Podcast
Questions and Answers
What are the three membranes that protect the brain?
What are the three membranes that protect the brain?
- skull, cerebrospinal fluid, meninges
- dura mater, arachnoid mater, pia mater (correct)
- arachnoid mater, pia mater, cerebrospinal fluid
- skull, cerebrospinal fluid, dura mater
What is the most common cause of death and disability among Canadians under 40 years old?
What is the most common cause of death and disability among Canadians under 40 years old?
- Cancer
- Stroke
- Traumatic brain injury (correct)
- Heart disease
Primary TBI is caused by a direct impact to the brain.
Primary TBI is caused by a direct impact to the brain.
True (A)
Secondary TBI occurs due to the primary injury and can include cerebral swelling, inflammation, and increased intracranial pressure.
Secondary TBI occurs due to the primary injury and can include cerebral swelling, inflammation, and increased intracranial pressure.
Closed trauma, where the dura remains intact, is the most common type of TBI.
Closed trauma, where the dura remains intact, is the most common type of TBI.
What is a coup injury?
What is a coup injury?
What is a contrecoup injury?
What is a contrecoup injury?
A contusion is a bruising within the brain caused by blood leaking from injured vessels.
A contusion is a bruising within the brain caused by blood leaking from injured vessels.
Which of the following is NOT a possible symptom of a contusion?
Which of the following is NOT a possible symptom of a contusion?
Open brain injury occurs when trauma penetrates the dura.
Open brain injury occurs when trauma penetrates the dura.
What is a hematoma?
What is a hematoma?
Where does an epidural hematoma form?
Where does an epidural hematoma form?
A person with an epidural hematoma may become unconscious, have a moment of clarity, and then experience a decreased level of consciousness.
A person with an epidural hematoma may become unconscious, have a moment of clarity, and then experience a decreased level of consciousness.
Subdural hematomas are less common than epidural hematomas and develop slower.
Subdural hematomas are less common than epidural hematomas and develop slower.
Subdural hematomas are always caused by arterial bleeding.
Subdural hematomas are always caused by arterial bleeding.
Diffuse axonal injury (DAI) is a severe brain injury characterized by which of the following?
Diffuse axonal injury (DAI) is a severe brain injury characterized by which of the following?
DAI can only occur with severe brain injury.
DAI can only occur with severe brain injury.
What are the signs of a mild concussion?
What are the signs of a mild concussion?
What are the signs of a classic cerebral concussion?
What are the signs of a classic cerebral concussion?
Which of the following is NOT a complication of TBI?
Which of the following is NOT a complication of TBI?
What is the most common cause of an ischemic stroke?
What is the most common cause of an ischemic stroke?
A thrombotic stroke is caused by a blood clot that forms in the brain.
A thrombotic stroke is caused by a blood clot that forms in the brain.
An embolic stroke is caused by fragments that break from a thrombus formed outside the brain and block an artery.
An embolic stroke is caused by fragments that break from a thrombus formed outside the brain and block an artery.
A lacunar stroke is a type of hemorrhagic stroke.
A lacunar stroke is a type of hemorrhagic stroke.
A hemorrhagic stroke is caused by bleeding in the brain.
A hemorrhagic stroke is caused by bleeding in the brain.
Hypertension can be a cause of hemorrhagic stroke.
Hypertension can be a cause of hemorrhagic stroke.
What is a transient ischemic attack (TIA)?
What is a transient ischemic attack (TIA)?
TIAs are a warning sign for a future stroke.
TIAs are a warning sign for a future stroke.
Increased intracranial pressure (ICP) occurs when the volume of one or more of the intracranial components increases.
Increased intracranial pressure (ICP) occurs when the volume of one or more of the intracranial components increases.
What are the three key components that occupy the intracranial space?
What are the three key components that occupy the intracranial space?
Which of the following is NOT a cause of increased ICP?
Which of the following is NOT a cause of increased ICP?
The Monroe Kellie Doctrine states that because the skull is a rigid structure, any increase in the volume of one component must be offset by a decrease in another to maintain a stable ICP.
The Monroe Kellie Doctrine states that because the skull is a rigid structure, any increase in the volume of one component must be offset by a decrease in another to maintain a stable ICP.
Which of the following is a compensatory mechanism for preventing increased ICP?
Which of the following is a compensatory mechanism for preventing increased ICP?
Cerebral blood flow autoregulation is the brain's ability to adjust its blood flow according to its metabolic needs.
Cerebral blood flow autoregulation is the brain's ability to adjust its blood flow according to its metabolic needs.
An increase in PaCO2 (partial pressure of arterial carbon dioxide) constricts blood vessels and decreases cerebral blood flow.
An increase in PaCO2 (partial pressure of arterial carbon dioxide) constricts blood vessels and decreases cerebral blood flow.
A decrease in PaO2 (partial pressure of arterial oxygen) below 50 mm Hg causes cerebral vasoconstriction.
A decrease in PaO2 (partial pressure of arterial oxygen) below 50 mm Hg causes cerebral vasoconstriction.
Cerebral perfusion pressure (CPP) is the pressure required to ensure sufficient blood flow to the brain.
Cerebral perfusion pressure (CPP) is the pressure required to ensure sufficient blood flow to the brain.
Cerebral edema is an increase in brain tissue fluid content, often resulting from TBI.
Cerebral edema is an increase in brain tissue fluid content, often resulting from TBI.
Which of the following is NOT a type of cerebral edema?
Which of the following is NOT a type of cerebral edema?
Vasogenic edema is the most common type of cerebral edema and is characterized by increased permeability of capillary endothelium.
Vasogenic edema is the most common type of cerebral edema and is characterized by increased permeability of capillary endothelium.
Cytotoxic edema occurs due to cell membrane disruption caused by trauma or lesions that lead to oxygen deprivation and loss of cellular transport systems.
Cytotoxic edema occurs due to cell membrane disruption caused by trauma or lesions that lead to oxygen deprivation and loss of cellular transport systems.
Interstitial edema is primarily observed in hydrocephalus.
Interstitial edema is primarily observed in hydrocephalus.
Pupillary changes can be a sign of increased ICP.
Pupillary changes can be a sign of increased ICP.
Vision changes, such as blurred vision, double vision, and altered extraocular eye movements can occur with increased ICP.
Vision changes, such as blurred vision, double vision, and altered extraocular eye movements can occur with increased ICP.
Motor function impairment, such as hemiparesis or hemiplegia, can be a sign of increased ICP.
Motor function impairment, such as hemiparesis or hemiplegia, can be a sign of increased ICP.
Headache, often projectile and without nausea, can be a sign of increased ICP.
Headache, often projectile and without nausea, can be a sign of increased ICP.
Diagnosis of increased ICP involves the use of CT scans, MRIs, and ICP monitoring in intensive care units.
Diagnosis of increased ICP involves the use of CT scans, MRIs, and ICP monitoring in intensive care units.
Mannitol is an osmotic diuretic that helps draw water from the brain tissue to reduce ICP.
Mannitol is an osmotic diuretic that helps draw water from the brain tissue to reduce ICP.
Corticosteroids are routinely used to decrease vasogenic edema caused by tumors or abscesses in head injuries.
Corticosteroids are routinely used to decrease vasogenic edema caused by tumors or abscesses in head injuries.
Mechanical ventilation may be required to maintain adequate oxygenation and ventilation in patients with TBI.
Mechanical ventilation may be required to maintain adequate oxygenation and ventilation in patients with TBI.
Early initiation of nutrition within five days of TBI has been shown to improve outcomes.
Early initiation of nutrition within five days of TBI has been shown to improve outcomes.
Brain herniation occurs when increased ICP forces brain tissue to shift from its normal position, potentially compressing vital structures.
Brain herniation occurs when increased ICP forces brain tissue to shift from its normal position, potentially compressing vital structures.
Treatment for brain herniation is not an emergency.
Treatment for brain herniation is not an emergency.
Which of the following is NOT a component of the treatment for brain herniation?
Which of the following is NOT a component of the treatment for brain herniation?
Flashcards
Dura Mater
Dura Mater
Outermost layer of the meninges, protecting the brain.
Arachnoid Mater
Arachnoid Mater
Middle layer of the meninges, thin and delicate.
Pia Mater
Pia Mater
Innermost layer of the meninges, connective tissue.
Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI)
Signup and view all the flashcards
Primary TBI
Primary TBI
Signup and view all the flashcards
Secondary TBI
Secondary TBI
Signup and view all the flashcards
Focal Brain Injury
Focal Brain Injury
Signup and view all the flashcards
Diffuse Axonal Injury (DAI)
Diffuse Axonal Injury (DAI)
Signup and view all the flashcards
Coup Injury
Coup Injury
Signup and view all the flashcards
Contrecoup Injury
Contrecoup Injury
Signup and view all the flashcards
Contusion
Contusion
Signup and view all the flashcards
Edema
Edema
Signup and view all the flashcards
Epidural Hematoma
Epidural Hematoma
Signup and view all the flashcards
Subdural Hematoma
Subdural Hematoma
Signup and view all the flashcards
Intracerebral Hemorrhage
Intracerebral Hemorrhage
Signup and view all the flashcards
Mild Concussion
Mild Concussion
Signup and view all the flashcards
Classic Cerebral Concussion
Classic Cerebral Concussion
Signup and view all the flashcards
Increased Intracranial Pressure (ICP)
Increased Intracranial Pressure (ICP)
Signup and view all the flashcards
Monroe-Kellie Doctrine
Monroe-Kellie Doctrine
Signup and view all the flashcards
Cerebral Blood Flow
Cerebral Blood Flow
Signup and view all the flashcards
Cerebral Perfusion Pressure (CPP)
Cerebral Perfusion Pressure (CPP)
Signup and view all the flashcards
Cerebral Edema
Cerebral Edema
Signup and view all the flashcards
Vasogenic Edema
Vasogenic Edema
Signup and view all the flashcards
Cytotoxic Edema
Cytotoxic Edema
Signup and view all the flashcards
Interstitial Edema
Interstitial Edema
Signup and view all the flashcards
Study Notes
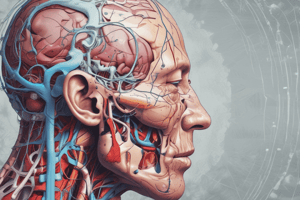
Anatomy of the Brain
- The brain is protected by the skull, cerebrospinal fluid, and three membranes called meninges.
- Dura mater: The outermost layer, tough, fibrous, leather-like tissue.
- Arachnoid mater: The middle protective layer, thin and delicate.
- Pia mater: The innermost layer, made of connective tissue.
Traumatic Brain Injury (TBI)
- TBI is a disruption of the brain's normal function caused by external force.
- It is a common cause of death and disability, especially in Canadians under 40.
- Two types: primary and secondary.
- Primary: Direct impact to the brain. Can be focal (one area) or diffuse (multiple areas).
- Secondary: Results from the primary injury. Examples include cerebral swelling, inflammation, and increased intracranial pressure.
- Focal Brain Injuries: Result from closed (blunt) or open (penetrating) trauma.
- Closed trauma: Most common, dura remains intact. Can cause coup injury (at the impact site) and contrecoup injury (on the opposite side).
- Open brain injury: Trauma penetrates the dura mater (e.g., crush injuries).
Hematomas
- Hematomas are collections of blood within the skull.
- Epidural hematoma: Blood collects between the skull and the dura mater.
- Often caused by arterial bleeding, an emergency needing rapid surgical intervention.
- Subdural hematoma: Blood collects between the arachnoid and pia mater.
- Often venous, develops more slowly.
- Epidural hematoma: Blood collects between the skull and the dura mater.
Other Brain Injuries
- Acute subdural hematomas occur within 48 hours of injury.
- Subacute subdural hematomas occur 2-14 days after injury.
- Chronic subdural hematomas occur weeks or months after injury.
- Intracerebral hemorrhage: Bleeding within the brain tissue.
- Often associated with contusions. Occurs in 2-3% of persons with head injuries. Can lead to increased intracranial pressure and cerebral edema.
- Diffuse Axonal Injury (DAI): Widespread axonal injury (shearing, tearing, or stretching of nerve fibers), often in severe brain injuries. Results from mild, moderate, or severe brain injury (12-24 hours post-injury). Signs include decreased level of consciousness, increased intracranial pressure, and cerebral edema.
Classifications of DAI
- Mild concussion
- Mild but immediate clinical manifestations, CSF pressure rises, EEG/ECG changes.
- Glasgow Coma Scale (GCS) score of 13-15.
- Confusion lasting 1-several minutes with amnesia, headache and nervousness a few days later.
- Classic cerebral concussion
- Loss of consciousness (LOC) less than 6 hours with amnesia, confusion, transient cessation of respiration, and vital signs stabilizing within minutes.
Cerebral Vascular Disorders (Stroke)
- Ischemic stroke: Blockage of blood flow to the brain.
- Thrombotic: Blood clot forming in the artery supplying the brain.
- Embolic: Blood clot breaking away from another part of the body and blocking a brain artery.
- Lacunar: Occlusion of a deep perforating artery, causing ischemic lesions.
- Hemorrhagic stroke: Bleeding in the brain.
- Hypertension is the main cause.
- Can lead to cerebral edema and increased intracranial pressure (ICP).
Transient Ischemic Attacks (TIAs)
- TIAs are brief episodes of neurological dysfunction (less than an hour) due to an ischemic event.
- Considered warning signs for future strokes (within 90 days).
Increased Intracranial Pressure (ICP)
- The intracranial space (brain tissue, blood, CSF) is enclosed.
- Any increase in one component can lead to increased ICP.
- Various conditions like cerebral neoplasms (tumors), contusions, abscesses, cerebral edema, hematomas, hemorrhages, metabolic and physiological factors and vascular anomalies can lead to increased intracranial pressure.
Compensatory Mechanisms
- The body employs mechanisms to prevent elevated ICP. Includes CSF volume compensation, blood volume compensation, and brain tissue compensation.
Cerebral Blood Flow and Autoregulation
- The brain needs consistent oxygen and glucose supply. Autoregulation is the brain's ability to change blood vessel diameter for maintaining consistent blood flow even with blood pressure changes.
Cerebral Edema
- Increased fluid content in the brain's tissues.
- Vasogenic: Increased permeability of capillaries allows plasma proteins to leak into extra-cellular space (fluid accumulation).
- Cytotoxic: Cellular swelling due to oxygen deprivation and dysfunction.
- Interstitial: Due to fluid buildup in extracellular spaces, usually seen in hydrocephalus.
Clinical Manifestations of Increased ICP
- Various changes, including sluggish or fixed pupils, blurred/double vision, and motor function impairment, headache, and vomiting.
Diagnosis and Management of Increased ICP
- Diagnosis involves CT scans, MRIs, and ICP monitoring.
- Management strategies include ICP monitoring, surgical intervention (e.g., mass removal, hematoma evacuation), osmotic diuretics (mannitol), and steroids.
Brain Herniation
- Increased ICP force brain tissue to shift inappropriately, putting pressure on vital structures, especially the brainstem.
- A life-threatening emergency.
Treatment for Herniation
- Immediate interventions such as CSF drainage, steroid administration, mannitol, intubation, and sometimes surgery (removal of part of the skull or brain tissue).
Additional Notes
- Nutritional therapy may be critical in treating TBI, as early initiation of nutrition can improve outcomes.
- Mechanical ventilation may be necessary to support breathing and oxygenation in severe cases of brain injury.
- Corticosteroids can decrease vasogenic edema but not routinely used in head injuries.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the protective structures of the brain, including the meninges and the impact of traumatic brain injury (TBI). This quiz delves into the types of TBI and their effects on brain function. Understand the differences between primary and secondary injuries, as well as focal brain injuries.