Podcast
Questions and Answers
What structures arise from the proximal portion of the sixth aortic arch in adults?
What structures arise from the proximal portion of the sixth aortic arch in adults?
- Pulmonary veins
- Common carotid arteries
- Pulmonary arteries (correct)
- Left and right subclavian arteries
Which statement is true regarding the fifth aortic arch?
Which statement is true regarding the fifth aortic arch?
- It regresses but remains present in all embryos.
- It develops completely and contributes to vascular structures.
- It persists as a major arterial structure.
- It is absent in approximately 50% of embryos. (correct)
What part of the sixth aortic arch persists as the ductus arteriosus?
What part of the sixth aortic arch persists as the ductus arteriosus?
- Proximal portion on the left
- Proximal portion on the right
- Distal portion on the right
- Distal portion on the left (correct)
Which derivative is associated with the third aortic arch?
Which derivative is associated with the third aortic arch?
Which of the following best describes the fate of the first aortic arch?
Which of the following best describes the fate of the first aortic arch?
What does the right fourth aortic arch form in adults?
What does the right fourth aortic arch form in adults?
Which aortic arch does not have a significant contribution to adult vascular structures?
Which aortic arch does not have a significant contribution to adult vascular structures?
What vascular structure is formed from the distal part of the sixth aortic arch on the left side?
What vascular structure is formed from the distal part of the sixth aortic arch on the left side?
What is the fate of most blood entering the pulmonary trunk?
What is the fate of most blood entering the pulmonary trunk?
What happens to the ductus arteriosus shortly after birth?
What happens to the ductus arteriosus shortly after birth?
Which factor maintains the patency of the ductus arteriosus and ductus venosus in the fetus?
Which factor maintains the patency of the ductus arteriosus and ductus venosus in the fetus?
After blood enters the right atrium, where does it primarily go next?
After blood enters the right atrium, where does it primarily go next?
What percentage of blood in the descending aorta supplies the lower limbs and trunk?
What percentage of blood in the descending aorta supplies the lower limbs and trunk?
What occurs with the first inspiratory effort after birth?
What occurs with the first inspiratory effort after birth?
What percentage of blood is distributed to the placenta via the umbilical arteries?
What percentage of blood is distributed to the placenta via the umbilical arteries?
How does deoxygenated blood return to the left atrium from the lungs?
How does deoxygenated blood return to the left atrium from the lungs?
What does the umbilical vein primarily carry to the fetus?
What does the umbilical vein primarily carry to the fetus?
What is the fate of the majority of blood from the umbilical vein?
What is the fate of the majority of blood from the umbilical vein?
Which structure allows blood to flow from the right atrium to the left atrium in fetal circulation?
Which structure allows blood to flow from the right atrium to the left atrium in fetal circulation?
Which path describes how oxygenated blood is distributed from the left ventricle?
Which path describes how oxygenated blood is distributed from the left ventricle?
What happens to the blood that enters the ascending aorta from the heart?
What happens to the blood that enters the ascending aorta from the heart?
Which blood components are mixed when traveling through the left atrium?
Which blood components are mixed when traveling through the left atrium?
What primarily happens to the blood in the ductus arteriosus?
What primarily happens to the blood in the ductus arteriosus?
Which function does the porta vein serve regarding blood from the umbilical vein?
Which function does the porta vein serve regarding blood from the umbilical vein?
What happens when the ductus arteriosus remains patent?
What happens when the ductus arteriosus remains patent?
What percentage of cardiovascular malformations in infancy is attributed to the failure of the ductus arteriosus to close?
What percentage of cardiovascular malformations in infancy is attributed to the failure of the ductus arteriosus to close?
What is the condition associated with the narrowing of the aorta known as?
What is the condition associated with the narrowing of the aorta known as?
Where is the narrowing typically located in preductal coarctation?
Where is the narrowing typically located in preductal coarctation?
What collateral pathway allows blood to reach the lower part of the body once the ductus arteriosus closes?
What collateral pathway allows blood to reach the lower part of the body once the ductus arteriosus closes?
In young adults with hypertension, what should always be suspected?
In young adults with hypertension, what should always be suspected?
Which symptom is commonly associated with coarctation of the aorta in young adults?
Which symptom is commonly associated with coarctation of the aorta in young adults?
What is the typical outcome of anatomical closure of the ductus arteriosus?
What is the typical outcome of anatomical closure of the ductus arteriosus?
Which of the following best describes a consequence of pulmonary stenosis in tetralogy of Fallot?
Which of the following best describes a consequence of pulmonary stenosis in tetralogy of Fallot?
What is the role of the ventricular septal defect (VSD) in the context of tetralogy of Fallot?
What is the role of the ventricular septal defect (VSD) in the context of tetralogy of Fallot?
What characteristic is NOT associated with aortic or pulmonary stenosis?
What characteristic is NOT associated with aortic or pulmonary stenosis?
Which statement correctly explains the term 'overriding aorta' in tetralogy of Fallot?
Which statement correctly explains the term 'overriding aorta' in tetralogy of Fallot?
What physical change occurs in the heart due to aortic or pulmonary valve stenosis?
What physical change occurs in the heart due to aortic or pulmonary valve stenosis?
In the absence of significant obstruction, what typically happens to ventricular strain in cases of mild stenosis?
In the absence of significant obstruction, what typically happens to ventricular strain in cases of mild stenosis?
What ultimately happens if valvular stenosis obstruction is severe?
What ultimately happens if valvular stenosis obstruction is severe?
Which of the following correctly identifies the relationship between right ventricular hypertrophy and pulmonary stenosis?
Which of the following correctly identifies the relationship between right ventricular hypertrophy and pulmonary stenosis?
Select the correct direction of blood flow in the embryological heart tube
Select the correct direction of blood flow in the embryological heart tube
Which embryological structure gives rise to the bulk of the right ventricle?
Which embryological structure gives rise to the bulk of the right ventricle?
Which embryological structure gives rise to the bulk of the left ventricle?
Which embryological structure gives rise to the bulk of the left ventricle?
Match the following components of cardiac development with their descriptions:
Match the following components of cardiac development with their descriptions:
Match the following terms with their respective origins:
Match the following terms with their respective origins:
Match the following development stages with their outcomes:
Match the following development stages with their outcomes:
Match the following structures with their functions during heart development:
Match the following structures with their functions during heart development:
Match the following cardiovascular development processes with their results:
Match the following cardiovascular development processes with their results:
What is the fate of the truncus arteriosus in adult anatomy?
What is the fate of the truncus arteriosus in adult anatomy?
At what stage does the heart tube begin to beat somewhat ineffectively?
At what stage does the heart tube begin to beat somewhat ineffectively?
Which structure develops into the bulk of the left ventricle in embryonic development?
Which structure develops into the bulk of the left ventricle in embryonic development?
What are the layers in the heart tube initially composed of before further development?
What are the layers in the heart tube initially composed of before further development?
Which embryological regions are defined during the elongation and reshaping of the heart tube?
Which embryological regions are defined during the elongation and reshaping of the heart tube?
What is the developmental fate of the bulbis cordis?
What is the developmental fate of the bulbis cordis?
During embryonic folding, what critical structure forms the first aortic arch?
During embryonic folding, what critical structure forms the first aortic arch?
Which sequence accurately describes a sequential aspect of heart tube development?
Which sequence accurately describes a sequential aspect of heart tube development?
What is the primary function of cardiac jelly in heart development?
What is the primary function of cardiac jelly in heart development?
Which structure develops into the future epicardium of the heart wall?
Which structure develops into the future epicardium of the heart wall?
Which of the following is NOT a component of the cardiac jelly?
Which of the following is NOT a component of the cardiac jelly?
What occurs during the investment of the heart tube by the splanchnic mesoderm?
What occurs during the investment of the heart tube by the splanchnic mesoderm?
What role does the cardiac jelly play at the atrio-ventricular (A-V) junction?
What role does the cardiac jelly play at the atrio-ventricular (A-V) junction?
Around day 22, how does the heart tube physically change as it expands into the pericardial cavity?
Around day 22, how does the heart tube physically change as it expands into the pericardial cavity?
Which layer separates the myocardium from the endothelium of the heart tube?
Which layer separates the myocardium from the endothelium of the heart tube?
What process does the cardiac jelly stimulate in developing endothelial cells?
What process does the cardiac jelly stimulate in developing endothelial cells?
What is the most common type of cardiac defect associated with ventricular septal defects (VSD)?
What is the most common type of cardiac defect associated with ventricular septal defects (VSD)?
What are the two types of ventricular septal defects (VSD)?
What are the two types of ventricular septal defects (VSD)?
What leads to massive left to right shunting of blood in ventricular septal defect (VSD)?
What leads to massive left to right shunting of blood in ventricular septal defect (VSD)?
What is a common association found with defect in the formation of the membranous part of the interventricular septum?
What is a common association found with defect in the formation of the membranous part of the interventricular septum?
What effect does excessive cavitation of myocardial tissue have during the formation of the muscular interventricular septum?
What effect does excessive cavitation of myocardial tissue have during the formation of the muscular interventricular septum?
What is a persistent characteristic of foramen primum defects?
What is a persistent characteristic of foramen primum defects?
What occurs if the vessel diameters are normal in a patient with a ventricular septal defect?
What occurs if the vessel diameters are normal in a patient with a ventricular septal defect?
What specific part of the interventricular septum is affected in a membranous VSD?
What specific part of the interventricular septum is affected in a membranous VSD?
What is the primary function of the umbilical vein in fetal circulation?
What is the primary function of the umbilical vein in fetal circulation?
What happens to most of the blood that enters the inferior vena cava during fetal circulation?
What happens to most of the blood that enters the inferior vena cava during fetal circulation?
What fate does the majority of oxygenated blood have after entering the ascending aorta?
What fate does the majority of oxygenated blood have after entering the ascending aorta?
How is some of the umbilical vein blood directed to the liver?
How is some of the umbilical vein blood directed to the liver?
What type of blood primarily enters the right atrium from the inferior vena cava?
What type of blood primarily enters the right atrium from the inferior vena cava?
What characteristic defines the blood that is mixed in the left atrium during fetal circulation?
What characteristic defines the blood that is mixed in the left atrium during fetal circulation?
Which location does the ductus venosus connect in fetal circulation?
Which location does the ductus venosus connect in fetal circulation?
Which statement best describes the flow of deoxygenated blood from the upper extremities in fetal circulation?
Which statement best describes the flow of deoxygenated blood from the upper extremities in fetal circulation?
What is a significant consequence of the persistent ductus arteriosus?
What is a significant consequence of the persistent ductus arteriosus?
What is typically associated with coarctation of the aorta in terms of anatomy?
What is typically associated with coarctation of the aorta in terms of anatomy?
Which collateral pathway is commonly involved when blood reaches the lower part of the body after the ductus arteriosus closes?
Which collateral pathway is commonly involved when blood reaches the lower part of the body after the ductus arteriosus closes?
Which condition is most likely linked to premature birth and rubella?
Which condition is most likely linked to premature birth and rubella?
Which symptom is strongly correlated with coarctation of the aorta in young adults?
Which symptom is strongly correlated with coarctation of the aorta in young adults?
What primary physiological process occurs if the ductus arteriosus remains patent?
What primary physiological process occurs if the ductus arteriosus remains patent?
What characterizes the typical anatomical positioning in preductal coarctation of the aorta?
What characterizes the typical anatomical positioning in preductal coarctation of the aorta?
What percentage of cardiovascular malformations is attributed to the failure of ductus arteriosus closure?
What percentage of cardiovascular malformations is attributed to the failure of ductus arteriosus closure?
Flashcards are hidden until you start studying
Study Notes
Formation and Regression of Aortic Arches
- The fifth pair of aortic arches develops in the embryo during the end of the fourth week
- It originates from angioblasts that migrate from the surrounding splanchnic mesoderm
- The fifth pair of arches typically regresses fully and does not contribute to any vascular structure
Sixth Pair of Aortic Arches
- Sixth pair of aortic arches form around the middle of the fifth week
- Angioblasts in the surrounding splanchnic mesoderm give rise to the arches
- The proximal portion of the sixth arch forms the right and left pulmonary arteries in adults
- The distal portion of the sixth arch becomes the ductus arteriosus
Derivatives of Aortic Arches
- The first pair of aortic arches mostly disappears, but remnants contribute to forming the maxillary arteries
- The second pair of aortic arches largely disappears, with remnants giving rise to the stapedial arteries
- The third pair of aortic arches contribute to the common carotid arteries and part of the internal carotid arteries
- The left fourth aortic arch forms the arch of the aorta
- The right fourth aortic arch forms the proximal part of the right subclavian artery
- The distal part of the right subclavian artery is derived from the right dorsal aorta and the right 7th intersegmental artery
- The sixth aortic arch persists on the left as the ductus arteriosus, which later becomes the ligamentum arteriosum
- On the right, the distal part of the sixth aortic arch disappears, but the proximal portion gives rise to the right and left pulmonary arteries
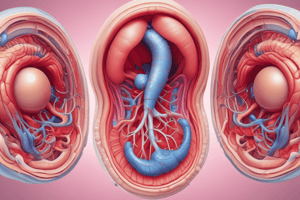
Fetal Circulation
- By the end of the seventh week, the heart has reached its final stage of development
- The umbilical vein carries highly oxygenated blood from the placenta to the fetus
- Most of the blood from the umbilical vein is shunted through the ductus venosus to the inferior vena cava
- Some blood from the umbilical vein is shunted to the portal vein to supply the liver and eventually reaches the inferior vena cava
- The inferior vena cava delivers blood to the right atrium
- Most of the blood from the inferior vena cava flows through the foramen ovale to the left atrium, mixing with a small amount of deoxygenated blood from the lungs
- This high-oxygen blood moves through the left ventricle and is pumped into the ascending aorta
- The ascending aorta distributes oxygenated blood to the heart, head, neck, and upper limbs
- The remaining oxygenated blood mixes with deoxygenated blood from the ductus arteriosus in the descending aorta
- Deoxygenated blood from the upper body via the superior vena cava enters the right atrium, mixing with a small amount of blood coming from the inferior vena cava
- This medium oxygen-content blood flows into the right ventricle and is pumped into the pulmonary trunk
- A small portion of the blood from the pulmonary trunk enters the lungs to supply lung tissues
- Deoxygenated blood from the lungs returns to the left atrium via the pulmonary veins
- Most of the blood entering the pulmonary trunk flows through the ductus arteriosus to the descending aorta
- The descending aorta delivers blood to the lower limbs, lower trunk, and placenta via the umbilical arteries
Changes in Fetal Circulation at Birth
- The first breath opens up the pulmonary vascular beds, causing blood in the pulmonary trunk to enter the lungs
- Pressure in the ductus arteriosus drops significantly, causing it to constrict within minutes after birth
- The increased blood flow from the lungs to the left atrium increases pressure in the left atrium, leading to closure of the foramen ovale
Tetralogy of Fallot
- Tetralogy of Fallot is a congenital heart defect
- It is characterized by: - Pulmonary stenosis - Ventricular septal defect of the membranous portion - Overriding aorta, which straddles the ventricular septal defect - Right ventricular hypertrophy, due to the shunting of blood from right to left
Aortic or Pulmonary Stenosis
- Aortic or pulmonary stenosis occurs when the valve is thickened and narrowed
- This leads to abnormally high pressure in the left or right ventricle, respectively
- The left or right ventricular wall thickens, known as hypertrophy
- Stenosis restricts blood flow, leading to a heart murmur
- Mild stenosis often does not cause strain on the heart, but may worsen with growth
- Severe stenosis can lead to symptoms and require treatment to open the valve
Persistent Ductus Arteriosus
- Normally, the ductus arteriosus closes functionally within a few days after birth and anatomically within a few weeks
- When the ductus arteriosus persists, blood flows from the aorta to the pulmonary artery
- Patent ductus arteriosus accounts for 10% of congenital cardiovascular malformations in infancy
- It is often associated with premature birth and rubella
Coarctation of the Aorta
- Coarctation of the aorta is a narrowing of the aorta
- The narrowing is usually proximal to the ductus arteriosus, known as preductal coarctation
- In some cases, coarctation may not be identified until early childhood
- When the ductus arteriosus closes, blood reaches the lower body through collateral pathways:
- Scapular anastomosis, connecting to intercostal arteries
- Internal thoracic arteries to the superior epigastric, inferior epigastric, and femoral arteries
- Coarctation of the aorta should be suspected in young adults with hypertension
- Patients often have reduced and delayed femoral pulses
- Coarctation of the aorta is associated with a prominent scapular artery and intercostal arteries
Development of the Heart
- The heart develops from the cardiogenic area of the embryo, which is located in the cranial region of the embryo.
- The heart begins as a pair of endocardial tubes, which form on either side of the midline.
- The endocardial tubes fuse to form the primitive heart tube.
- Developmentally the heart tube consists of 5 regions: truncus arteriosus , bulbus cordis, ventricle, atrium and sinus venosus.
- The heart tube undergoes cardiac looping, which results in the formation of the adult heart.
- During the cardiac looping process, the heart tube undergoes a series of twists and turns to form the four chambers of the heart, and the correct positioning of the chambers, valves and major vessels of the heart.
- The atrioventricular canal is the opening between the atrium and ventricle.
- The conus arteriosus is at the superior end of the ventricle.
- Cardiac jelly forms between the endocardium and myocardium.
- Cardiac jelly is a gelatinous material that acts as a scaffold for angiogenesis and myogenesis, which is the formation of blood vessels and muscles, respectively.
Development of the Conduction System
- The earliest sign of differentiation of the conduction system appears as a thickening of the myocardium in the caudal end of the heart tube, called the sinoatrial node
- Later a second thickening arises in the caudal region of the inflow tract of the ventricle forming the atrioventricular node.
- The conductive system establishes and coordinates the pattern of heart muscle contraction.
Early Circulatory System
- The early circulatory system consists of three main components:
- Vitelline veins and arteries: Provide oxygenated and nutrient rich blood from the yolk sac to the embryo.
- Umbilical veins and arteries: Provide oxygenated blood and nutrients to the embryo from the placenta and carry deoxygenated blood from the embryo back to the placenta.
- General Circulation: Provides blood flow to all parts of the embryo.
Heart Tube Remodeling
- Heart tube remodeling leads to the formation of the definitive atria.
- The sinus venosus is incorporated into the right atrium.
- The sinus venosus will form the smooth walled portion of the right atrium, the right and left horns of the sinus venosus will become the superior and inferior vena cava, respectively.
Partitioning of the Heart tube
- Partitioning of the heart tube is a complex process that results in the formation of the four chambers of the heart: the right and left atria, and the right and left ventricles.
- The process is divided into several stages:
- Partitioning of the atrioventricular canal
- Partitioning of the primitive ventricle
- Partitioning of the bulbus cordis and the truncus arteriosus
Partitioning of the Atrioventricular Canal
- The atrioventricular valves develop from endocardial cushions (epithelial tissue between the atria and ventricles).
- The atrioventricular canal is divided into right and left atrioventricular canals by the fusion of the endocardial cushions.
- The atrioventricular valves are formed from the endocardial cushions.
- The tricuspid valve will form on the right and the mitral valve will form on the left.
Partitioning of the Primitive Atrium
- The septum primum grows down from the roof of the atrium towards the endocardial cushions.
- The septum primum partitions the atrium into two chambers.
- The foramen primum is an opening in the septum primum.
- The foramen secundum develops as the septum primum fuses with the endocardial cushions.
- The septum secundum grows down from the roof of the atrium to form the foramen ovale (the opening will later be covered by a flap of tissue).
- The septum primum and septum secundum are fused to form the interatrial septum.
- The foramen ovale allows blood to bypass the lungs in the fetus, as the lungs are not fully developed.
Partitioning of the Primitive Ventricle
- The muscular interventricular septum (IVS) grows up from the floor of the ventricle towards the atrioventricular canal.
- The membranous interventricular septum forms from tissue derived from the atrioventricular endocardial cushions.
- The membranous interventricular septum closes the interventricular foramen.
- The membranous interventricular septum is a thin-walled structure.
Partitioning of the Bulbus Cordis and the Truncus Arteriosus
- Aortico-pulmonary septum is formed by the fusion of ridges that appear in the bulbus cordis and truncus arteriosus.
- The aortico-pulmonary septum is derived from neural crest cells.
- The aortico-pulmonary septum divides the bulbus cordis and truncus arteriosus into the aorta and pulmonary trunk.
- The fusion of the developing aortico-pulmonary septum with the proliferating anterior atrioventricular cushion closes the interventricular foramen and forms the membranous portion of the interventricular septum
- Cavitation of the ventricular walls leads to formation of trabeculae carneae, papillary muscles, and chordae tendineae.
- **
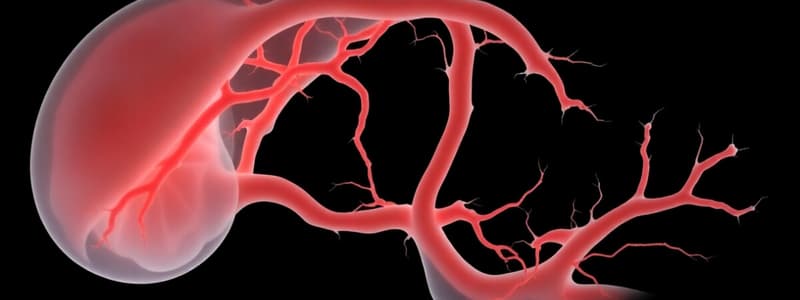
Development of Blood Vessels associated with the Heart
- Development of the veins associated with the heart occurs from the vitelline veins, umbilical veins, and cardinal veins.
- The development of the aortic arches involves the formation of six pairs of arches (first, second, third, fourth, fifth, and sixth arches).
- Aortic arches can be classified as:
- Pharyngeal arches: These are the arches that form the head and neck.
- Visceral arches: These are the branches of the aorta that bring blood to the body.
- Dorsal aorta: These are the arteries that run along the back of the embryo.
Development of Aortic Arches
- The first pair of aortic arches develops first (between day 22 and 24).
- The second pair of aortic arches appear in week 4.
- The third pair of aortic arches appear at the end of the fourth week.
- The fourth pair of aortic arches develop soon after the third pair.
- The fifth pair of aortic arches are transient and regress quickly.
- The sixth pair of aortic arches are the final pair of aortic arches.
Fate of Aortic Arches
- First pair of aortic arches: Forms the maxillary arteries.
- Second pair of aortic arches: Forms the stapedial artery and hyoid artery.
- Third pair of aortic arches: Forms the common carotid arteries and proximal portion of the internal carotid arteries.
- Fourth pair of aortic arches:
- Left side: Forms the aortic arch.
- Right side: Forms the proximal portion of the right subclavian artery.
- Fifth pair of aortic arches: Regress.
- Sixth pair of aortic arches:
- Left side: Forms the ductus arteriosus.
- Right side: Form the pulmonary artery.
Fetal Circulation
- The fetus develops a unique circulatory system that allows for nutrient and oxygen transfer from the placenta.
- The fetus receives oxygenated blood from the placenta through the umbilical vein.
- Oxygen-rich blood bypasses the lungs through the foramen ovale, entering the left atrium.
- Blood from the right ventricle is pumped through the pulmonary trunk, into the aorta, and into the systemic circulation.
- Some deoxygenated blood from the left ventricle is pumped through the ductus arteriosus and into the descending aorta.
- The ductus arteriosus bypasses the lungs.
- Most of the deoxygenated blood flows from the inferior vena cava, through the right atrium, through the foramen ovale, and into the left atrium.
Changes in Fetal Circulation at Birth
- The first breath initiates a cascade of changes in the heart, lungs, and circulation.
- The lungs expand, leading to increased pulmonary blood flow.
- Increased pulmonary blood flow leads to an increase in pressure in the left atrium.
- The increased pressure in the left atrium closes the foramen ovale.
- The clamping of the umbilical cord stops the blood flow from the placenta, and blood flow through the ductus arteriosus decreases.
- The ductus arteriosus usually closes within a few days after birth.
Congenital Defects of the Heart and Major Vessels
- Congenital heart defects are structural abnormalities of the heart that are present at birth.
- Congenital heart defects can range from mild to severe, and can be divided into congenital defects involving the atria, ventricles, aorta, and pulmonary trunk
- The vulnerable period for cardiovascular development and anomalies is between weeks 3 and 8 of pregnancy.
- Cardiac development and anomalies can be prevented by maintaining a healthy lifestyle and taking prenatal vitamins.
- The risk of congenital heart defects increases with maternal age.
Atrial Septal Defects
- Atrial septal defects (ASD) are defects in the interatrial septum.
- ASD allows blood to flow from the left atrium to the right atrium.
- Two common types of ASD:
- Secundum ASD: These defects occur in the septum secundum of the interatrial septum, near the foramen ovale.
- Endocardial cushion defect with primum ASD: Occur in the septum primum and endocardial cushions of the interatrial septum.
- ASD is classified as a shunt and may range in severity from severe to minor.
Ventricular Septal Defects
- Ventricular septal defects (VSD) are defects in the interventricular septum.
- VSDs are one of the most common types of congenital heart defects.
- VSDs allow blood to flow from the left ventricle to the right ventricle.
- VSDs are classified by their location and size.
- The majority of VSDs close spontaneously before the age of 1 year.
- Some VSDs, however, require surgical closure.
Persistent Truncus Arteriosus
- Persistent Truncus Arteriosus arises when the aorticopulmonary septum fails to develop.
- The aorta and pulmonary trunk fuse, resulting in one large artery arising from the heart.
- The heart receives oxygenated and deoxygenated blood through the single large trunk.
Transposition of the Great Vessels
- Transposition of the Great Vessels is a congenital heart defect that is characterized by the aorta arising from the right ventricle, and the pulmonary trunk arising from the left ventricle.
- Blood flow is interrupted, and the heart is unable to effectively pump blood to the lungs and body.
Tetralogy of Fallot
- Tetralogy of Fallot is a congenital heart defect that involves four separate defects:
- A ventricular septal defect.
- Pulmonary stenosis, a narrowing of the valve between the right ventricle and the pulmonary trunk.
- Overriding aorta, a large aorta arising from the right ventricle.
- Right ventricular hypertrophy, an increased thickness of the right ventricular wall.
- Tetralogy of Fallot is characterized by a shortage of oxygen.
Aortic or Pulmonary Stenosis
- Aortic stenosis is a congenital heart defect that results in narrowing of the aortic valve, which causes obstructed blood flow to the body.
- Pulmonary stenosis is a congenital heart defect that results in narrowing of the pulmonary valve, which causes obstructed blood flow to the lungs.
Persistent Ductus Arteriosus
- Persistent ductus arteriosus arises when the ductus arteriosus fails to close after birth.
- Blood flows from the aorta to the pulmonary artery, increasing the workload of the right ventricle.
- The ductus arteriosus typically closes within a few days after birth.
Coarctation of the Aorta
- Coarctation of the aorta is a congenital heart defect that results in narrowing of the aorta, which typically occurs near the ductus arteriosus.
- The narrowing can block blood flow to the body and may remain unidentified until early childhood.
Dextrocardia
- Dextrocardia is a congenital heart defect characterized by the location of the heart on the right side of the chest.
- Dextrocardia is usually associated with situs inversus, a condition where the internal organs are reversed in their position.
- Dextrocardia is typically found in children.
Embryonic Heart Development
- The heart tube forms by the end of the third week of embryologic development.
- The heart tube bulges into the pericardial cavity by day 21.
- The heart tube elongates and develops different regions around day 21, such as the truncus arteriosus, bulbis cordis, primitive ventricle, and primitive atria.
- The heart tube consists of three layers: endocardium, myocardium, and epicardium.
- Cardiac jelly is an acellular matrix between the myocardium and endocardium, playing a critical role in cardiac septation and valve formation.
- The heart tube attaches to the dorsal wall of the pericardial cavity.
Fetal Circulation
- The umbilical vein carries highly oxygenated blood from the placenta to the fetus.
- Most of the blood from the umbilical vein is shunted through the ductus venosus to the inferior vena cava.
- The inferior vena cava delivers blood to the right atrium.
- Most of the blood from the inferior vena cava passes through the foramen ovale to the left atrium.
- This highly oxygenated blood is pumped from the left ventricle to the ascending aorta.
- Most of the oxygenated blood from the ascending aorta is distributed to the heart, head, and neck.
- The remaining blood mixes with deoxygenated blood from the ductus arteriosus, continuing to the descending aorta.
Common Cardiovascular Defects
- Atrial Septal Defects (ASD) - A common cardiac defect where a hole remains between the left and right atria, causing a left-to-right shunt of blood.
- Ventricular Septal Defects (VSD) - The most common type of cardiac defect (25% of all cardiac defects), causing a left-to-right shunting of blood. Two main types: membranous VSD and muscular VSD.
- Persistent Ductus Arteriosus (PDA) - Occurs when the ductus arteriosus, a connection between the aorta and pulmonary artery, fails to close after birth, leading to blood shunting from the aorta to the pulmonary artery.
- Coarctation of the Aorta - A narrowing of the aorta, usually located proximal to the ductus arteriosus, often leading to high blood pressure and delayed femoral pulses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.