Podcast
Questions and Answers
Which bacterium is the most common cause of community-acquired meningitis in previously healthy adults?
Which bacterium is the most common cause of community-acquired meningitis in previously healthy adults?
- Streptococcus pneumoniae (correct)
- Neisseria meningitidis
- Listeria monocytogenes
- Haemophilus influenzae type b
What characteristic is used to classify Neisseria meningitidis into different serogroups?
What characteristic is used to classify Neisseria meningitidis into different serogroups?
- Metabolic activity
- Capsular polysaccharide antigens (correct)
- Cell wall structure
- Gram staining reaction
What is a common symptom of meningitis?
What is a common symptom of meningitis?
- Rash on the abdomen
- Neck stiffness (correct)
- Shortness of breath
- Chest pain
Which age group is commonly affected by Haemophilus influenzae type b meningitis?
Which age group is commonly affected by Haemophilus influenzae type b meningitis?
What is the primary site for colonization of Neisseria meningitidis in humans?
What is the primary site for colonization of Neisseria meningitidis in humans?
What are the two main types of meningococcal disease?
What are the two main types of meningococcal disease?
Which medium is NOT commonly used for culturing meningococci?
Which medium is NOT commonly used for culturing meningococci?
What is the optimum temperature range for the growth of meningococci?
What is the optimum temperature range for the growth of meningococci?
How are meningococci primarily detected in cerebrospinal fluid?
How are meningococci primarily detected in cerebrospinal fluid?
Which of the following is the treatment of choice for meningococcal disease?
Which of the following is the treatment of choice for meningococcal disease?
Flashcards
Meningococci Growth Requirements
Meningococci Growth Requirements
Meningococci require special media like blood agar, enriched with blood, serum or ascetic fluid to grow.
Meningococci Temperature Preference
Meningococci Temperature Preference
Meningococci prefer a warm environment, growing best at 35-36°C and struggling below 30°C.
Meningococci pH Preference
Meningococci pH Preference
Meningococci need a slightly acidic environment, with an ideal pH of 7.4-7.6.
Meningococci CO2 Requirement
Meningococci CO2 Requirement
Signup and view all the flashcards
Meningococci Colony Appearance
Meningococci Colony Appearance
Signup and view all the flashcards
Neisseria meningitidis
Neisseria meningitidis
Signup and view all the flashcards
Nasopharynx
Nasopharynx
Signup and view all the flashcards
Capsular polysaccharide
Capsular polysaccharide
Signup and view all the flashcards
Meningococcemia
Meningococcemia
Signup and view all the flashcards
Epidemic Cerebrospinal Meningitis
Epidemic Cerebrospinal Meningitis
Signup and view all the flashcards
Study Notes
Bacterial Meningitis
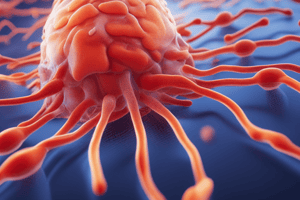
- Bacterial meningitis is an infection of the membranes surrounding the brain and spinal cord.
- Common causes include Streptococcus pneumoniae, Neisseria meningitidis (meningococcus), Haemophilus influenzae type b (Hib), and Listeria monocytogenes.
- Hib was a common cause of meningitis in children, especially young ones.
- Listeria monocytogenes can affect older adults, pregnant women, or people with weakened immune systems.
- Other bacteria, including Staphylococcus aureus, streptococci, and pseudomonas, can also cause meningitis.
- Spirochetes are another possible bacterial cause.
Symptoms of Meningitis
- Headache is a common symptom
- Fever is a common symptom
- Vomiting is a common symptom
- Stiff neck (nuchal rigidity) along with joint pains
- Drowsiness or confusion
- Photophobia (sensitivity to light)
Neisseria meningitidis
- Morphology: Small, gram-negative diplococci, typically arranged in pairs with flattened sides.
- Common cause (second only to Streptococcus pneumoniae) of community-acquired meningitis in healthy adults.
- Disease transmission is person-to-person via aerosolization of respiratory tract secretions in crowded areas.
- The nasopharynx is the primary site for meningococci colonisation.
- Individuals can transmit infection without showing symptoms (carriers).
Virulence Factors in Neisseria meningitidis
- Pili-mediated colonization of the nasopharynx
- Antiphagocytic polysaccharide capsule facilitating spread without specific immunity.
- Lipooligosaccharide (a component of the bacterial outer membrane)
- IgA proteases, which break down antibodies
Classification of Neisseria meningitidis
- Meningococci are encapsulated, unlike other Neisseria.
- Classified into serogroups based on capsular polysaccharide antigens.
- Important serogroups include A, B, C, Y, and W135; these account for about 90% of infections.
- Serogroup A is frequently associated with epidemics.
Pathogenesis/Clinical Picture
- Incubation period of two to three days before onset.
- Sudden onset characterized by severe headache, fever, neck stiffness, and skin rash.
- Severe hemorrhagic sepsis may develop.
- Types of meningococcal disease include epidemic cerebrospinal meningitis and meningococcal septicaemia.
Cultural Characteristics of Meningococci
- Meningococci do not grow on ordinary media.
- Growth requires enriched media like blood, serum, or ascites fluid.
Laboratory Diagnosis
- Examination of cerebrospinal fluid (CSF) for cocci; the fluid typically is under pressure and turbid (cloudy) and high in pus cells
- Gram staining of CSF reveals the bacterium inside white blood cells.
- Inoculation of the second portion of CSF onto media like blood agar, chocolate agar, or Thayer-Martin medium, incubated in CO2-enriched conditions, following 18 - 24 hours; results in the identification of bacteria by morphology and biochemical reactions
- Positive tests for catalase and oxidase
- Acid production from glucose and maltose
- Blood cultures are often positive in cases of meningococcema and early meningitis (in the 4 to 7 days).
- Additional methods include:
- Nasopharyngeal swab (detection of carriers)
- Observation of petechial lesions
- Molecular diagnosis via PCR amplification of meningococcal DNA in CSF or blood
Treatment for Bacterial Meningitis
- Intravenous penicillin G is often a first-line treatment.
- Other third-generation cephalosporins (e.g., cefotaxime or ceftriaxone) or chloramphenicol may be used, depending on sensitivity.
- Treatment choice is adjusted based on antimicrobial susceptibility testing.
- Vancomycin may be used for penicillin-resistant strains.
- Cephalosporins and erythromycin may be used in those allergic to penicillin.
Streptococcus pneumoniae
- Endogenous spread often begins in the nasopharynx/oropharynx and spreads in distal tissues via the blood or lungs/sinuses/ears/blood/meninges
- Frequently a secondary infection, following the flu.
- Young children and elderly are most at risk for meningitis.
- Five to 75% of the population carry the bacteria.
Streptococcus pneumoniae: Virulence Factors
- Polysaccharide capsule: Inhibits phagocytosis.
- Pneumolysin: Membrane-damaging toxin that has cytotoxic and complement-activating properties.
- IgA protease: Breaks down IgA antibodies.
- Autolysin: Causes the lysis of pneumococci.
Clinical Diseases in Streptococcus pneumoniae
- Lobar pneumonia
- Sinusitis
- Otitis media
- Meningitis (local spread from mastoid, hematogenous spread from bacteremia)
Laboratory Diagnosis for Streptococcus pneumoniae
- Using samples like sputum, CSF, blood, and synovial fluid.
- Microscopy reveals gram-positive, lanceolate-shaped diplococci with numerous pus cells.
- Quellung reaction identifies capsular swelling using type-specific antiserum and methylene blue solution.
- Antigen detection uses passive latex agglutination or ELISA.
- Culture on blood agar at 37°C in 5% CO2.
- Microscopy using Gram’s stain.
- Testing for solubility in bile
- Optochin sensitivity
- Biochemical reactions (ferment Inulin)
Prophylaxis for Bacterial Meningitis
- Pneumococcal Conjugate Vaccine (PCV13 or Prevnar 13®) (recommended doses for children < 2, 4, 6, 18 months of age)
- Pneumococcal Polysaccharide Vaccine (PPSV23 or Pneumovax23®) (for adults > 65 or those with certain medical conditions/smokers)
- Chemoprophylaxis of close contacts with rifampin.
Haemophilus influenzae
- Fastidious gram-negative coccobacilli that colonize mucosal surfaces.
- Types b and other non-typable varieties can trigger infections.
- Factors V (NAD+) and X (hematin) are required for successful growth.
Haemophilus influenzae Clinical Features
- Preschool children, who may exhibit pyogenic meningitis, acute epiglottitis, septicemia, facial cellulitis, or osteomyelitis.
- Usually a commensal in nasopharyn; may cause otitis media, sinusitis, and chest infections in patients with obstructive airways disease in adults
Haemophilus influenzae Laboratory Diagnosis
- Gram staining reveals gram-negative, pleomorphic coccobacilli.
- Biochemical reactions such as positive tests for oxidase and catalase
- Requires factors V (NAD+) and X (hematin) for growth
- Most strains does not grow on 5% Sheep Blood Agar; Growth on Chocolate agar;
- Some strains may display satellite growth around colonies of Staphylococcus aureus (due to production of NAD by Staphylococci).
- Antigen detection using direct and indirect immunofluorescence; Multiplex nucleic acid amplification tests (NAATs).
Haemophilus influenzae Treatment and Prevention
- Ampicillin, chloramphenicol, or third-generation cephalosporins (e.g., ceftriaxone or cefotaxime)
- Treatment usually spans 10 days.
- If Beta-lactamase is detected, Ceftriaxone is the treatment of choice.
- Hib conjugate vaccine is recommended for children under 5.
- Vaccination protects against Hib type b meningitis, epiglottitis and other infections.
- Infants receive 2, 4, and 6 month vaccinations.
- Booster dose given 15 to 18 months post initial infection.
Tuberculous Meningitis (TBM)
- TBM is the most common form of CNS tuberculosis; often fatal, due to its high morbidity/mortality.
- Typically a subacute disease; symptoms can persist for weeks before diagnosis.
- Cerebrospinal fluid (CSF) analysis often reveals a high number of lymphocytes, elevated protein levels, and low glucose levels.
- CSF acid-fast smear and culture may help diagnosis.
- Nucleic acid amplification tests (PCR) applied to CSF can be highly specific.
Tuberculous Meningitis (TBM) Treatment
- Empiric treatment incorporating first-line drugs, including isoniazid, rifampin, pyrazinamide, and either streptomycin or ethambutol, should be initiated promptly given suspected diagnosis.
- Adjunctive treatment with corticosteroids can improve mortality rate.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.