Podcast
Questions and Answers
What is the functional unit of the kidneys composed of?
What is the functional unit of the kidneys composed of?
- Renal pelvis and calices
- Nephron and renal sinus
- Renal lobe and pyramid
- Renal cortex and medulla (correct)
What is the main function of the proximal convoluted tubules?
What is the main function of the proximal convoluted tubules?
- Selective reabsorption of most of the water and other molecules (correct)
- Secretion of waste products
- Filtration of water and small molecules
- Regulation of blood pressure
What is the composition of the renal capsule?
What is the composition of the renal capsule?
- Adventitia, submucosae, and smooth muscle
- Smooth muscle, adventitia, and epithelium
- Collagen fibers, smooth muscle, and blood vessels (correct)
- Urothelium, submucosae, and smooth muscle
What is the characteristic feature of multilobular kidneys found in large ruminants?
What is the characteristic feature of multilobular kidneys found in large ruminants?
What is the site of osmoregulation in the kidneys?
What is the site of osmoregulation in the kidneys?
What is the function of the Loop of Henle?
What is the function of the Loop of Henle?
What is the characteristic feature of proximal convoluted tubules?
What is the characteristic feature of proximal convoluted tubules?
What is the composition of the renal medulla?
What is the composition of the renal medulla?
What is the primary function of the lamina densa in the glomerular basement membrane?
What is the primary function of the lamina densa in the glomerular basement membrane?
What type of endothelium allows for the 'free' transfer of plasma proteins, red and white blood cells, water, and most molecules?
What type of endothelium allows for the 'free' transfer of plasma proteins, red and white blood cells, water, and most molecules?
What is the approximate size of the filtration slits in the glomerular capillary loops?
What is the approximate size of the filtration slits in the glomerular capillary loops?
What is the primary composition of the ultrafiltrate produced by ultrafiltration of blood in the renal corpuscle?
What is the primary composition of the ultrafiltrate produced by ultrafiltration of blood in the renal corpuscle?
What percentage of the glomerular filtrate is reabsorbed in the renal tubules?
What percentage of the glomerular filtrate is reabsorbed in the renal tubules?
What type of molecules can pass through the fenestrations in fenestrated endothelium?
What type of molecules can pass through the fenestrations in fenestrated endothelium?
What is the function of podocytes with pedicles (foot processes) in the filtration barrier?
What is the function of podocytes with pedicles (foot processes) in the filtration barrier?
What is the outcome of the filtration barrier?
What is the outcome of the filtration barrier?
What is the primary function of the renal corpuscle?
What is the primary function of the renal corpuscle?
What is the main difference between the glomerulus of deep-sea fish and that of other animals?
What is the main difference between the glomerulus of deep-sea fish and that of other animals?
What is the composition of the mesangium?
What is the composition of the mesangium?
What is the function of mesangial cells?
What is the function of mesangial cells?
What is the site of ultrafiltration in the renal corpuscle?
What is the site of ultrafiltration in the renal corpuscle?
What is the function of the glomerular capillaries?
What is the function of the glomerular capillaries?
What is the composition of Bowman's capsule?
What is the composition of Bowman's capsule?
What is the fate of the ultrafiltrate produced in the glomerulus?
What is the fate of the ultrafiltrate produced in the glomerulus?
What is the primary function of the microvilli in the proximal convoluted tubules?
What is the primary function of the microvilli in the proximal convoluted tubules?
What is the percentage of sodium and water absorbed from the glomerular filtrate by the proximal convoluted tubules?
What is the percentage of sodium and water absorbed from the glomerular filtrate by the proximal convoluted tubules?
What is reabsorbed 100% from the glomerular filtrate by the proximal convoluted tubules?
What is reabsorbed 100% from the glomerular filtrate by the proximal convoluted tubules?
What is the characteristic feature of the lateral borders of the proximal convoluted tubules?
What is the characteristic feature of the lateral borders of the proximal convoluted tubules?
What is the site of tubular secretion of potassium, hydrogen, and NH4+?
What is the site of tubular secretion of potassium, hydrogen, and NH4+?
What is the function of the mitochondria in the proximal convoluted tubules?
What is the function of the mitochondria in the proximal convoluted tubules?
What is the location of the proximal convoluted tubules in the kidney?
What is the location of the proximal convoluted tubules in the kidney?
What is the characteristic feature of the basal surface of the proximal convoluted tubules?
What is the characteristic feature of the basal surface of the proximal convoluted tubules?
What is the primary function of the ureters in the urinary system?
What is the primary function of the ureters in the urinary system?
What is the correct order of urine descent in the kidney?
What is the correct order of urine descent in the kidney?
What is the primary function of the blood-urinary barrier?
What is the primary function of the blood-urinary barrier?
What hormone is produced by the kidneys to stimulate red blood cell production?
What hormone is produced by the kidneys to stimulate red blood cell production?
What is the primary function of the kidneys in maintaining electrolyte homeostasis?
What is the primary function of the kidneys in maintaining electrolyte homeostasis?
What is the significance of the juxtaglomerular apparatus in the kidneys?
What is the significance of the juxtaglomerular apparatus in the kidneys?
What is the function of the kidneys in vitamin D activation?
What is the function of the kidneys in vitamin D activation?
Flashcards are hidden until you start studying
Study Notes
Urinary System: General Info
- The kidneys excrete nitrogenous waste, conserve body fluids and electrolytes, and reabsorb solutes and water.
- The ureters convey urine to the bladder.
- The urinary bladder stores urine.
- The urethra expels urine from the body.
- Urine is an ultrafiltrate of blood.
- Clinical signs of renal and non-renal disease relate to the microanatomy and function of the kidneys.
- A dog's kidney has a normal dark red/brown cortex color, while a cat's kidney has a normal pale red cortex color due to high adipose tissue components.
Blood-Urinary Barrier
- The blood-urinary barrier consists of four components: fenestration, basement membrane, endothelial cells, and podocytes.
- Proteins always travel to the basement membrane because filtration happens here.
Urine Descent
- Urine descent takes place in the following order: proximal convoluted tubules, Loops of Henle, and then distal convoluted tubules.
Kidney Functions
- The kidneys help maintain water and electrolyte homeostasis by:
- Filtrating cellular waste from blood
- Selectively reabsorbing water and solutes
- Regulating fluid balance
- Maintaining electrolyte homeostasis/acid-base balance
- The kidneys also excrete metabolic waste products, bioactive substances (including drugs), and water.
- The kidneys produce the hormones erythropoietin and renin.
- Erythropoietin is involved in targeting bone marrow cells to increase RBC (red blood cell) production.
- Kidney damage can result in anemia.
- The kidneys regulate blood pressure via the juxtaglomerular apparatus.
- The kidneys also activate vitamin D, which aids in calcium metabolism.
Kidney Structure
- The kidneys are composed of:
- Capsule
- Renal lobe/pyramid
- Outer cortex
- Inner medulla
- Papillae/crest
- Calices
- Renal pelvis
- The calices are dilations of the renal pelvis.
- The renal pelvis is a dilation of the proximal ureter.
- The renal hilus is the area of the kidneys where arteries and veins enter/leave.
- It is normal to see adipose connective tissue in the renal sinus in low quantities.
- The nephron is the "functional unit" of the kidneys, composed of the renal cortex and medulla.
- The nephrons are the site of osmoregulation via:
- Filtration of water and small molecules from blood plasma to form a filtrate
- Selective reabsorption of most of the water and other molecules from the filtrate
Kidney Types
- Unilobular kidneys are typically found in carnivores.
- Multilobular kidneys of large ruminants lack a renal pelvis, and the kidneys' surface has each lobe distinctly outlined by deep grooves.
- Multilobular kidneys of pigs have a smooth surface.
Kidney Components
- The capsule of the kidney is composed of collagen fibers, smooth muscle, and blood vessels.
- The cortex of the kidneys is composed of:
- Renal corpuscles
- Distal and proximal convoluted tubules
- Collecting tubules
- Peritubular capillary plexuses
- Proximal convoluted tubules have a brush border.
- Distal convoluted tubules (DCT) lack a brush border.
- The medulla of the kidneys is composed of:
- Loops of Henle
- Collecting ducts
- Vasa recta
- The renal pelvis is composed of:
- Urothelium
- Submucosae
- Smooth muscle
- Adventitia
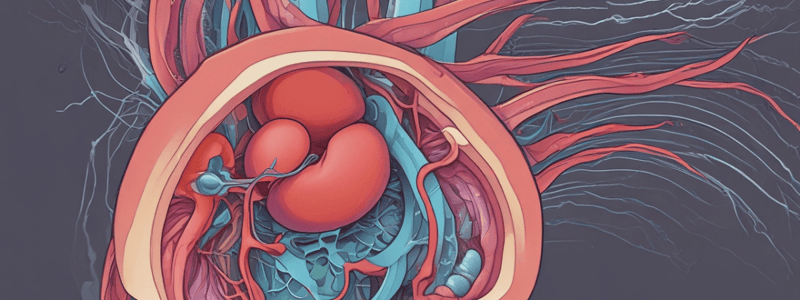
- The renal corpuscle is composed of:
- Glomerulus
- Bowman's capsule
- The renal corpuscle has the main function of protein conservation.
- The glomerulus is loops (tufts) of capillaries with fenestrated endothelium within the bowman's capsule.
- Mesangial cells lie between fenestrated capillaries and are phagocytic, contractile, and act as support.
- The glomerulus is the site of ultrafiltration and retains proteins.
- Deep sea fish lack a glomerulus and instead have renal tubules surrounded by a well-developed renal portal system, forming primitive urine by tubular secretion.
Ultrafiltration at the Glomerulus
- Vascular pole:
- Blood arrives at and enters the glomerular capillaries via the main afferent arteriole.
- Blood exits at the efferent arteriole.
- Ultrafiltration at the glomerulus:
- Blood is pushed through the filtration barrier, which is composed of:
- Fenestrated endothelium
- Glomerular basement membrane
- Podocyte foot processes
- The ultrafiltrate enters the urinary space.
- Blood is pushed through the filtration barrier, which is composed of:
- Urinary pole:
- The ultrafiltrate enters the proximal convoluted tubule.
Filtration Barrier
- The filtration barrier is composed of:
- Endothelium of glomerular capillary loops with fenestrations
- Glomerular basement membrane, which is made of fused basal laminae of capillaries and podocytes
- The glomerular basement membrane has three layers: lamina rara interna, lamina densa, and lamina rara externa
- The lamina densa of the basement membrane acts as the exclusion barrier for molecules the size of IgG and albumin.
- Podocytes with pedicles (foot processes)
Endothelium Types
- Continuous endothelium is a barrier system that controls the transfer of molecules across the cell.
- Fenestrated endothelium allows for controlled transfer of small molecules and limited amounts of protein across the fenestrae (filtration mechanism).
- Discontinued endothelium has gaps which allow for "free" transfer of plasma proteins, red and white blood cells, water, and most molecules across endothelial cells.
Urine Formation: Steps
- Step 1: Primary/glomerular filtrate is produced by ultrafiltration of blood in the renal corpuscle.
- The composition of ultrafiltrate is similar to blood plasma, but it does not contain most proteins.
- Step 2: In the renal tubules, 98% of the filtrate is reabsorbed.
- Most water and sodium, all of the glucose, and all of the amino acids from the ultrafiltrate are reabsorbed.
- Step 3: Tubular secretion of potassium, hydrogen, NH4+, bile salts, drugs, and metabolites takes place.
- Waste molecules and some water remain in the tubular system, and eventually will empty into the ureter.
- Step 4: Urine is stored in the bladder pending voiding/micturition.
Proximal Convoluted Tubule (PCT)
- The proximal convoluted tubules begin at the urinary pole of the renal corpuscle and are only located in the cortex of the kidney.
- The proximal convoluted tubule consists of a single layer of cuboidal epithelial cells with microvilli (forming the Brush border), and a basement membrane.
- The purpose of the brush border/microvilli is to increase the surface area.
- The microvilli are non-motile.
- The proximal convoluted tubules have highly metabolic active cells with many mitochondria that act as:
- Sodium-potassium pumps
- Aquaporins
- Peroxisomes
- Endosome
- Lysosomes
- The proximal convoluted tubules function to reabsorb:
- Glucose
- Na+/H2O
- Amino acids
- Peptides
- Low molecular weight proteins
- Activate vitamin D
- Low molecular weight proteins may normally be in the urine to some extent, but they are undetectable.
- Otherwise, protein should not normally be detected in the urine.
- Specifically, the PCT will absorb 85% of sodium and water from the glomerular filtrate.
- Additionally, the PCT will absorb 100% of the glucose and amino acids present in the glomerular filtrate.
- The PCT has selective reabsorption of anions, cations, and urea.
- The lateral borders of the proximal convoluted tubule have inter-digitations of lateral cell processes, making the cell limits indistinct.
- The basal surface of the PCT has a folded membrane, forming basal striations.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.