Podcast
Questions and Answers
What component is primarily found in fungal cell walls, distinguishing them from bacteria?
What component is primarily found in fungal cell walls, distinguishing them from bacteria?
- Cellulose
- Peptidoglycan
- Chitin (correct)
- Ergosterol
Which of the following is a common characteristic that differentiates fungal cell membranes from mammalian cell membranes?
Which of the following is a common characteristic that differentiates fungal cell membranes from mammalian cell membranes?
- Absence of sterols
- Presence of cholesterol
- Presence of peptidoglycan
- Presence of ergosterol (correct)
What term describes a fungal infection?
What term describes a fungal infection?
- Parasitosis
- Viremia
- Bacteremia
- Mycosis (correct)
Which type of fungal infection affects the skin, hair, and nails?
Which type of fungal infection affects the skin, hair, and nails?
Which of the following infections is commonly caused by yeasts?
Which of the following infections is commonly caused by yeasts?
Which of the following defines a systemic mycosis?
Which of the following defines a systemic mycosis?
Which antifungal drug is derived from Streptomyces nodosus?
Which antifungal drug is derived from Streptomyces nodosus?
Which component of the fungal cell membrane does Amphotericin B bind to?
Which component of the fungal cell membrane does Amphotericin B bind to?
What is the primary mechanism of action of amphotericin B?
What is the primary mechanism of action of amphotericin B?
What is a common mechanism of resistance to Amphotericin B?
What is a common mechanism of resistance to Amphotericin B?
Which of the following is a common adverse effect associated with amphotericin B administration?
Which of the following is a common adverse effect associated with amphotericin B administration?
Which enzyme, absent in mammalian cells, allows 5-FC to enter fungal cells?
Which enzyme, absent in mammalian cells, allows 5-FC to enter fungal cells?
What is the mechanism of action of flucytosine (5-FC) once it enters the fungal cell?
What is the mechanism of action of flucytosine (5-FC) once it enters the fungal cell?
Why is flucytosine typically used in combination with other antifungal agents?
Why is flucytosine typically used in combination with other antifungal agents?
Which of the following is a common adverse effect of flucytosine (5-FC)?
Which of the following is a common adverse effect of flucytosine (5-FC)?
What is the primary mechanism of action of azole antifungals?
What is the primary mechanism of action of azole antifungals?
What is a common mechanism of resistance to azole antifungals?
What is a common mechanism of resistance to azole antifungals?
Why are azole antifungals generally avoided during pregnancy?
Why are azole antifungals generally avoided during pregnancy?
Which of the following is a key limitation of fluconazole's antifungal spectrum?
Which of the following is a key limitation of fluconazole's antifungal spectrum?
Which azole antifungal requires administration with food and an acidic beverage for enhanced absorption?
Which azole antifungal requires administration with food and an acidic beverage for enhanced absorption?
Which azole antifungal is contraindicated in patients with ventricular dysfunction or heart failure?
Which azole antifungal is contraindicated in patients with ventricular dysfunction or heart failure?
How is posaconazole primarily eliminated from the body?
How is posaconazole primarily eliminated from the body?
Which of the following is a notable side effect associated with high concentrations of voriconazole?
Which of the following is a notable side effect associated with high concentrations of voriconazole?
Which of the following Echinocandins does NOT require a loading dose?
Which of the following Echinocandins does NOT require a loading dose?
What is the mechanism of action of echinocandins?
What is the mechanism of action of echinocandins?
Which of the following describes the term "ringworm"?
Which of the following describes the term "ringworm"?
What is the mechanism of action of squalene epoxidase inhibitors?
What is the mechanism of action of squalene epoxidase inhibitors?
Which of the following is the preferred treatment for dermatophyte onychomycoses (nail fungal infections)?
Which of the following is the preferred treatment for dermatophyte onychomycoses (nail fungal infections)?
Which topical antifungal is effective against Trichophyton, Microsporum, and Epidermophyton?
Which topical antifungal is effective against Trichophyton, Microsporum, and Epidermophyton?
What is the mechanism of action of griseofulvin?
What is the mechanism of action of griseofulvin?
Why is nystatin not administered parenterally?
Why is nystatin not administered parenterally?
Which of the following describes the spectrum of activity of imidazoles when used topically?
Which of the following describes the spectrum of activity of imidazoles when used topically?
Which process does ciclopirox disrupt in fungal cells?
Which process does ciclopirox disrupt in fungal cells?
What is the mechanism of action of tavaborole?
What is the mechanism of action of tavaborole?
Which fungi are specifically targeted by tolnaftate?
Which fungi are specifically targeted by tolnaftate?
A patient is prescribed itraconazole capsules for a fungal infection. What instructions should the healthcare provider give regarding administration to maximize absorption?
A patient is prescribed itraconazole capsules for a fungal infection. What instructions should the healthcare provider give regarding administration to maximize absorption?
A patient with a history of liver dysfunction is prescribed an antifungal medication. Which of the following antifungals requires the most careful monitoring of liver function due to its significant hepatic metabolism and potential for hepatotoxicity?
A patient with a history of liver dysfunction is prescribed an antifungal medication. Which of the following antifungals requires the most careful monitoring of liver function due to its significant hepatic metabolism and potential for hepatotoxicity?
A patient is diagnosed with invasive aspergillosis and has a known hypersensitivity to amphotericin B. Considering the guidelines, which of the following would be the MOST appropriate alternative first-line treatment?
A patient is diagnosed with invasive aspergillosis and has a known hypersensitivity to amphotericin B. Considering the guidelines, which of the following would be the MOST appropriate alternative first-line treatment?
A researcher is investigating a novel antifungal compound. In preclinical studies, they observe that the compound inhibits fungal cell growth but also significantly interferes with cholesterol synthesis in mammalian cells. Based on this information, which of the following mechanisms of action is MOST likely for this compound?
A researcher is investigating a novel antifungal compound. In preclinical studies, they observe that the compound inhibits fungal cell growth but also significantly interferes with cholesterol synthesis in mammalian cells. Based on this information, which of the following mechanisms of action is MOST likely for this compound?
A patient is receiving posaconazole for prophylaxis against invasive fungal infections during chemotherapy. They are also taking citalopram for depression. What is the most important consideration regarding this drug combination?
A patient is receiving posaconazole for prophylaxis against invasive fungal infections during chemotherapy. They are also taking citalopram for depression. What is the most important consideration regarding this drug combination?
What cellular component do fungi possess that is absent in bacteria?
What cellular component do fungi possess that is absent in bacteria?
Which characteristic of the fungal cell membrane makes it a target for antifungal drugs, while minimizing harm to human cells?
Which characteristic of the fungal cell membrane makes it a target for antifungal drugs, while minimizing harm to human cells?
Which of the following is NOT typically associated with systemic mycoses?
Which of the following is NOT typically associated with systemic mycoses?
Which of the following is the primary mechanism of action of amphotericin B?
Which of the following is the primary mechanism of action of amphotericin B?
What mechanism underlies fungal resistance to amphotericin B?
What mechanism underlies fungal resistance to amphotericin B?
Why is flucytosine (5-FC) often used in combination with amphotericin B?
Why is flucytosine (5-FC) often used in combination with amphotericin B?
How do azole antifungals disrupt fungal cell growth?
How do azole antifungals disrupt fungal cell growth?
What is the mechanism by which fungi typically develop resistance to azole antifungals?
What is the mechanism by which fungi typically develop resistance to azole antifungals?
Why are azole antifungals generally contraindicated during pregnancy?
Why are azole antifungals generally contraindicated during pregnancy?
Which of the following best explains why posaconazole's oral bioavailability is affected by gastric pH?
Which of the following best explains why posaconazole's oral bioavailability is affected by gastric pH?
Which aspect of voriconazole's metabolism is most clinically relevant when considering drug interactions?
Which aspect of voriconazole's metabolism is most clinically relevant when considering drug interactions?
Echinocandins are particularly effective against which types of fungi due to their mechanism of action?
Echinocandins are particularly effective against which types of fungi due to their mechanism of action?
How does terbinafine exert its antifungal effect?
How does terbinafine exert its antifungal effect?
Why is griseofulvin contraindicated in patients with porphyria?
Why is griseofulvin contraindicated in patients with porphyria?
If a novel antifungal is discovered that inhibits ALL aminoacyl-tRNA synthetases, what is the MOST likely reason it would be unsuitable for clinical use?
If a novel antifungal is discovered that inhibits ALL aminoacyl-tRNA synthetases, what is the MOST likely reason it would be unsuitable for clinical use?
Flashcards
Mucocutaneous Infections
Mucocutaneous Infections
Fungal infections, generally resistant to antibiotics, affecting skin, hair, and nails.
Systemic Mycoses
Systemic Mycoses
Fungal infections that affect internal organs, often in immune-compromised individuals.
Amphotericin B
Amphotericin B
Binds to ergosterol in fungal membranes, creating pores and causing cell death; used for life-threatening mycoses.
Amphotericin B Resistance
Amphotericin B Resistance
Signup and view all the flashcards
Flucytosine (5-FC)
Flucytosine (5-FC)
Signup and view all the flashcards
Azole Antifungals
Azole Antifungals
Signup and view all the flashcards
Azole Resistance
Azole Resistance
Signup and view all the flashcards
Fluconazole
Fluconazole
Signup and view all the flashcards
Itraconazole
Itraconazole
Signup and view all the flashcards
Posaconazole
Posaconazole
Signup and view all the flashcards
Voriconazole
Voriconazole
Signup and view all the flashcards
Echinocandins
Echinocandins
Signup and view all the flashcards
Terbinafine
Terbinafine
Signup and view all the flashcards
Griseofulvin
Griseofulvin
Signup and view all the flashcards
Nystatin
Nystatin
Signup and view all the flashcards
Squalene epoxidase inhibitors
Squalene epoxidase inhibitors
Signup and view all the flashcards
Study Notes
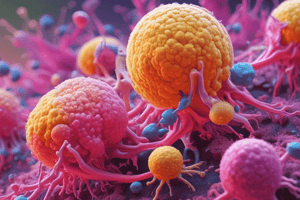
- Fungi are eukaryotic organisms with cell walls containing chitin, and their cell membranes include ergosterol.
- Fungal infections are termed mycoses.
Types of Fungal Infections
- Mucocutaneous infections affect skin, hair, and nails (dermatophytes) or moist skin and mucous membranes (yeasts).
- Systemic mycoses are fungal infections affecting internal organs, often in immunocompromised patients.
Classification of Antifungal Drugs
- Antifungals are grouped based on their mechanism of action.
- Polyenes like amphotericin B bind to ergosterol, disrupting the fungal membrane.
- Azoles inhibit ergosterol synthesis in the fungal cell's endoplasmic reticulum.
- Flucytosine converts to 5-fluorouracil, inhibiting DNA synthesis within the fungal cell.
Drugs for Subcutaneous and Systemic Mycotic Infections
Amphotericin B
- Amphotericin B is a polyene antifungal derived from Streptomyces nodosus, used for life-threatening mycoses.
- It binds to ergosterol, forming pores in the fungal cell membrane, leading to leakage and cell death.
- Exhibits both fungicidal and fungistatic properties against a wide range of fungi and is also used in treating leishmaniasis.
- Resistance develops via reduced ergosterol content in the fungal membrane.
- Administered via slow IV infusion due to its insolubility in water, requiring co-formulation.
- Exhibits extensive plasma protein binding, broad distribution, and primary excretion in urine.
- Adverse effects may include fever, chills, renal impairment, hypotension, hypokalemia, and thrombophlebitis.
Antimetabolite Antifungals
- Flucytosine (5-FC) is a synthetic pyrimidine antimetabolite, often combined with other antifungals.
- Enters fungal cells via cytosine-specific permease, converting to compounds like 5-fluorouracil (5-FU) that disrupt nucleic acid and protein synthesis.
- Fungistatic and effective with itraconazole for chromoblastomycosis, or with amphotericin B for systemic mycoses and meningitis caused by C. neoformans and C. albicans.
- Resistance is linked to decreased enzyme levels in the conversion of flucytosine to active metabolites.
- Combining with another antifungal agent lowers the emergence of resistant fungal cells, emphasizing that it is not employed as a standalone antifungal drug.
- Well-absorbed orally and widely distributed with good CSF penetration.
- Both the parent drug and its metabolites are excreted through glomerular filtration, necessitating dose adjustments in individuals with impaired renal function.
- Adverse effects include reversible neutropenia, thrombocytopenia, bone marrow depression, hepatic dysfunction, nausea, vomiting, and diarrhea.
Azole Antifungals
- Azoles include imidazoles (typically topical) and triazoles (systemic).
- Triazoles: fluconazole, itraconazole, posaconazole, voriconazole, and isavuconazole.
- Mechanism of action: Fungistatic agents inhibiting 14-α-demethylase, disrupting ergosterol biosynthesis and compromising fungal membrane structure/function.
- Resistance can occur through mutations in the 14-α-demethylase gene, efflux pumps, or reduced ergosterol.
- Azoles are teratogenic and that they should be avoided in pregnancy.
Fluconazole
- Fluconazole is a triazole antifungal with activity against yeasts and certain dimorphic fungi.
- Ineffective against aspergillosis or mucormycosis but highly effective against C. neoformans and specific Candida species.
- Used in bone marrow transplant recipients for fungal infection prevention.
- The preferred treatment for C. neoformans after initial therapy with amphotericin B and flucytosine.
- Also used for candidemia, coccidioidomycosis, and mucocutaneous candidiasis.
- For vulvovaginal candidiasis, it is commonly administered as a single oral dose.
- Available in oral and IV formulations, well-absorbed, widely distributed, and primarily excreted in urine.
- Doses must be reduced in patients with renal dysfunction.
- Adverse effects include nausea, vomiting, headache, and skin rashes.
Itraconazole
- Itraconazole is a synthetic triazole with a broad antifungal spectrum.
- Preferred treatment for blastomycosis, sporotrichosis, paracoccidioidomycosis, and histoplasmosis.
- The capsule is best taken with food and an acidic beverage for enhanced absorption, while the solution is more effective on an empty stomach.
- Distributes well in tissues including bone and adipose tissues.
- Extensively metabolized by the liver.
- Both the drug and its inactive metabolites are excreted in urine and feces.
- Itraconazole is a potent inhibitor of CYP3A4 and coadministration of other agents metabolized by CYP3A4 should be avoided, if possible.
- Adverse effects include nausea, vomiting, diarrhea, rash, hypokalemia, hypertension, edema, and headache.
- Liver toxicity is a concern, particularly with other hepatotoxic drugs.
- Exhibits a negative inotropic effect, making it unsuitable for patients with ventricular dysfunction or heart failure.
Posaconazole
- Posaconazole is a synthetic triazole similar to itraconazole, available in oral suspension, tablet, and IV forms.
- Used for treating and preventing invasive Candida and Aspergillus infections.
- Effective against infections caused by Scedosporium and Mucorales.
- Has low oral bioavailability and requires administration with food.
- Not metabolized by CYP450 but is eliminated via glucuronidation.
- Drugs that increase gastric pH may decrease the absorption of oral posaconazole and should be avoided.
- Concomitant use of posaconazole with various agents is contraindicated due to posaconazole's potent inhibition of CYP450 3A4.
Voriconazole
- Voriconazole is a synthetic triazole related to fluconazole, available in IV and oral forms.
- Has replaced amphotericin B as the preferred treatment for invasive aspergillosis.
- Approved for invasive candidiasis and serious infections caused by Scedosporium and Fusarium species.
- Exhibits high oral bioavailability, effective tissue penetration, and extensive metabolism by CYP2C19, CYP2C9, and CYP3A4 isoenzymes.
- High concentrations may cause visual and auditory hallucinations, increased risk of hepatotoxicity and hypokalemia, and reversible visual impairment upon discontinuation.
- Contraindicated with many drugs that are inducers of CYP450.
Isavuconazole
- Isavuconazole is a broad-spectrum antifungal agent available in intravenous and oral forms, supplied as the prodrug isavuconazonium.
- Effective against invasive aspergillosis and invasive mucormycosis, similar to voriconazole.
- Exhibits high bioavailability orally and distributes well into tissues.
- Metabolism involves CYP3A4, CYP3A5, and uridine-diphosphate-glucuronosyltransferases.
- Coadministration with potent CYP3A4 inhibitors and inducers is contraindicated due to drug interactions.
- Inhibits the CYP3A4 isoenzyme, leading to increased concentrations of drugs that are substrates of CYP3A4.
- Common side effects include nausea, vomiting, diarrhea, and hypokalemia.
Echinocandins
- Echinocandins (caspofungin, micafungin, and anidulafungin) disrupt fungal cell wall synthesis by inhibiting β(1,3)-d-glucan synthesis.
- Administered intravenously once daily.
- Effective against Aspergillus and various Candida species, including azole-resistant strains.
- Micafungin stands out for not requiring a loading dose.
- Adverse effects include fever, rash, nausea, and phlebitis.
- Slow IV infusion is recommended to prevent histamine-like reactions.
- Caspofungin is a first-line treatment for invasive candidiasis and a second-line option for invasive aspergillosis.
- Dosing adjustments are necessary for moderate hepatic dysfunction.
- Concurrent use with cyclosporine is discouraged due to a high risk of elevated hepatic transaminases.
- Micafungin and anidulafungin are recommended as first-line treatments for invasive candidiasis.
- Micafungin also serves for prophylaxis against invasive Candida infections.
- Notably, both drugs are not substrates for CYP450 enzymes and do not pose any associated drug interactions.
Drugs for Cutaneous Mycotic Infections
- Cutaneous infections, caused by mold-like fungi, are known as dermatophytes or tinea.
- Classified by the affected site and commonly referred to as "ringworm".
- Primary fungi: Trichophyton, Microsporum, and Epidermophyton.
- Skin infections can also be caused by yeasts like Malassezia and Candida.
Squalene Epoxidase Inhibitors
- These agents inhibit squalene epoxidase, blocking ergosterol biosynthesis.
- Accumulation of toxic amounts of squalene results in increased membrane permeability and death of the fungal cell.
- Oral terbinafine is preferred for dermatophyte onychomycoses, also applicable for tinea capitis.
- Topical terbinafine treats tinea pedis, tinea corporis, tinea cruris, and tinea versicolor.
- Effective against Trichophyton and Malassezia. While it may potentially work against Candida, Epidermophyton, and Scopulariopsis.
- 40% bioavailability orally due to first-pass metabolism.
- Highly protein-bound and accumulates in the skin, nails, and adipose tissue, leading to a prolonged half-life of 200 to 400 hours.
- Metabolized by various CYP450 isoenzymes.
- Excreted through urine.
- Should be avoided in patients with significant renal or hepatic impairment.
- Inhibits CYP2D6 isoenzyme, posing a risk of adverse effects when used concurrently with CYP2D6 substrates.
- Oral formulation adverse effects include diarrhea, dyspepsia, nausea, headache, and rash. Taste and visual disturbances may also occur, along with elevated levels of serum hepatic transaminases.
- Topical formulations are generally well tolerated.
- Naftifine: Effective against Trichophyton, Microsporum, and Epidermophyton, used topically for tinea infections.
- Butenafine: Effective against Trichophyton rubrum, Epidermophyton, and Malassezia, used topically for tinea infections.
Griseofulvin
- Griseofulvin disrupts the mitotic spindle and inhibits fungal mitosis, effective for dermatophytosis of the scalp and hair.
- Largely replaced by oral terbinafine for onychomycosis treatment.
- Fungistatic, requiring prolonged treatment.
- Absorbed well with high-fat meals, concentrating in skin, hair, nails, and adipose tissue.
- Induces hepatic CYP450 activity, impacting drug metabolism.
- Contraindicated in pregnancy and porphyria patients.
Nystatin
- Nystatin is a polyene antifungal similar to amphotericin B.
- Used for treating cutaneous and oral Candida infections.
- Not administered parenterally due to minimal absorption and potential systemic toxicity.
- Given orally, intravaginally, or topically.
Imidazoles
- Imidazoles include butoconazole, clotrimazole, econazole, ketoconazole, miconazole, oxiconazole, sertaconazole, sulconazole, terconazole, and tioconazole.
- These topical agents have broad activity against Epidermophyton, Microsporum, Trichophyton, Candida, and Malassezia.
- Used for treating tinea infections, oropharyngeal, and vulvovaginal candidiasis.
- Topical use may lead to contact dermatitis, vulvar irritation, and edema.
- Clotrimazole and miconazole are available in troche and buccal tablet forms for treating thrush.
- Topical ketoconazole is effective against tinea versicolor and seborrheic dermatitis.
Efinaconazole
- Efinaconazole is a topical triazole antifungal agent designed for treating toenail onychomycosis.
Ciclopirox
- Ciclopirox, a pyridine antimycotic, disrupts the synthesis of DNA, RNA, and proteins by inhibiting the transport of essential elements.
- Exhibits activity against various fungi.
- Comes in multiple formulations, such as shampoo for seborrheic dermatitis, and cream, gel, or suspension for conditions like tinea pedis, tinea corporis, tinea cruris, cutaneous candidiasis, and tinea versicolor.
- Onychomycosis can be addressed with the nail lacquer formulation of ciclopirox.
Tavaborole
- Tavaborole is a topical solution used to treat toenail onychomycosis by inhibiting an aminoacyl-transfer ribonucleic acid synthetase.
Tolnaftate
- Tolnaftate, a topical thiocarbamate, disrupts hyphae and inhibits mycelial growth in susceptible fungi.
- Specifically targets Epidermophyton, Microsporum, and Malassezia furfur, and is not effective against Candida.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.