Podcast
Questions and Answers
What is the primary function of the gallbladder?
What is the primary function of the gallbladder?
The gallbladder stores and concentrates bile.
Which of the following is NOT a component of the biliary system?
Which of the following is NOT a component of the biliary system?
- Gallbladder
- Common bile duct
- Small intestine (correct)
- Cystic duct
The gallbladder is located in the left upper quadrant of the abdomen.
The gallbladder is located in the left upper quadrant of the abdomen.
False (B)
What is the normal range for gallbladder diameter?
What is the normal range for gallbladder diameter?
Which layer of the gallbladder wall is responsible for muscle contractions?
Which layer of the gallbladder wall is responsible for muscle contractions?
Bile production is increased during digestion.
Bile production is increased during digestion.
What is the name of the main pancreatic duct?
What is the name of the main pancreatic duct?
The pancreas is a retroperitoneal organ.
The pancreas is a retroperitoneal organ.
Which of the following is a function of the pancreas?
Which of the following is a function of the pancreas?
The uncinate process of the pancreas is located anterior to the inferior vena cava.
The uncinate process of the pancreas is located anterior to the inferior vena cava.
What is the name of the junction where the splenic vein and superior mesenteric vein join?
What is the name of the junction where the splenic vein and superior mesenteric vein join?
Which of the following is a characteristic of the jejunum?
Which of the following is a characteristic of the jejunum?
Peyer's patches are found in the jejunum.
Peyer's patches are found in the jejunum.
What is the primary function of the ileocecal valve?
What is the primary function of the ileocecal valve?
The appendix is located in the left iliac fossa.
The appendix is located in the left iliac fossa.
Which of the following is NOT a recognized anatomical segment of the large intestine?
Which of the following is NOT a recognized anatomical segment of the large intestine?
What is the name of the condition where the head and part of the body of the pancreas are found intraperitoneally?
What is the name of the condition where the head and part of the body of the pancreas are found intraperitoneally?
The upper GI tract is defined as the portion from the mouth to the duodenum.
The upper GI tract is defined as the portion from the mouth to the duodenum.
Which of the following statements is TRUE regarding the pyloric antrum?
Which of the following statements is TRUE regarding the pyloric antrum?
What is the primary function of the lower esophageal sphincter?
What is the primary function of the lower esophageal sphincter?
The jejunum is the primary site for nutrient absorption in the small intestine.
The jejunum is the primary site for nutrient absorption in the small intestine.
The rectum is characterized by the presence of haustra.
The rectum is characterized by the presence of haustra.
What is the primary purpose of a transabdominal technique in ultrasound imaging?
What is the primary purpose of a transabdominal technique in ultrasound imaging?
Which of the following imaging techniques is considered the gold standard for evaluating the pancreas?
Which of the following imaging techniques is considered the gold standard for evaluating the pancreas?
Water loading is a common preparation for upper GI ultrasound procedures.
Water loading is a common preparation for upper GI ultrasound procedures.
What is the term for the outermost layer of the GI tract?
What is the term for the outermost layer of the GI tract?
Which layer of the GI tract wall is responsible for muscle contractions that propel food through the digestive system?
Which layer of the GI tract wall is responsible for muscle contractions that propel food through the digestive system?
The presence of a vascular network in the submucosa is considered a normal finding.
The presence of a vascular network in the submucosa is considered a normal finding.
What is a common indication for performing an ultrasound examination of the pancreas?
What is a common indication for performing an ultrasound examination of the pancreas?
Which of the following is NOT a typical sonographic characteristic of the splenic vein?
Which of the following is NOT a typical sonographic characteristic of the splenic vein?
A hyperechoic pancreas is more likely to be observed in children compared to adults.
A hyperechoic pancreas is more likely to be observed in children compared to adults.
What is the term for the abnormal condition where the ducts of Wirsung and Santorini fail to fuse?
What is the term for the abnormal condition where the ducts of Wirsung and Santorini fail to fuse?
Which of the following is a common location for ectopic pancreatic tissue?
Which of the following is a common location for ectopic pancreatic tissue?
A well-defined, hyperechoic rim around a gallbladder wall is a normal finding.
A well-defined, hyperechoic rim around a gallbladder wall is a normal finding.
What is the technical term for the condition where a thin band of pancreatic tissue surrounds the second part of the duodenum?
What is the technical term for the condition where a thin band of pancreatic tissue surrounds the second part of the duodenum?
Pancreatic tissue present in the wall of the gallbladder is known as a pancreatic cyst.
Pancreatic tissue present in the wall of the gallbladder is known as a pancreatic cyst.
Which of the following is a common indication for performing an ultrasound examination of the gallbladder?
Which of the following is a common indication for performing an ultrasound examination of the gallbladder?
A Phrygian cap is considered a common anatomical variation of the gallbladder.
A Phrygian cap is considered a common anatomical variation of the gallbladder.
What is the term for the fold at the neck of the gallbladder, which is a common site for stone collection?
What is the term for the fold at the neck of the gallbladder, which is a common site for stone collection?
Which of the following is a sign of a postprandial state on an ultrasound examination of the gallbladder?
Which of the following is a sign of a postprandial state on an ultrasound examination of the gallbladder?
A normal gallbladder wall thickness measurement is considered to be less than 3mm.
A normal gallbladder wall thickness measurement is considered to be less than 3mm.
What is the name of the duct that joins the cystic duct to form the common bile duct?
What is the name of the duct that joins the cystic duct to form the common bile duct?
An endoluminal ultrasound examination requires access to the GI tract through an endoscope.
An endoluminal ultrasound examination requires access to the GI tract through an endoscope.
Which of the following is a common reason for performing an endoluminal ultrasound examination of the GI tract?
Which of the following is a common reason for performing an endoluminal ultrasound examination of the GI tract?
Flashcards
Gallbladder length
Gallbladder length
7-10 cm in length, where bile is stored.
Gallbladder diameter
Gallbladder diameter
2.5-4 cm in diameter, varies with filling.
Gallbladder wall thickness
Gallbladder wall thickness
Should be ≤3 mm thick in health.
Common Bile Duct diameter
Common Bile Duct diameter
Signup and view all the flashcards
Bile production
Bile production
Signup and view all the flashcards
Bile composition
Bile composition
Signup and view all the flashcards
Intraperitoneal organ
Intraperitoneal organ
Signup and view all the flashcards
Gallbladder function
Gallbladder function
Signup and view all the flashcards
Ultrasound preparation
Ultrasound preparation
Signup and view all the flashcards
Segmentation of small intestine
Segmentation of small intestine
Signup and view all the flashcards
Uncinate process
Uncinate process
Signup and view all the flashcards
Endocrine pancreas function
Endocrine pancreas function
Signup and view all the flashcards
Exocrine pancreas function
Exocrine pancreas function
Signup and view all the flashcards
Main pancreatic duct
Main pancreatic duct
Signup and view all the flashcards
Celiac axis
Celiac axis
Signup and view all the flashcards
Superior mesenteric artery
Superior mesenteric artery
Signup and view all the flashcards
Major duodenal papilla
Major duodenal papilla
Signup and view all the flashcards
Pylorus function
Pylorus function
Signup and view all the flashcards
Halves of the stomach
Halves of the stomach
Signup and view all the flashcards
Ascending colon
Ascending colon
Signup and view all the flashcards
Sigmoid colon
Sigmoid colon
Signup and view all the flashcards
Echogenic appearance
Echogenic appearance
Signup and view all the flashcards
Hypoechoic layer
Hypoechoic layer
Signup and view all the flashcards
Compressibility evaluation
Compressibility evaluation
Signup and view all the flashcards
Water technique
Water technique
Signup and view all the flashcards
Pathological indicators
Pathological indicators
Signup and view all the flashcards
Sonographic differentiation
Sonographic differentiation
Signup and view all the flashcards
Advanced imaging consideration
Advanced imaging consideration
Signup and view all the flashcards
Ectopic pancreas
Ectopic pancreas
Signup and view all the flashcards
Congenital pancreas divisum
Congenital pancreas divisum
Signup and view all the flashcards
Pancreatic gallbladder
Pancreatic gallbladder
Signup and view all the flashcards
Study Notes
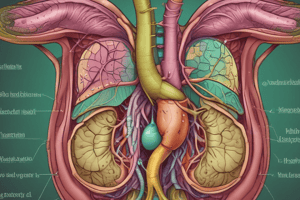
Anatomy of the Biliary System
- The biliary system comprises the liver, gallbladder, and bile ducts.
- The liver produces bile, a fluid containing water, electrolytes, bile salts, lipids, and pigments. Daily production is 500-1000 mL.
- Bile is transported through the hepatic ducts (right and left), then into the common hepatic duct. The cystic duct joins with the common hepatic duct to form the common bile duct.
- Approximately 50% of the bile is stored in the gallbladder.
- The gallbladder concentrates and stores bile, releasing it into the duodenum during digestion.
Gallbladder Anatomy
- The gallbladder is a pear-shaped organ located in the gallbladder fossa on the posterior surface of the right lobe of the liver.
- Its parts include the fundus, body, and neck, with the neck connecting to the cystic duct.
- The gallbladder wall consists of three layers: mucosa, fibromuscular layer, and serosal layer.
- Normal gallbladder length is 7-10 cm, diameter is 2.5-4 cm, and wall thickness is less than 3mm.
Bile Duct Classification
- Intrahepatic ducts are within the liver.
- Extrahepatic ducts include the common bile duct, cystic duct, and part of the common hepatic duct.
Gallbladder Functions
- Bile aids in the digestion and absorption of lipids and fat-soluble vitamins, and eliminates waste products within the small intestine.
- Bile neutralizes gastric acid.
- The gallbladder concentrates and stores bile.
Ultrasound Examination
- Patient preparation involves an 8-12 hour fast.
- Patient positioning usually involves a supine or left lateral decubitus position.
- A 5 MHz or higher frequency transducer is often used.
- Morning scans are often preferred.
- Ultrasound is used to assess the gallbladder for possible abnormalities.
Normal Variants and Variations
- Junctional fold is a common anatomical variant.
- Hartmann's pouch is a fold at the neck of the gallbladder, a common site for stone collection.
- Phrygian cap is a folding of the gallbladder fundus.
- Septated gallbladder can be partial or complete.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.