Podcast
Questions and Answers
What percentage of traumatic brain injuries are caused by transportation?
What percentage of traumatic brain injuries are caused by transportation?
- 8%
- 26%
- 44% (correct)
- 13%
What is the primary function of the Monro-Kellie Doctrine?
What is the primary function of the Monro-Kellie Doctrine?
- To illustrate the relationship between venous and arterial volume in the brain (correct)
- To describe the anatomy of the brain
- To explain the pathophysiology of primary brain injury
- To diagnose secondary brain injury
What is the annual mortality rate of children from road traffic accidents (RTC) per 100,000 in South Africa?
What is the annual mortality rate of children from road traffic accidents (RTC) per 100,000 in South Africa?
- 5.89 per 100,000
- 7.89 per 100,000
- 1.89 per 100,000
- 3.89 per 100,000 (correct)
What is the definition of traumatic brain injury?
What is the definition of traumatic brain injury?
What percentage of traumatic brain injuries are caused by firearms?
What percentage of traumatic brain injuries are caused by firearms?
What is the primary layer of protection for the brain?
What is the primary layer of protection for the brain?
What is the volume of the brain's CSF?
What is the volume of the brain's CSF?
What is the point of decompensation in the Volume-Pressure Curve?
What is the point of decompensation in the Volume-Pressure Curve?
What is the total Glasgow Coma Scale (GCS) of a 20-year-old male in MVA?
What is the total Glasgow Coma Scale (GCS) of a 20-year-old male in MVA?
What is an indication for a CT scan in a head injury patient?
What is an indication for a CT scan in a head injury patient?
What is a common indication for re-admission in head injury patients?
What is a common indication for re-admission in head injury patients?
What is a sign of skull base fracture?
What is a sign of skull base fracture?
What is the target value for cerebral perfusion pressure?
What is the target value for cerebral perfusion pressure?
When is a skull X-ray useful in a trauma setting?
When is a skull X-ray useful in a trauma setting?
What is the primary goal of ICP management steps?
What is the primary goal of ICP management steps?
What is an indication for observation at home?
What is an indication for observation at home?
What is not an indication for a CT scan in a head injury patient?
What is not an indication for a CT scan in a head injury patient?
What is the normal value for brain tissue oxygen tension?
What is the normal value for brain tissue oxygen tension?
What is the target value for partial pressure of oxygen in the arterial blood?
What is the target value for partial pressure of oxygen in the arterial blood?
What is a contraindication for conservative management?
What is a contraindication for conservative management?
What is a prognostic factor that increases mortality?
What is a prognostic factor that increases mortality?
What is a part of general monitoring in ICU?
What is a part of general monitoring in ICU?
What is the cutoff for severe head injury based on the Glasgow Coma Scale?
What is the cutoff for severe head injury based on the Glasgow Coma Scale?
What is the primary goal of operative and non-operative strategies in managing head injuries?
What is the primary goal of operative and non-operative strategies in managing head injuries?
What is the most common complication of hypotension in patients with head injuries?
What is the most common complication of hypotension in patients with head injuries?
What is the definition of hypoxia in the context of head injuries?
What is the definition of hypoxia in the context of head injuries?
Which of the following is a member of the multidisciplinary team that manages patients with head injuries?
Which of the following is a member of the multidisciplinary team that manages patients with head injuries?
What is the term for a Glasgow Outcome Scale score of 1?
What is the term for a Glasgow Outcome Scale score of 1?
Flashcards are hidden until you start studying
Study Notes
Head Injury
- Traumatic brain injury is an insult to the brain caused by an external physical force, resulting in a diminished or altered state of consciousness and impairment of cognitive abilities or physical functioning.
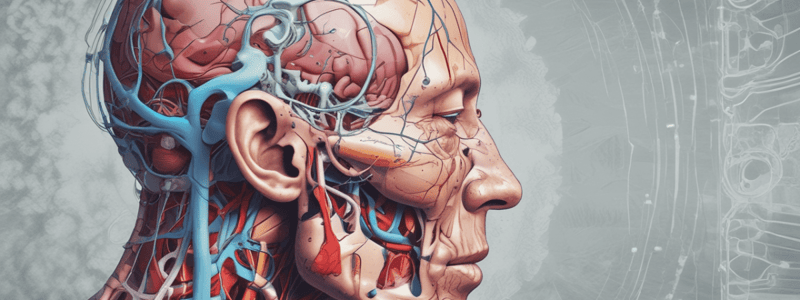
Anatomy
- Scalp
- Skull
- Brain
Epidemiology
- Transportation accounts for 44% of traumatic brain injuries
- Falls account for 26% of traumatic brain injuries
- Other causes include: • Firearms (8%) • Non-firearm assaults (9%) • Annual mortality of children from road traffic accidents is 3.89 per 100,000
Pathophysiology
- Primary vs secondary brain injury
- Monro-Kellie doctrine: the concept of a fixed volume of the cranial vault, where an increase in one component (blood, CSF, or brain tissue) leads to a decrease in another
Concepts
- Autoregulation
- Volume-pressure curve: • 60-55 mmHg: herniation • 50-40 mmHg: point of decompensation • 30-20 mmHg: compensation • 15-10 mmHg: volume of mass
Classification of Head Injury
- Glasgow Coma Scale (GCS): • Eye opening: 1-4 points • Verbal response: 1-5 points • Motor response: 1-6 points • Total GCS: 3-15 points
- Clinical scenario: a 20-year-old male in a motor vehicle accident, intubated, with a GCS score of 8
Approach to Head Injury
- History: • Mechanism of injury • Loss of consciousness • Vomiting • Seizures • Intoxicants • Post-traumatic amnesia
- Clinical examination: • Dilated non-reactive pupils • Hemiplegia/hemiparesis • Aphasia/dysphasia • Facial weakness • Cranial nerve palsy • Papilloedema
- Signs of skull base fracture: • Raccoon eyes • Battle sign
Investigations
- Skull X-ray: useful only for detecting skull fractures, but may waste time in the trauma setting
- CT scan:
• Indications:
- GCS ≤ 14
- Focal neurological deficits
- Deteriorating GCS
- Penetrating head injuries
- Post-traumatic seizures
- Loss of consciousness and amnesia
- Multiple trauma
- Skull fracture
- Patients who are intoxicated
- Patients on anti-coagulant therapy
- Mechanism of injury • Indications for observation at home:
- Normal CT
- GCS 15
- No focal deficits
- Easy access to ER
- Responsible adult to observe at home
- No complicating circumstances • Indications for re-admission:
- Drowsiness
- CSF leak
- Seizures
- New focal deficit
- Fever
Pathology
- Primary injury: • Acute extradural hematoma • Acute subdural hematoma • Contusion/intracerebral hematoma • Diffuse cerebral injury • Skull fracture • Gunshot injuries • Penetrating stab injuries • Concussion in sports • Non-accidental injury
- Secondary brain injury:
• Prevention: maintain Po2 > 60 mmHg, systolic BP > 90 mmHg, glucose control, and appropriate IV fluids
• Conservative management:
- GCS 13-15
- No focal deficits
- Neurological observations: ICU/high care (hourly) • Surgical management:
- ICU management:
- General measures:
- Head elevation 30 degrees
- Neck neutral position
- Urinary catheter
- Analgesia
- Gastro-protective agents
- Anti-seizure prophylaxis
- DVT prophylaxis
- Nutrition
- Fluids
- Medical management:
- Ventilation: PCo2 30-35 mmHg
- Sedation
- Mannitol
- Hypertonic saline
- General monitoring:
- ECG
- Saturations: 100%
- Systolic BP: > 90 mmHg
- Pulse
- Temperature: maintain euthermia or mild hypothermia
- CVP: 8-14 mmHg
- Glucose: normoglycemic
- ICP monitoring:
- Indications:
- GCS ≤ 8
- Polytrauma
- Prolonged ventilation
- Hypotension
- Posturing
- ICP > 20 mmHg: abnormal
- Indications:
- Brain tissue oxygen tension (PbtO2) monitoring:
- Normal values: 20-35 mmHg
- Cerebral perfusion pressure (CPP):
- CPP = MAP – ICP
- Targeted value: 60 mmHg
- Values < 50 mmHg: cerebral ischemia and hypo-perfusion
- Values > 70 mmHg: cardiorespiratory failure, ARDS
- General measures:
Prognostic Factors
- Age: younger patients have a greater potential for survival and recovery
- Mechanism of injury: e.g., motorbike crashes
- GCS < 8
- ICP > 45
- Hypotension: > 50% increase in mortality with a single episode of hypotension
- Hypoxia: PO2 < 60 mmHg, Sats < 90%
Glasgow Outcome Scale
- 1: Dead
- 2: Vegetative state
- 3: Severe disability
- 4: Moderate disability
- 5: Mild disability
Late Complications
- Post-traumatic seizures
- Hydrocephalus
- Infections
- Post-concussive syndrome: • Somatic: headaches, dizziness, anosmia, hearing difficulties, balance difficulties • Cognitive: difficulty concentrating, dementia, impaired judgment • Psychosocial: emotional problems, personality changes, loss of libido, tiredness, difficulty sleeping
Multidisciplinary Team
- Physiotherapists
- Occupational therapists
- Psychologists
- Social workers
- Nurses
- Doctors
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.