Podcast
Questions and Answers
What is osteitis fibrosa cystica primarily associated with?
What is osteitis fibrosa cystica primarily associated with?
- Increased phosphate levels (correct)
- High calcium levels
- Adynamic bone disease
- Decreased GFR
Secondary hyperparathyroidism is characterized by hypocalcemia and hypophosphatemia.
Secondary hyperparathyroidism is characterized by hypocalcemia and hypophosphatemia.
False (B)
What enzyme's inhibition leads to calcitriol deficiency in patients with CKD?
What enzyme's inhibition leads to calcitriol deficiency in patients with CKD?
1,25-dihydroxyvitamin D 1-alpha-hydroxylase (1,2 hydroxylase)
In chronic kidney disease, the glomerular filtration rate (GFR) tends to _____ significantly.
In chronic kidney disease, the glomerular filtration rate (GFR) tends to _____ significantly.
Match the following conditions with their definitions:
Match the following conditions with their definitions:
What is the most common cause of anemia in chronic kidney disease?
What is the most common cause of anemia in chronic kidney disease?
In chronic kidney disease, elevated levels of erythropoietin (EPO) contribute to anemia.
In chronic kidney disease, elevated levels of erythropoietin (EPO) contribute to anemia.
What effect does hypoxia have on erythropoietin production?
What effect does hypoxia have on erythropoietin production?
Chronic inflammation stimulates the production of __________, which contributes to anemia.
Chronic inflammation stimulates the production of __________, which contributes to anemia.
Match the following complications of anemia in chronic kidney disease with their consequences:
Match the following complications of anemia in chronic kidney disease with their consequences:
What is the primary consequence of a decrease in the number of viable nephrons in chronic kidney disease?
What is the primary consequence of a decrease in the number of viable nephrons in chronic kidney disease?
Viable nephrons can be regenerated or replaced after birth.
Viable nephrons can be regenerated or replaced after birth.
What is the most common cause of chronic kidney disease?
What is the most common cause of chronic kidney disease?
The primary determinant of renal function decline in chronic kidney disease is the __________.
The primary determinant of renal function decline in chronic kidney disease is the __________.
Match the following conditions with their descriptions:
Match the following conditions with their descriptions:
Which of the following iron therapies is administered intravenously?
Which of the following iron therapies is administered intravenously?
EPO-α has a half-life of 8.5 hours.
EPO-α has a half-life of 8.5 hours.
What is the prerequisite to start EPO therapy in terms of TSAT?
What is the prerequisite to start EPO therapy in terms of TSAT?
Daprodustat is classified as a _______ hydroxylase inhibitor.
Daprodustat is classified as a _______ hydroxylase inhibitor.
Match the drugs with their characteristics:
Match the drugs with their characteristics:
What can cause anemia in patients with chronic kidney disease?
What can cause anemia in patients with chronic kidney disease?
Anemia can develop independently of changes in the Glomerular Filtration Rate (GFR) in chronic kidney disease.
Anemia can develop independently of changes in the Glomerular Filtration Rate (GFR) in chronic kidney disease.
What is the primary condition that leads to anemia in chronic kidney disease?
What is the primary condition that leads to anemia in chronic kidney disease?
Anemia appears in chronic kidney disease when the Glomerular Filtration Rate (GFR) __________.
Anemia appears in chronic kidney disease when the Glomerular Filtration Rate (GFR) __________.
Match the following terms related to chronic kidney disease with their correct descriptions:
Match the following terms related to chronic kidney disease with their correct descriptions:
What is the leading cause of mortality in ESRD patients?
What is the leading cause of mortality in ESRD patients?
Younger patients with CKD have a significantly lower risk of cardiac disease compared to the control population.
Younger patients with CKD have a significantly lower risk of cardiac disease compared to the control population.
What is the best marker for myocardial infarction in CKD patients?
What is the best marker for myocardial infarction in CKD patients?
In CKD, preserved ejection fraction (EF) is often associated with _________.
In CKD, preserved ejection fraction (EF) is often associated with _________.
Match the conditions with their corresponding features in CKD:
Match the conditions with their corresponding features in CKD:
Which of the following is a clinical feature of Calciphylaxis?
Which of the following is a clinical feature of Calciphylaxis?
Patients with CKD should strictly avoid calcium and Vitamin D supplements.
Patients with CKD should strictly avoid calcium and Vitamin D supplements.
What is the primary cause of Nephrogenic Systemic Fibrosis?
What is the primary cause of Nephrogenic Systemic Fibrosis?
In the case of Calciphylaxis, the arterioles undergo medial __________ due to vasculopathy.
In the case of Calciphylaxis, the arterioles undergo medial __________ due to vasculopathy.
Match the body part with its corresponding image description related to Calciphylaxis:
Match the body part with its corresponding image description related to Calciphylaxis:
Which of the following is NOT an indication for dialysis?
Which of the following is NOT an indication for dialysis?
A holistic approach to CKD treatment should include the use of tobacco products.
A holistic approach to CKD treatment should include the use of tobacco products.
What is the target LDL level for patients with diabetic CKD?
What is the target LDL level for patients with diabetic CKD?
The first-line drug therapy for managing proteinuria includes ACE(-) or ARBS and _____ for most patients.
The first-line drug therapy for managing proteinuria includes ACE(-) or ARBS and _____ for most patients.
Match the following components with their respective descriptions:
Match the following components with their respective descriptions:
What could be a hurdle for a patient fit for transplantation?
What could be a hurdle for a patient fit for transplantation?
The mortality rates after the initiation of dialysis decrease over time.
The mortality rates after the initiation of dialysis decrease over time.
What is the main reason for creating an AV fistula before dialysis treatment?
What is the main reason for creating an AV fistula before dialysis treatment?
What is the GFR range for Stage G3a in kidney classification?
What is the GFR range for Stage G3a in kidney classification?
Cardiac complications are the most common cause of death in kidney disease.
Cardiac complications are the most common cause of death in kidney disease.
List two reversible causes of kidney dysfunction.
List two reversible causes of kidney dysfunction.
Stage G4 of kidney classification corresponds to a GFR of _____ ml/min.
Stage G4 of kidney classification corresponds to a GFR of _____ ml/min.
Match the following complications with their characteristics:
Match the following complications with their characteristics:
Which of the following is a first-line treatment for high bone turnover in CKD?
Which of the following is a first-line treatment for high bone turnover in CKD?
Pure phosphate binders can lead to decreased LDL levels.
Pure phosphate binders can lead to decreased LDL levels.
What is the target calcium level in CKD management?
What is the target calcium level in CKD management?
In chronic kidney disease, the normal range for PTH is __________ pg/ml.
In chronic kidney disease, the normal range for PTH is __________ pg/ml.
Match the following treatments with their related features:
Match the following treatments with their related features:
Flashcards are hidden until you start studying
Study Notes
Anemia in Chronic Kidney Disease
- Anemia is a common complication of chronic kidney disease (CKD) and can be caused by decreased red blood cell (RBC) production or decreased RBC survival.
- Decreased RBC production is more common and is due to low iron levels, poor iron absorption, and blood loss.
- Decreased RBC survival is less common and is due to increased RBC destruction or reduced red blood cell lifespan.
Hypoxia-Inducible Factor (HIF)-alpha
- Hypoxia (low oxygen) triggers the activation of HIF-alpha.
- HIF-alpha stimulates erythropoietin (EPO) production in the kidneys, leading to increased RBC production.
- In CKD, the kidneys are damaged and lose their ability to produce EPO, leading to anemia.
- Inflammation and other factors contribute to anemia in CKD.
Iron Therapy
- Iron therapy is the first step in managing anemia in CKD.
- Iron deficiency is the most common cause of ESA hyporesponsiveness.
- Formulas are available to determine iron requirements.
- Oral iron supplements are less effective than intravenous iron therapy.
- Intravenous iron therapy is preferred for patients with significant iron deficiency.
EPO Stimulating Agents (ESA)
- ESA are used to stimulate red blood cell production.
- ESA are only given to patients with adequate iron stores.
- EPO-alpha and EPO-beta are commonly used ESA.
- Darbepoetin is a long-acting EPO-beta that may increase the hematocrit more effectively than EPO-alpha.
- Daprodustat is prolyl hydroxylase inhibitor which may be a future alternative to ESA.
Chronic Kidney Disease (CKD)
- CKD is a progressive disease that leads to a decline in glomerular filtration rate (GFR).
- The number of viable nephrons declines in CKD, which causes intraglomerular hypertension and proteinuria.
- GFR can be calculated using different methods:
- Cockcroft-Gault formula
- MDRD equation
- CKD-EPI equation
Management of CKD
- Lifestyle modifications are essential for managing CKD.
- Medications can be used to manage proteinuria, hypertension, and other complications.
- Dialysis may be needed for patients with advanced CKD.
- Kidney transplantation may be an option for some patients.
CKD - Mineral Bone Disease
- CKD-MBD is a complex disorder that affects bone metabolism.
- High bone turnover is characterized by osteitis fibrosa cystica.
- Low bone turnover is characterized by adynamic bone disease.
- Calcification is a common complication of CKD-MBD.
- Treatment of CKD-MBD involves managing phosphate levels, calcium levels, and vitamin D levels.
- Phosphate binders are the first-line treatment for hyperphosphatemia.
- Calcitriol is a vitamin D analogue that can be used to treat hypocalcemia and hyperparathyroidism.
- Bisphosphonates can be used to treat low bone mass.
- Calcium and vitamin D supplements should be used with caution in CKD patients.
CKD - Cardiovascular System
- Cardiovascular disease is a major cause of death in CKD patients.
- CKD patients have an increased risk of heart disease and hypertension.
- Uremic toxins contribute to cardiovascular disease in CKD.
- Early diagnosis and treatment of cardiovascular disease are essential in CKD patients.
- Pre-transplant evaluation for vascular calcification is mandatory.
Telegram channel - @back_ed8
- The Telegram channel @back_ed8 contains more information on nephrology.
Nephrology
- This appears to be the label or a reference to a specific section within the document.
Rate of Fall of GFR (ml/min/year)
- The rate of decline in GFR varies depending on the underlying cause of CKD.
- DKD (Diabetic Kidney Disease) is the most common cause with a rapid rate of decline in GFR.
- CGN (Chronic Glomerulonephritis) has a moderate rate of decline in GFR.
- IN (Ischemic Nephropathy) has a slower rate of decline in GFR.
- CTID (Chronic Tubulointerstitial Disease) has the slowest rate of decline in GFR.
Classification (GFR)
- The stages of CKD are classified based on GFR.
- Stage 1 is characterized by GFR > 90 ml/min.
- Stage 5 is characterized by GFR <15 ml/min or end-stage renal disease (ESRD).
Complications (Mnemonic: ABCDE)
- Common complications of CKD:
- Anemia
- Acidosis
- Access for dialysis
- Bone mineral disease
- Cardiac complications
- Dry weight
- Electrolyte imbalances
- Uremia
Management
- Diagnosis of CKD is based on:
- Presence of kidney damage
- Decreased GFR
- History of CKD
- Treatment:
- Address reversible causes.
- Manage complications.
- Monitor GFR.
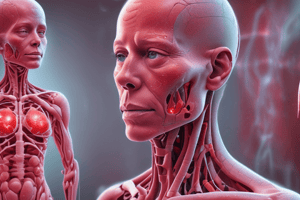
CKD - Calciphylaxis & Cardiovascular Changes
-
Calciphylaxis is a rare but serious complication of CKD.
-
It is characterized by painful, ischemic necrosis of the skin and subcutaneous fat.
-
The pathogenesis of calciphylaxis is complex and involves hyperphosphatemia, vitamin K deficiency, and vascular calcification.
-
It is associated with a high mortality rate.
-
Treatment usually involves supportive care, wound care, and treatment of hyperphosphatemia.
-
The document lists specific figures and tables.
-
The document is a protocol or treatment guide for chronic kidney disease (CKD).
-
Some of the tables and graphs are related to dialysis, particularly the "Total Glomerular Filtration Rate (GFR)" and "Plasma Concentration" graphs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.