Podcast
Questions and Answers
What happens if RAAS is blocked in a patient with severe renal impairment (S.creatinine > 3 mg/dl)?
What happens if RAAS is blocked in a patient with severe renal impairment (S.creatinine > 3 mg/dl)?
- It will improve renal function.
- It will aggravate renal failure. (correct)
- It will stabilize blood pressure.
- It will have no effect on renal function.
Which of the following ACE inhibitors contains a sulfhydryl (SH) group?
Which of the following ACE inhibitors contains a sulfhydryl (SH) group?
- Fosinopril
- Lisinopril
- Captopril (correct)
- Benazepril
Which ACE inhibitor is a prodrug and requires metabolic activation?
Which ACE inhibitor is a prodrug and requires metabolic activation?
- Lisinopril
- Captopril
- Enalapril (correct)
- Benazepril
What is the mechanism of action of ACE inhibitors regarding bradykinin?
What is the mechanism of action of ACE inhibitors regarding bradykinin?
How frequently should Captopril be administered to achieve therapeutic efficacy?
How frequently should Captopril be administered to achieve therapeutic efficacy?
Which of the following is an effect of inhibition of the RAAS?
Which of the following is an effect of inhibition of the RAAS?
What distinguishes Aliskiren from other RAAS inhibitors?
What distinguishes Aliskiren from other RAAS inhibitors?
Which ACE inhibitor does not undergo significant metabolism by the liver?
Which ACE inhibitor does not undergo significant metabolism by the liver?
What physiological condition triggers the release of renin from the juxtaglomerular cells?
What physiological condition triggers the release of renin from the juxtaglomerular cells?
Which receptor does Angiotensin II primarily act on to maintain GFR despite decreased RBF?
Which receptor does Angiotensin II primarily act on to maintain GFR despite decreased RBF?
What is a consequence of Angiotensin II acting on AT1 receptors outside the kidneys?
What is a consequence of Angiotensin II acting on AT1 receptors outside the kidneys?
In the context of renal ischemia, which of the following is a potential outcome if RAAS is activated?
In the context of renal ischemia, which of the following is a potential outcome if RAAS is activated?
How does the RAAS system contribute to maintaining renal function in states of low renal blood flow?
How does the RAAS system contribute to maintaining renal function in states of low renal blood flow?
What changes in kidney function can lead to acute oliguria?
What changes in kidney function can lead to acute oliguria?
What role does Angiotensin II play in the kidneys during low renal perfusion states?
What role does Angiotensin II play in the kidneys during low renal perfusion states?
What effect does persistent activation of the RAAS have on renal tissues?
What effect does persistent activation of the RAAS have on renal tissues?
Renin is released from the juxtaglomerular cells in response to increased renal blood flow.
Renin is released from the juxtaglomerular cells in response to increased renal blood flow.
Angiotensin II has no effect on the efferent arterioles of the kidney.
Angiotensin II has no effect on the efferent arterioles of the kidney.
The activation of the RAAS can lead to systemic vasodilation in various tissues.
The activation of the RAAS can lead to systemic vasodilation in various tissues.
Acute tubular necrosis may develop as a result of renal ischemia.
Acute tubular necrosis may develop as a result of renal ischemia.
Angiotensin II contributes to cellular hypertrophy and apoptosis in some tissues.
Angiotensin II contributes to cellular hypertrophy and apoptosis in some tissues.
The RAAS system helps to increase renal blood flow when there is a decrease in blood volume.
The RAAS system helps to increase renal blood flow when there is a decrease in blood volume.
A decrease in renal blood flow and glomerular filtration rate directly triggers the release of aldosterone.
A decrease in renal blood flow and glomerular filtration rate directly triggers the release of aldosterone.
Vasoconstriction of the efferent arterioles helps maintain adequate GFR even with low renal blood flow.
Vasoconstriction of the efferent arterioles helps maintain adequate GFR even with low renal blood flow.
Inhibitors of the RAAS can potentially improve renal function in cases of severe renal impairment.
Inhibitors of the RAAS can potentially improve renal function in cases of severe renal impairment.
Captopril is a prodrug that requires liver metabolism to become active.
Captopril is a prodrug that requires liver metabolism to become active.
Bradykinin is degraded by Angiotensin-converting enzyme (ACE).
Bradykinin is degraded by Angiotensin-converting enzyme (ACE).
All ACE inhibitors listed are classified as prodrugs.
All ACE inhibitors listed are classified as prodrugs.
Blocking Angiotensin II formation will lead to decreased vascular constriction and reduced salt and water retention.
Blocking Angiotensin II formation will lead to decreased vascular constriction and reduced salt and water retention.
ACE inhibitors that contain a sulfhydryl (SH) group have a higher likelihood of causing immune side effects.
ACE inhibitors that contain a sulfhydryl (SH) group have a higher likelihood of causing immune side effects.
Angiotensin-converting enzyme inhibitors must be administered every 8 hours to achieve therapeutic efficacy.
Angiotensin-converting enzyme inhibitors must be administered every 8 hours to achieve therapeutic efficacy.
Lisinopril requires renal metabolism and is not effective in patients with kidney impairment.
Lisinopril requires renal metabolism and is not effective in patients with kidney impairment.
What initiates the release of renin from juxtaglomerular cells?
What initiates the release of renin from juxtaglomerular cells?
How does Angiotensin II help maintain GFR despite decreased RBF?
How does Angiotensin II help maintain GFR despite decreased RBF?
Describe the systemic effects of Angiotensin II upon activation of AT1 receptors.
Describe the systemic effects of Angiotensin II upon activation of AT1 receptors.
What condition can result from acute oliguria induced by renal ischemia?
What condition can result from acute oliguria induced by renal ischemia?
Explain the consequence of sustained RAAS activation on renal tissues.
Explain the consequence of sustained RAAS activation on renal tissues.
What is the relationship between renal blood flow and glomerular filtration rate?
What is the relationship between renal blood flow and glomerular filtration rate?
What triggers the compensatory mechanisms of the RAAS in response to decreased kidney perfusion?
What triggers the compensatory mechanisms of the RAAS in response to decreased kidney perfusion?
Identify the negative effects of Angiotensin II on tissues outside the kidneys.
Identify the negative effects of Angiotensin II on tissues outside the kidneys.
What is the primary risk of blocking RAAS in patients with severe renal impairment (S.creatinine > 3 mg/dl)?
What is the primary risk of blocking RAAS in patients with severe renal impairment (S.creatinine > 3 mg/dl)?
How do ACE inhibitors affect bradykinin levels in the body?
How do ACE inhibitors affect bradykinin levels in the body?
Which class of drug includes β-blockers, α-methyldopa, and clonidine in relation to RAAS inhibition?
Which class of drug includes β-blockers, α-methyldopa, and clonidine in relation to RAAS inhibition?
Identify a key pharmacological property that differentiates captopril from other ACE inhibitors.
Identify a key pharmacological property that differentiates captopril from other ACE inhibitors.
Which ACE inhibitors listed are classified as prodrugs?
Which ACE inhibitors listed are classified as prodrugs?
What is the role of angiotensin II in relation to glomerular filtration rate (GFR)?
What is the role of angiotensin II in relation to glomerular filtration rate (GFR)?
Describe the impact of ACE inhibitors on aldosterone release.
Describe the impact of ACE inhibitors on aldosterone release.
What is the significance of using an ACE inhibitor like lisinopril in patients with mild renal impairment (S.creatinine up to 3 mg/dl)?
What is the significance of using an ACE inhibitor like lisinopril in patients with mild renal impairment (S.creatinine up to 3 mg/dl)?
The renin-angiotensin-aldosterone (RAAS) system is activated in response to ↓ RBF and ↓ GFR due to renal ______.
The renin-angiotensin-aldosterone (RAAS) system is activated in response to ↓ RBF and ↓ GFR due to renal ______.
Renin is released from the juxtaglomerular cells as a rescue message to initiate stimulation of the ______ system.
Renin is released from the juxtaglomerular cells as a rescue message to initiate stimulation of the ______ system.
Angiotensin II acts on AT1 receptors causing ______ of the efferent arterioles to maintain GFR.
Angiotensin II acts on AT1 receptors causing ______ of the efferent arterioles to maintain GFR.
Activation of AT1 receptors outside the kidneys causes systemic ______, hypertrophy, and apoptosis.
Activation of AT1 receptors outside the kidneys causes systemic ______, hypertrophy, and apoptosis.
Chronic activation of the RAAS can lead to ______ renal tissues and may induce degenerative changes.
Chronic activation of the RAAS can lead to ______ renal tissues and may induce degenerative changes.
Acute oliguria may develop due to renal ______ resulting from activation of the RAAS.
Acute oliguria may develop due to renal ______ resulting from activation of the RAAS.
Angiotensin II plays a role in maintaining adequate GFR despite decreases in renal ______ flow.
Angiotensin II plays a role in maintaining adequate GFR despite decreases in renal ______ flow.
The release of ______ is a compensatory mechanism in response to decreased renal perfusion.
The release of ______ is a compensatory mechanism in response to decreased renal perfusion.
Inhibition of the RAAS will correct the hypertension but also will ↓ GFR and aggravate _____ if renal ischemia was grave.
Inhibition of the RAAS will correct the hypertension but also will ↓ GFR and aggravate _____ if renal ischemia was grave.
Inhibitors of plasma renin activity include _____ such as aliskiren.
Inhibitors of plasma renin activity include _____ such as aliskiren.
Normal S.creatinine is _____ mg/dl.
Normal S.creatinine is _____ mg/dl.
Captopril, zofenopril, and alacepril are examples of SH-containing _____ inhibitors.
Captopril, zofenopril, and alacepril are examples of SH-containing _____ inhibitors.
ACE inhibitors inhibit Ang-converting enzyme (ACE) leading to the inhibition of both Ang-II formation and _____ release.
ACE inhibitors inhibit Ang-converting enzyme (ACE) leading to the inhibition of both Ang-II formation and _____ release.
If S.creatinine is up to 3 mg/dl, you can block the RAAS, but blocking the RAAS is dangerous if S.creatinine is greater than _____ mg/dl.
If S.creatinine is up to 3 mg/dl, you can block the RAAS, but blocking the RAAS is dangerous if S.creatinine is greater than _____ mg/dl.
ACE inhibitor frequency of administration varies, with Captopril being administered every _____ hours.
ACE inhibitor frequency of administration varies, with Captopril being administered every _____ hours.
Bradykinin is prevented from degradation primarily through the action of _____ inhibitors.
Bradykinin is prevented from degradation primarily through the action of _____ inhibitors.
Match the following ACE inhibitors with their pharmacological properties:
Match the following ACE inhibitors with their pharmacological properties:
Match the following substances with their role in the RAAS system:
Match the following substances with their role in the RAAS system:
Match the following statements about RAAS inhibition with their outcomes:
Match the following statements about RAAS inhibition with their outcomes:
Match the following drugs with their administration frequency:
Match the following drugs with their administration frequency:
Match the following ACE inhibitors with their types regarding SH group presence:
Match the following ACE inhibitors with their types regarding SH group presence:
Match the following conditions with their implications for RAAS blocking:
Match the following conditions with their implications for RAAS blocking:
Match the following mechanisms of action to their effects:
Match the following mechanisms of action to their effects:
Match the following RAAS inhibitors with their specific types:
Match the following RAAS inhibitors with their specific types:
Match the following components of the RAAS system with their functions:
Match the following components of the RAAS system with their functions:
Match the following outcomes with the corresponding triggers of the RAAS system:
Match the following outcomes with the corresponding triggers of the RAAS system:
Match the following effects of Angiotensin II with their specific vascular impacts:
Match the following effects of Angiotensin II with their specific vascular impacts:
Match the ACE inhibitors with their notable characteristics:
Match the ACE inhibitors with their notable characteristics:
Match the following pathophysiological states with their relation to RAAS activation:
Match the following pathophysiological states with their relation to RAAS activation:
Match the following statements about renal function with their implications on RAAS:
Match the following statements about renal function with their implications on RAAS:
Match the following concepts related to the RAAS system with their descriptions:
Match the following concepts related to the RAAS system with their descriptions:
Match the following ACE inhibitor characteristics with their implications in therapy:
Match the following ACE inhibitor characteristics with their implications in therapy:
Flashcards are hidden until you start studying
Study Notes
Overview of RAAS and ACE Inhibitors
- RAAS (renin-angiotensin-aldosterone system) regulates blood pressure and fluid balance.
- Renal ischemia leads to decreased renal blood flow (RBF) and glomerular filtration rate (GFR), risking acute tubular necrosis.
- Juxtaglomerular cells release renin to initiate RAAS as a compensatory response.
- Angiotensin II (Ang-II) activates AT1 receptors in kidney efferent arterioles, causing vasoconstriction (VC) to support GFR despite reduced RBF.
- Ang-II also causes systemic VC and promotes cell hypertrophy and apoptosis in other tissues, leading to degenerative changes.
Impact of Inhibiting RAAS
- Inhibiting RAAS corrects hypertension but may worsen renal function in severe renal ischemia.
- Normal serum creatinine (S.creatinine) levels range from 0.3-1.2 mg/dl; levels above 3 mg/dl indicate severe renal impairment.
- In mild renal impairment (S.creatinine up to 3 mg/dl), RAAS blockade is generally safe.
- In severe renal impairment, RAAS inhibition is dangerous and can exacerbate renal failure (RF).
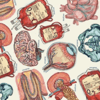
Types of Angiotensin-Converting Enzyme Inhibitors (ACEIs)
- SH-containing drugs: Captopril, zofenopril, alacepril.
- Non-SH-containing drugs: Enalapril, fosinopril, lisinopril, benazepril, ramipril.
Pharmacological Properties of Selected ACEIs
-
Captopril
- SH group: Yes
- Immune side effects: Yes
- Prodrug: No
- Metabolism: Liver, kidney
- Onset: 1-4 hours
- Frequency: Every 8 hours
- Sub-lingual dose: 25 mg
-
Fosinopril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver, kidney
- Frequency: Every 12 hours
-
Enalapril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Every 12 hours
-
Lisinopril
- SH group: No
- Immune side effects: No
- Prodrug: No
- Metabolism: No hepatic metabolism, kidney excretion
- Frequency: Once daily
-
Benazepril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Once daily
Mechanism of Action of ACEIs
- ACEIs block angiotensin-converting enzyme (ACE) in vascular endothelium.
- Result in:
- Reduced formation of Ang-II and aldosterone, decreasing vasoconstriction and salt & water retention.
- Inhibition of bradykinin degradation, enhancing vasodilation effects.
Overview of RAAS and ACE Inhibitors
- RAAS (renin-angiotensin-aldosterone system) regulates blood pressure and fluid balance.
- Renal ischemia leads to decreased renal blood flow (RBF) and glomerular filtration rate (GFR), risking acute tubular necrosis.
- Juxtaglomerular cells release renin to initiate RAAS as a compensatory response.
- Angiotensin II (Ang-II) activates AT1 receptors in kidney efferent arterioles, causing vasoconstriction (VC) to support GFR despite reduced RBF.
- Ang-II also causes systemic VC and promotes cell hypertrophy and apoptosis in other tissues, leading to degenerative changes.
Impact of Inhibiting RAAS
- Inhibiting RAAS corrects hypertension but may worsen renal function in severe renal ischemia.
- Normal serum creatinine (S.creatinine) levels range from 0.3-1.2 mg/dl; levels above 3 mg/dl indicate severe renal impairment.
- In mild renal impairment (S.creatinine up to 3 mg/dl), RAAS blockade is generally safe.
- In severe renal impairment, RAAS inhibition is dangerous and can exacerbate renal failure (RF).
Types of Angiotensin-Converting Enzyme Inhibitors (ACEIs)
- SH-containing drugs: Captopril, zofenopril, alacepril.
- Non-SH-containing drugs: Enalapril, fosinopril, lisinopril, benazepril, ramipril.
Pharmacological Properties of Selected ACEIs
-
Captopril
- SH group: Yes
- Immune side effects: Yes
- Prodrug: No
- Metabolism: Liver, kidney
- Onset: 1-4 hours
- Frequency: Every 8 hours
- Sub-lingual dose: 25 mg
-
Fosinopril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver, kidney
- Frequency: Every 12 hours
-
Enalapril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Every 12 hours
-
Lisinopril
- SH group: No
- Immune side effects: No
- Prodrug: No
- Metabolism: No hepatic metabolism, kidney excretion
- Frequency: Once daily
-
Benazepril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Once daily
Mechanism of Action of ACEIs
- ACEIs block angiotensin-converting enzyme (ACE) in vascular endothelium.
- Result in:
- Reduced formation of Ang-II and aldosterone, decreasing vasoconstriction and salt & water retention.
- Inhibition of bradykinin degradation, enhancing vasodilation effects.
Overview of RAAS and ACE Inhibitors
- RAAS (renin-angiotensin-aldosterone system) regulates blood pressure and fluid balance.
- Renal ischemia leads to decreased renal blood flow (RBF) and glomerular filtration rate (GFR), risking acute tubular necrosis.
- Juxtaglomerular cells release renin to initiate RAAS as a compensatory response.
- Angiotensin II (Ang-II) activates AT1 receptors in kidney efferent arterioles, causing vasoconstriction (VC) to support GFR despite reduced RBF.
- Ang-II also causes systemic VC and promotes cell hypertrophy and apoptosis in other tissues, leading to degenerative changes.
Impact of Inhibiting RAAS
- Inhibiting RAAS corrects hypertension but may worsen renal function in severe renal ischemia.
- Normal serum creatinine (S.creatinine) levels range from 0.3-1.2 mg/dl; levels above 3 mg/dl indicate severe renal impairment.
- In mild renal impairment (S.creatinine up to 3 mg/dl), RAAS blockade is generally safe.
- In severe renal impairment, RAAS inhibition is dangerous and can exacerbate renal failure (RF).
Types of Angiotensin-Converting Enzyme Inhibitors (ACEIs)
- SH-containing drugs: Captopril, zofenopril, alacepril.
- Non-SH-containing drugs: Enalapril, fosinopril, lisinopril, benazepril, ramipril.
Pharmacological Properties of Selected ACEIs
-
Captopril
- SH group: Yes
- Immune side effects: Yes
- Prodrug: No
- Metabolism: Liver, kidney
- Onset: 1-4 hours
- Frequency: Every 8 hours
- Sub-lingual dose: 25 mg
-
Fosinopril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver, kidney
- Frequency: Every 12 hours
-
Enalapril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Every 12 hours
-
Lisinopril
- SH group: No
- Immune side effects: No
- Prodrug: No
- Metabolism: No hepatic metabolism, kidney excretion
- Frequency: Once daily
-
Benazepril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Once daily
Mechanism of Action of ACEIs
- ACEIs block angiotensin-converting enzyme (ACE) in vascular endothelium.
- Result in:
- Reduced formation of Ang-II and aldosterone, decreasing vasoconstriction and salt & water retention.
- Inhibition of bradykinin degradation, enhancing vasodilation effects.
Overview of RAAS and ACE Inhibitors
- RAAS (renin-angiotensin-aldosterone system) regulates blood pressure and fluid balance.
- Renal ischemia leads to decreased renal blood flow (RBF) and glomerular filtration rate (GFR), risking acute tubular necrosis.
- Juxtaglomerular cells release renin to initiate RAAS as a compensatory response.
- Angiotensin II (Ang-II) activates AT1 receptors in kidney efferent arterioles, causing vasoconstriction (VC) to support GFR despite reduced RBF.
- Ang-II also causes systemic VC and promotes cell hypertrophy and apoptosis in other tissues, leading to degenerative changes.
Impact of Inhibiting RAAS
- Inhibiting RAAS corrects hypertension but may worsen renal function in severe renal ischemia.
- Normal serum creatinine (S.creatinine) levels range from 0.3-1.2 mg/dl; levels above 3 mg/dl indicate severe renal impairment.
- In mild renal impairment (S.creatinine up to 3 mg/dl), RAAS blockade is generally safe.
- In severe renal impairment, RAAS inhibition is dangerous and can exacerbate renal failure (RF).
Types of Angiotensin-Converting Enzyme Inhibitors (ACEIs)
- SH-containing drugs: Captopril, zofenopril, alacepril.
- Non-SH-containing drugs: Enalapril, fosinopril, lisinopril, benazepril, ramipril.
Pharmacological Properties of Selected ACEIs
-
Captopril
- SH group: Yes
- Immune side effects: Yes
- Prodrug: No
- Metabolism: Liver, kidney
- Onset: 1-4 hours
- Frequency: Every 8 hours
- Sub-lingual dose: 25 mg
-
Fosinopril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver, kidney
- Frequency: Every 12 hours
-
Enalapril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Every 12 hours
-
Lisinopril
- SH group: No
- Immune side effects: No
- Prodrug: No
- Metabolism: No hepatic metabolism, kidney excretion
- Frequency: Once daily
-
Benazepril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Once daily
Mechanism of Action of ACEIs
- ACEIs block angiotensin-converting enzyme (ACE) in vascular endothelium.
- Result in:
- Reduced formation of Ang-II and aldosterone, decreasing vasoconstriction and salt & water retention.
- Inhibition of bradykinin degradation, enhancing vasodilation effects.
Overview of RAAS and ACE Inhibitors
- RAAS (renin-angiotensin-aldosterone system) regulates blood pressure and fluid balance.
- Renal ischemia leads to decreased renal blood flow (RBF) and glomerular filtration rate (GFR), risking acute tubular necrosis.
- Juxtaglomerular cells release renin to initiate RAAS as a compensatory response.
- Angiotensin II (Ang-II) activates AT1 receptors in kidney efferent arterioles, causing vasoconstriction (VC) to support GFR despite reduced RBF.
- Ang-II also causes systemic VC and promotes cell hypertrophy and apoptosis in other tissues, leading to degenerative changes.
Impact of Inhibiting RAAS
- Inhibiting RAAS corrects hypertension but may worsen renal function in severe renal ischemia.
- Normal serum creatinine (S.creatinine) levels range from 0.3-1.2 mg/dl; levels above 3 mg/dl indicate severe renal impairment.
- In mild renal impairment (S.creatinine up to 3 mg/dl), RAAS blockade is generally safe.
- In severe renal impairment, RAAS inhibition is dangerous and can exacerbate renal failure (RF).
Types of Angiotensin-Converting Enzyme Inhibitors (ACEIs)
- SH-containing drugs: Captopril, zofenopril, alacepril.
- Non-SH-containing drugs: Enalapril, fosinopril, lisinopril, benazepril, ramipril.
Pharmacological Properties of Selected ACEIs
-
Captopril
- SH group: Yes
- Immune side effects: Yes
- Prodrug: No
- Metabolism: Liver, kidney
- Onset: 1-4 hours
- Frequency: Every 8 hours
- Sub-lingual dose: 25 mg
-
Fosinopril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver, kidney
- Frequency: Every 12 hours
-
Enalapril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Every 12 hours
-
Lisinopril
- SH group: No
- Immune side effects: No
- Prodrug: No
- Metabolism: No hepatic metabolism, kidney excretion
- Frequency: Once daily
-
Benazepril
- SH group: No
- Immune side effects: No
- Prodrug: Yes
- Metabolism: Liver
- Frequency: Once daily
Mechanism of Action of ACEIs
- ACEIs block angiotensin-converting enzyme (ACE) in vascular endothelium.
- Result in:
- Reduced formation of Ang-II and aldosterone, decreasing vasoconstriction and salt & water retention.
- Inhibition of bradykinin degradation, enhancing vasodilation effects.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.