Podcast
Questions and Answers
What is the main function of the autonomic innervation of the parotid gland?
What is the main function of the autonomic innervation of the parotid gland?
- Regulation of blood pressure
- Regulation of body temperature
- Modulation of facial expressions
- Control of saliva production rate (correct)
Which nerve carries parasympathetic fibers from the otic ganglion to the parotid gland?
Which nerve carries parasympathetic fibers from the otic ganglion to the parotid gland?
- Glossopharyngeal nerve
- Lesser petrosal nerve
- Great auricular nerve
- Auriculotemporal nerve (correct)
What is the effect of sympathetic stimulation on saliva secretion?
What is the effect of sympathetic stimulation on saliva secretion?
- No effect on saliva production
- Decreased saliva production (correct)
- Increased saliva production
- Variable effect on saliva production
Which of the following structures is not drained by the deep set of lymph nodes?
Which of the following structures is not drained by the deep set of lymph nodes?
Which of the following areas is NOT drained by the superficial set of lymph nodes of the parotid gland?
Which of the following areas is NOT drained by the superficial set of lymph nodes of the parotid gland?
What is the origin of the sympathetic innervation to the parotid gland?
What is the origin of the sympathetic innervation to the parotid gland?
What is the main function of the buccal fat pad?
What is the main function of the buccal fat pad?
Which artery is NOT a branch of the external carotid artery?
Which artery is NOT a branch of the external carotid artery?
How many lobes is the buccal fat pad divided into?
How many lobes is the buccal fat pad divided into?
What is the primary function of the retromandibular vein?
What is the primary function of the retromandibular vein?
What surrounds the parotid duct?
What surrounds the parotid duct?
What is unique about the lymphatic drainage of the parotid gland compared to other salivary glands?
What is unique about the lymphatic drainage of the parotid gland compared to other salivary glands?
What lies between the anterior and posterior lobes of the buccal fat pad?
What lies between the anterior and posterior lobes of the buccal fat pad?
What happens to the intermediate lobe of the buccal fat pad between childhood and adulthood?
What happens to the intermediate lobe of the buccal fat pad between childhood and adulthood?
What is the main difference between the buccal fat pad and the jowl fat pads?
What is the main difference between the buccal fat pad and the jowl fat pads?
What is the function of the sublevator extension of the buccal fat pad?
What is the function of the sublevator extension of the buccal fat pad?
What is the primary function of the parotid gland's secretions in the oral cavity?
What is the primary function of the parotid gland's secretions in the oral cavity?
What is the anatomical boundary superior to the parotid region?
What is the anatomical boundary superior to the parotid region?
Which structure passes through the parotid gland and is responsible for innervating the muscles of facial expression?
Which structure passes through the parotid gland and is responsible for innervating the muscles of facial expression?
Where does the Stensen duct pierce to enter the oral cavity?
Where does the Stensen duct pierce to enter the oral cavity?
What is the name of the artery that arises from the external carotid artery within the parotid gland?
What is the name of the artery that arises from the external carotid artery within the parotid gland?
What is the name of the vein formed by the convergence of the superficial temporal and maxillary veins within the parotid gland?
What is the name of the vein formed by the convergence of the superficial temporal and maxillary veins within the parotid gland?
What is the name of the small papilla where the Stensen duct enters the oral cavity?
What is the name of the small papilla where the Stensen duct enters the oral cavity?
What is the morphology of the parotid gland?
What is the morphology of the parotid gland?
What is the primary function of the buccal fat pad in relation to chewing and suckling?
What is the primary function of the buccal fat pad in relation to chewing and suckling?
What is the most common site of a salivary gland tumour?
What is the most common site of a salivary gland tumour?
What is the name of the procedure that involves the surgical excision of the tumour and parotid gland?
What is the name of the procedure that involves the surgical excision of the tumour and parotid gland?
What is the result of damage to the facial nerve or its branches during a parotidectomy?
What is the result of damage to the facial nerve or its branches during a parotidectomy?
What is the name of the nerve that provides sensory innervation to the parotid gland and the external ear?
What is the name of the nerve that provides sensory innervation to the parotid gland and the external ear?
What is the result of the parotid gland being enclosed in a tough fibrous capsule?
What is the result of the parotid gland being enclosed in a tough fibrous capsule?
What is the name of the condition where the inferior eyelid falls away from the eyeball?
What is the name of the condition where the inferior eyelid falls away from the eyeball?
What is the term for inflammation of the parotid gland?
What is the term for inflammation of the parotid gland?
What is the most common way the parotid gland becomes infected?
What is the most common way the parotid gland becomes infected?
What is the primary cause of pain in acute parotitis?
What is the primary cause of pain in acute parotitis?
What is the location of the parotid duct in relation to the zygomatic arch?
What is the location of the parotid duct in relation to the zygomatic arch?
What is the typical outcome of a malignant tumor of the parotid gland?
What is the typical outcome of a malignant tumor of the parotid gland?
What is the explanation for the appearance of beads of perspiration on the skin covering the parotid gland in Frey's syndrome?
What is the explanation for the appearance of beads of perspiration on the skin covering the parotid gland in Frey's syndrome?
What is the location of the facial nerve in relation to the parotid salivary gland?
What is the location of the facial nerve in relation to the parotid salivary gland?
What is the typical location of the parotid duct in the mouth?
What is the typical location of the parotid duct in the mouth?
What is the characteristic of a benign parotid neoplasm?
What is the characteristic of a benign parotid neoplasm?
Flashcards are hidden until you start studying
Study Notes
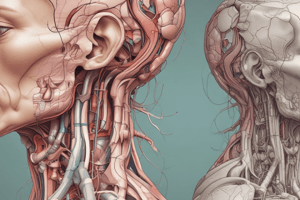
The Parotid Gland
- Bilateral salivary gland located in the face, producing serous saliva (watery solution rich in enzymes) to lubricate and aid in food breakdown in the oral cavity
- Anatomical position:
- Divided into deep and superficial lobes, separated by the facial nerve
- Lies within the parotid region, bounded by:
- Superiorly: Zygomatic arch
- Inferiorly: Inferior border of the mandible
- Anteriorly: Masseter muscle
- Posteriorly: External ear and sternocleidomastoid
Secretions and Duct
- Secretions are transported to the oral cavity by the Stensen duct
- Duct:
- Arises from the anterior surface of the gland, traversing the masseter muscle
- Pierces the buccinator, moving medially to enter the vestibule of the mouth opposite the upper second molar tooth
Anatomical Relationships
- Clinically important during parotid gland surgery
- Neurovascular structures passing through the gland:
- Facial nerve (CN VII): gives rise to five terminal branches, innervating muscles of facial expression
- External carotid artery: gives rise to the posterior auricular artery within the parotid gland
- Retromandibular vein: formed by the convergence of the superficial temporal and maxillary veins, responsible for venous drainage of the face
Blood Supply and Drainage
- Arterial supply: posterior auricular and superficial temporal arteries, both branches of the external carotid artery
- Venous drainage: retromandibular vein
Innervation
- Receives sensory and autonomic innervation
- Autonomic innervation controls the rate of saliva production
- Sensory innervation supplied by the auriculotemporal nerve (gland) and the great auricular nerve (fascia)
- Parasympathetic innervation:
- Begins with the glossopharyngeal nerve
- Reaches the gland via the lesser petrosal nerve to the otic ganglion
- Auriculotemporal nerve carries parasympathetic fibers from the otic ganglion to the parotid gland
- Sympathetic innervation:
- Originates from the superior cervical ganglion (part of the paravertebral chain)
- Fibers travel along the external carotid artery to reach the parotid gland
Lymphatic Drainage
- Numerous lymph nodes distributed throughout and around the substance of the parotid gland
- Nodes are distributed in both superficial and deep lobes
- Majority of nodes (about 90%) are found in the superficial node
- Nodes drain various structures, including:
- External acoustic meatus, auricle, scalp, eyelids, and lacrimal glands
- Soft palate, middle ear, and nasopharynx
The Buccal Fat Pad
- Encapsulated fat mass in the cheek, located between the buccinator muscle and several superficial muscles
- Inferior portion is contained within the buccal space
- Implicated in the formation of hollow cheeks and the nasolabial fold, but not in the formation of jowls
- Composed of several parts, including:
- Anterior, intermediate, and posterior lobes
- Four extensions: sublevator, melolabial, buccal, and pterygoid
Clinical Relevance: Disorders of the Parotid Gland
- Parotid gland tumors:
- Most common site of salivary gland tumors
- Usually benign, such as an adenolymphoma
- Treatment involves surgical excision of the tumor and parotid gland (parotidectomy)
- Parotitis:
- Inflammation of the parotid gland, usually due to infection
- Pain referred to the external ear due to the auriculotemporal nerve
- Parotid duct injury:
- May be damaged in facial injuries or during surgical operations
- Duct is superficial, passing forward across the masseter about a fingerbreadth below the zygomatic arch
- Parotid salivary gland and lesions of the facial nerve:
- Benign parotid neoplasm rarely causes facial palsy
- Malignant tumor of the parotid is highly invasive and may involve the facial nerve, causing unilateral facial paralysis
- Frey's syndrome:
- Interesting complication that develops after penetrating wounds of the parotid gland
- Characterized by beads of perspiration on the skin covering the parotid when eating
- Caused by damage to the auriculotemporal and great auricular nerves
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.