Podcast
Questions and Answers
What is one of the key stages of atherosclerosis?
What is one of the key stages of atherosclerosis?
- Inflammation and complications (correct)
- Endothelial regeneration
- Arterial constriction
- Excessive lipid breakdown
What is the primary role of endothelial cells in blood vessels?
What is the primary role of endothelial cells in blood vessels?
- Producing white blood cells
- Regulating blood flow (correct)
- Stimulating clot formation
- Breaking down lipids
What happens when LDL particles deposit in the arterial intima?
What happens when LDL particles deposit in the arterial intima?
- They get excreted from the body
- They reduce inflammation
- They become oxidized (correct)
- They transform into HDL particles
How does endothelial dysfunction contribute to the development of atherosclerosis?
How does endothelial dysfunction contribute to the development of atherosclerosis?
What are atheromas primarily composed of?
What are atheromas primarily composed of?
Which factor attracts immune cells like macrophages to LDL deposits?
Which factor attracts immune cells like macrophages to LDL deposits?
What is the role of foamy macrophages in atherosclerosis?
What is the role of foamy macrophages in atherosclerosis?
How does chronic inflammation contribute to atherosclerosis?
How does chronic inflammation contribute to atherosclerosis?
Which structure provides structural support for the growing atherosclerotic lesion?
Which structure provides structural support for the growing atherosclerotic lesion?
What complication can result from atherosclerotic renal artery stenosis?
What complication can result from atherosclerotic renal artery stenosis?
In atherosclerosis, what role does smooth muscle cell behavior play?
In atherosclerosis, what role does smooth muscle cell behavior play?
What can be a consequence of luminal narrowing due to atherosclerosis?
What can be a consequence of luminal narrowing due to atherosclerosis?
Flashcards are hidden until you start studying
Study Notes
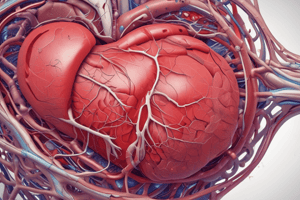
Atherosclerosis is a complex, multi-factorial disease characterized by the progressive accumulation of lipids and macrophages in the inner layers of large and medium-sized arteries. Its pathology involves several key stages, including endothelial dysfunction, atheroma formation, plaque development, inflammation, and complications.
Endothelial Dysfunction
Endothelial cells play a critical role in maintaining healthy blood vessels. They produce nitric oxide (NO), which helps regulate blood flow and protect against blood clots. However, when blood flow becomes disrupted, such as during periods of stress or inflammation, endothelial cells can become damaged, leading to impaired NO production and reduced vasodilation capacity. This decrease in NO and vasodilatory capacity contributes to endothelial dysfunction and sets the stage for the development of atherosclerosis.
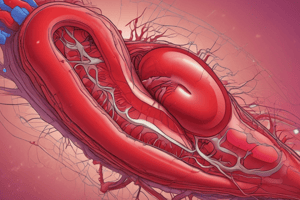
Atheroma Formation
Atheromas, or fatty plaques, are formed through the interaction of various factors, including lipids, inflammatory cells, and connective tissue. They start as low-density lipoprotein (LDL) particles, which deposit in the arterial intima due to an imbalance in the levels of LDL particles in the blood and scavenger cells responsible for removing them. Once trapped, LDL particles can become oxidized, attracting immune cells like macrophages and T-cells. Foamy macrophages, formed when large amounts of cholesterol accumulate within these cells, eventually transform into plaque-forming cells called neovascular cells. These cells produce extracellular matrix components, such as fibronectin, collagen, and glycosaminoglycans, which create a stable base for further plaque growth.
Plaque Development
As atheromas grow, they progress through distinct stages. Early plaques appear as bland, pale yellow spots on the arterial wall, while later stages exhibit a variety of features reflecting the integration of macrophages, smooth muscle cells (SMCs), and connective tissue. The plaque structure includes a thin intimal cushion covering the surface of the plaque, along with a cellular core containing inflammatory cells and lipid-rich foam cells. The plaque may also develop an extracellular matrix (ECM) rich in proteoglycans and collagen fibers, providing structural support for the growing lesion. Eventually, these changes can lead to luminal narrowing or even rupture of the arterial wall, potentially causing thrombus formation and acute clinical complications.
Inflammation in Atherosclerosis
Inflammation plays a crucial role in atherosclerosis pathology by promoting endothelial dysfunction, modulating smooth muscle cell behavior, and facilitating immune responses against invading pathogens. Chronic inflammation is characterized by increased levels of proinflammatory cytokines, chemokines, reactive oxygen species (ROS), and metalloproteases involved in vascular remodeling. These factors contribute to endothelial damage, which further exacerbates inflammatory processes and perpetuates the cycle of atherosclerotic plaque development and progression.
Complications of Atherosclerosis
Complications from atherosclerosis can include:
- Acute coronary syndrome: A sudden blockage of blood flow due to thrombosis on top of a ruptured plaque can cause chest pain, heart attack, or sudden death.
- Peripheral artery disease: Reduced blood flow to limbs due to plaque buildup in smaller vessels can lead to pain, ulcers, tissue loss, and gangrene.
- Stroke: Plaque rupture or embolization can result in blocked cerebral vessels, leading to transient ischemic attacks, stroke, or intracerebral hemorrhage.
- Carotid artery stenosis: Narrowing of the neck artery supplying blood to the brain can induce chronic hypoperfusion, transient ischemic attacks, or stroke.
- Renovascular hypertension: Atherosclerotic renal artery stenosis can lead to high blood pressure, uncontrolled hypertension, and kidney failure.
In summary, atherosclerosis results from a combination of environmental, genetic, and lifestyle factors, ultimately leading to complex pathologies involving endothelial dysfunction, atheroma formation, plaque development, inflammation, and various complications. Early detection and management of risk factors are crucial for preventing or minimizing the progression of this life-threatening condition.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.