Podcast
Questions and Answers
What is the primary function of the microvilli in the Proximal Convoluted Tubule (PCT) cells?
What is the primary function of the microvilli in the Proximal Convoluted Tubule (PCT) cells?
- To enhance the folding of the basolateral membrane
- To facilitate the exocytosis of waste molecules
- To regulate the tight junctions between adjacent cells
- To increase the surface area for passive transport (correct)
What is the role of the filtration slits in the glomerulus?
What is the role of the filtration slits in the glomerulus?
- To store waste molecules before excretion
- To facilitate the passage of substances into the capsular space (correct)
- To filter out large molecules from the bloodstream
- To regulate the pressure of the glomerulus
What is the main function of the basement membrane in the glomerulus?
What is the main function of the basement membrane in the glomerulus?
- To facilitate the passage of substances through the filtration slits (correct)
- To provide mechanical support to the podocytes
- To regulate the flow of substances into the capsular space
- To filter out small molecules from the bloodstream
What is the primary function of the mitochondria in the PCT cells?
What is the primary function of the mitochondria in the PCT cells?
What is the main function of the tight junctions between adjacent PCT cells?
What is the main function of the tight junctions between adjacent PCT cells?
What is the main characteristic of the PCT cells in terms of permeability?
What is the main characteristic of the PCT cells in terms of permeability?
What is the function of the podocytes in the glomerulus?
What is the function of the podocytes in the glomerulus?
What is the primary function of the fenestrations in the glomerulus?
What is the primary function of the fenestrations in the glomerulus?
Which structure is responsible for collecting urine from the renal pyramids before it is conveyed to the ureter?
Which structure is responsible for collecting urine from the renal pyramids before it is conveyed to the ureter?
What is the primary role of the peritubular capillaries in the kidney?
What is the primary role of the peritubular capillaries in the kidney?
Which structure carries blood away from the glomerulus?
Which structure carries blood away from the glomerulus?
Which pathway does blood follow after leaving the vasa recta?
Which pathway does blood follow after leaving the vasa recta?
What is the function of the renal columns?
What is the function of the renal columns?
Why do the renal pyramids appear striated?
Why do the renal pyramids appear striated?
Which blood vessels directly feed into the glomerulus?
Which blood vessels directly feed into the glomerulus?
What is the sequence of urine flow from the renal pyramids to the bladder?
What is the sequence of urine flow from the renal pyramids to the bladder?
Which cells of the Juxtaglomerular Apparatus serve as baroreceptors sensitive to blood pressure?
Which cells of the Juxtaglomerular Apparatus serve as baroreceptors sensitive to blood pressure?
What structures deliver urine through papillae into minor calyces?
What structures deliver urine through papillae into minor calyces?
Which cells in the JGA possess secretory granules containing renin?
Which cells in the JGA possess secretory granules containing renin?
What is the primary function of macula densa cells in the JGA?
What is the primary function of macula densa cells in the JGA?
What is the main characteristic of principal cells in the late distal convoluted tubule and cortical collecting duct?
What is the main characteristic of principal cells in the late distal convoluted tubule and cortical collecting duct?
Which cell type in the JGA acts as mechanoreceptors sensing blood pressure in the afferent arterioles?
Which cell type in the JGA acts as mechanoreceptors sensing blood pressure in the afferent arterioles?
Which cells are interconnected by gap junctions in the JGA?
Which cells are interconnected by gap junctions in the JGA?
Where is the juxtaglomerular apparatus located in relation to the afferent and efferent arterioles?
Where is the juxtaglomerular apparatus located in relation to the afferent and efferent arterioles?
Which is a function of intercalated cells in the kidneys?
Which is a function of intercalated cells in the kidneys?
What is the primary role of the myogenic mechanism in renal autoregulation?
What is the primary role of the myogenic mechanism in renal autoregulation?
What is a key characteristic of principal cells in the medullary collecting duct?
What is a key characteristic of principal cells in the medullary collecting duct?
What happens to the afferent arteriole when blood pressure decreases?
What happens to the afferent arteriole when blood pressure decreases?
What primarily regulates the permeability of principal cells to water and solutes?
What primarily regulates the permeability of principal cells to water and solutes?
Which of the following best describes the effect of high blood pressure on the afferent arteriole?
Which of the following best describes the effect of high blood pressure on the afferent arteriole?
In urine formation, what remains in the blood plasma after filtration?
In urine formation, what remains in the blood plasma after filtration?
What is the main factor that the tubuloglomerular mechanism responds to?
What is the main factor that the tubuloglomerular mechanism responds to?
Which of the following statements about urine formation is correct?
Which of the following statements about urine formation is correct?
Which cells are sensitive to filtrate NaCl osmolarity in the tubuloglomerular mechanism?
Which cells are sensitive to filtrate NaCl osmolarity in the tubuloglomerular mechanism?
Where do large quantities of water and solutes initially pass into during urine formation?
Where do large quantities of water and solutes initially pass into during urine formation?
How does the myogenic mechanism help to regulate glomerular blood flow?
How does the myogenic mechanism help to regulate glomerular blood flow?
Which structural feature is NOT common between principal cells and intercalated cells?
Which structural feature is NOT common between principal cells and intercalated cells?
What percentage of the filtrate ultimately becomes urine?
What percentage of the filtrate ultimately becomes urine?
Flashcards are hidden until you start studying
Study Notes
The Juxtaglomerular Apparatus (JGA)
- Located at the initial portion of the distal tubule where it passes between the afferent and efferent arterioles.
- Forms a monitoring structure that includes cells from arterioles and the thick ascending loop of Henle.
Cell Populations of the JGA
- Juxtaglomerular (JG) Cells: Modified smooth muscle cells in the afferent arteriole.
- Act as baroreceptors for blood pressure detection.
- Contain secretory granules with renin.
- Macula Densa Cells: Located in the thick ascending loop.
- Function as chemoreceptors monitoring NaCl levels in the filtrate.
- Extraglomerular Mesangial Cells: Interconnected and may relay signals between the macula densa and granular cells.
Late Distal Convoluted Tubule (DCT) and Cortical Collecting Duct
- Collecting ducts merge to deliver urine into minor calyces.
- Two cell types:
- Principal Cells: Fewer microvilli, respond to hormones regulating water and solute permeability.
- Intercalated Cells: Secrete hydrogen ions for acid-base balance during increased body acidity.
Regulation of Glomerular Filtration Rate (GFR)
-
Myogenic Mechanism: Smooth muscle cells in the afferent arterioles contract or relax in response to blood pressure changes.
- High blood pressure results in vasoconstriction; low blood pressure causes dilation.
-
Tubuloglomerular Feedback: Involves sensitivity of macula densa cells to filtrate NaCl osmolarity and flow rates.
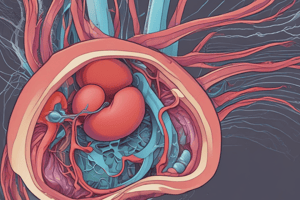
Filtration Mechanism
- Filtration membrane consists of capillary endothelium, basement membrane, and podocytes.
- Filtration occurs through fenestrations, basement membranes, and filtration slits, allowing selective passage of substances into the capsular space.
Proximal Convoluted Tubule (PCT)
- Composed of brush border cells with numerous microvilli for increased reabsorption surface area.
- Tight junctions allow water passage but restrict large molecules.
- Basolateral membrane features integral proteins for transport, supported by abundant mitochondria for ATP generation.
Renal Medulla
- Contains renal pyramids that drain into minor calyces.
- Renal columns are extensions of the cortex allowing for blood vessels and nerve passage.
Renal Pelvis
- Funnel-shaped structure within the renal sinus collecting urine from pyramids and transporting it to the ureter.
Nephron Structure
- Comprised of specialized tubular structures along with associated blood vessels.
- Blood flow: Renal artery → segmental arteries → lobar arteries → interlobar arteries → arcuate arteries → interlobular arteries → afferent arterioles → glomerulus.
- Efferent arterioles drain the glomeruli into peritubular capillaries and vasa recta.
Urine Formation Mechanisms
- Kidneys filter the body’s plasma volume approximately 60 times daily.
- Filtrate: Comprises everything in blood plasma minus proteins.
- Urine: Less than 1% of total filtrate, primarily containing metabolic wastes and surplus substances.
- Three key processes in urine formation:
- Filtration
- Reabsorption
- Secretion
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.