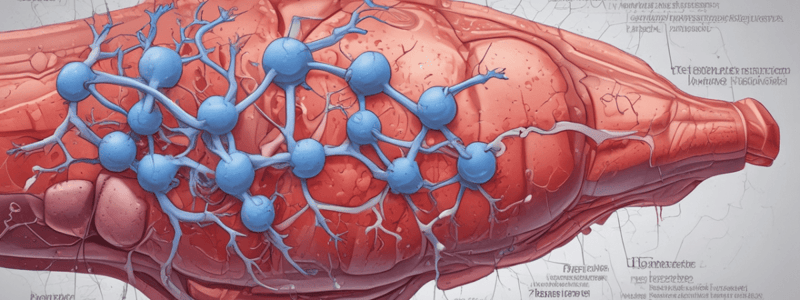
Liver Anatomy
- The acinus is the functional unit of the liver, centered around the connection between two portal triads and extending towards two central veins
- Divided into three zones in order of proximity to the portal triad:
- Zone 1: first hepatocytes to receive incoming blood
- Zone 2: intermediate range
- Zone 3: last hepatocytes to receive incoming blood
- Zone comparisons are relative to each other, and enough hypoxia can cause death of Zone 1 hepatocytes
- Hepatocytes concurrently excrete bile into the bile canaliculi to be excreted via bile ducts
Liver Function
- The liver serves around 500 functions, including:
- Biosynthesis (cholesterol, lipoproteins, glucose, etc.)
- Storage (vitamins, trace elements, etc.)
- Endocrine (IGF-1, thrombopoietin, angiotensinogen, etc.)
- Protein synthesis (albumin, clotting factors, globulins, etc.)
- Detoxification (drugs, nitrogenous waste, bilirubin, etc.)
- Laboratory tests can assess intrahepatic processes via function and integrity tests
- Function tests indicate the capacity of hepatocytes to carry out biological functions
- Integrity tests indicate the intactness of hepatocyte membranes
- Tests for extrahepatic processes assess the patency of the biliary system (cholestasis)
Liver Function: Bilirubin
- Bilirubin is a catabolic product of heme, mainly metabolized in the liver and excreted via bile
- Increasing levels may indicate failing liver function
- High bilirubin levels can also be a result of inborn errors of metabolism
- Toxic to neonates (kernicterus)
Liver Biochemistry
- Laboratory tests can help identify if liver disease is present
- Tests include:
- Alanine aminotransferase (ALT): hepatocyte integrity; more specific for hepatocyte injury
- Aspartate aminotransferase (AST): hepatocyte integrity; less specific for hepatocyte injury
- Alkaline phosphatase (ALP): biliary tract patency
- Gamma-glutamyltransferase (GGT): hepatocyte integrity and biliary tract patency
- Bilirubin: hepatocyte function and biliary tract patency
- Albumin: hepatocyte function (protein synthesis)
- Prothrombin time: hepatocyte function (protein synthesis)
- Specialized tests include:
- Ammonia: metabolic insufficiency
- ɑ-fetoprotein: hepatoma
- 5’-nucleotidase: cholestasis
- Lactate dehydrogenase: metastases, congestion
- ɑ1-antitrypsin: cirrhosis etiology
- Caeruloplasmin: cirrhosis etiology
- Iron, ferritin, TIBC: cirrhosis etiology
- Viral antigens and antibodies: hepatitis
- Immunoglobulins: chronic disease
- Autoantibodies: chronic disease
- Acetaminophen: overdose
Liver Disease: Cholestasis
- Cholestasis refers to the inability of bile to flow from the liver to the duodenum
- Causes include:
- Obstructive (extrahepatic) etiology (gallstones, tumors, primary sclerosing cholangitis)
- Infectious (infections, autoimmune disease, genetic disorders)
- Drug/toxin-induced
- Laboratory tests:
- ALP: very high; 10-20x upper limit of normal (ULN)
- TBil: high; parallel fold increase as ALP
- DBil: high; should account for most of TBil
- AST/ALT: normal or slightly elevated
- Albumin: normal
Liver Disease: Hepatitis
- Hepatitis is the inflammation of liver tissue
- Can be classified according to:
- Duration: acute, fulminant, chronic
- Cause: infectious (viral), alcoholic, toxic, autoimmune, ischemic, inherited, NAFLD
- Any chronic insult to the liver can lead to cirrhosis (extensive liver fibrosis + additional correlates)
- Laboratory tests may give an indication of degree of damage and/or chronicity
- In a patient with alcoholic hepatitis:
- AST/ALT: high; 10x ULN
- ALT: very high; >10x ULN
- DBil: very high
- IBil: very high
- In a patient with acute viral hepatitis (Hepatitis A):
- AST: very high; >10x ULN
- ALT: very high; >10x ULN
- TBil: normal or slightly elevated
- Albumin: normal
- In a patient with chronic viral hepatitis (Hepatitis C):
- AST: high; waxing and waning
- ALT: high; waxing and waning
- TBil: elevated
- Albumin: decreased
Liver Function: Bilirubin
- Bilirubin is a catabolic product of heme, a yellow pigment that can cause jaundice
- Mainly metabolized in the liver and excreted via bile; increasing levels may indicate failing liver function
- High bilirubin levels can also result from inborn errors of metabolism and are toxic to neonates, causing kernicterus
- Majority (85%) of bilirubin is derived from hemoglobin, with the remainder from other heme proteins
- Bilirubin is highly insoluble and travels to the liver bound to albumin
- Requires glucuronidation to be excretable, with the majority being di-glucuronide (90%)
Liver Biochemistry
- Alanine aminotransferase (ALT): indicates hepatocyte integrity and is more specific for hepatocyte injury
- Aspartate aminotransferase (AST): indicates hepatocyte integrity, but is less specific for hepatocyte injury
- Alkaline phosphatase (ALP): indicates biliary tract patency
- Gamma-glutamyltransferase (GGT): indicates hepatocyte integrity and biliary tract patency
- Bilirubin: indicates hepatocyte function and biliary tract patency
- Albumin: indicates hepatocyte function (protein synthesis)
- Prothrombin Time: indicates hepatocyte function (protein synthesis)
Liver Integrity Tests vs. Liver Function Tests
- Liver integrity tests: ALT, AST, GGT; indicate cellular damage
- Liver function tests: total bilirubin, direct bilirubin, albumin, prothrombin time; indicate liver's ability to perform its functions
- Note: function does not equal integrity; institutions may have a "liver function" panel that includes both function and integrity tests
Specialized Tests
- Ammonia: indicates metabolic insufficiency
- α-fetoprotein: indicates hepatoma
- 5'-nucleotidase: indicates cholestasis
- Lactate dehydrogenase: indicates metastases, congestion
- α1-antitrypsin: indicates cirrhosis etiology
- Caeruloplasmin: indicates cirrhosis etiology
- Iron, Ferritin, TIBC: indicates cirrhosis etiology
- Viral antigens and antibodies: indicates hepatitis
- Immunoglobulins: indicates chronic disease
- Autoantibodies: indicates chronic disease
- Acetaminophen: indicates overdose
Liver Disease: Cholestasis
- Cholestasis refers to the inability of bile to flow from the liver to the duodenum
- Most often caused by obstructive (extrahepatic) etiology, such as gallstones, tumors, or primary sclerosing cholangitis
- Other causes include infections, autoimmune disease, genetic disorders, and drug/toxin-induced
- Bilirubin and urobilinogen in the urine indicate cholestasis
Liver Disease: Cholestasis (Lab Profiles)
- In a patient with diffuse biliary tract obstruction (primary biliary cirrhosis):
- ALP is very high (>10x ULN)
- TBil is high, with a parallel fold increase as ALP
- DBil is high, accounting for most of TBil
- AST/ALT are normal or slightly elevated
- Albumin is normal
- In a patient with focal biliary tract obstruction (gallstone):
- ALP is very high
- GGT is very high
- DBil is high, but not as high as ALP increase
- AST/ALT are normal or slightly elevated
- Albumin is normal
- In a patient with primary sclerosing cholangitis:
- ALP is low (10x ULN)
- ALT is very high (>10x ULN)
- DBil is very high
- IBil is very high
- In a patient with viral hepatitis (Hepatitis A):
- AST is very high (>10x ULN)
- ALT is very high (>10x ULN)
- TBil is normal or slightly elevated
- Albumin is normal
- In a patient with chronic viral hepatitis (Hepatitis C):
- AST is high, waxing and waning
- ALT is high, waxing and waning
- TBil is elevated
- Albumin is decreased
Liver Anatomy
- The acinus is the functional unit of the liver, centered around the connection between two portal triads and extending towards two central veins
- Divided into 3 zones in order of proximity to the portal triad: Zone 1 (first hepatocytes to receive incoming blood), Zone 3 (last hepatocytes to receive incoming blood), and Zone 2 (intermediate range)
- Each zone has different functions, metabolic potential, and susceptibility to hypoxia, bile stasis, and toxins
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Quiz on liver disorders, covering clinical significance of blood and urine laboratory tests and test profiles.