Podcast
Questions and Answers
What is the typical thickness of the gallbladder wall in millimeters?
What is the typical thickness of the gallbladder wall in millimeters?
- 5 - 7 mm
- 3 - 4 mm
- 1 - 2 mm (correct)
- 8 - 10 mm
Which of the following is the correct sequence of structures in the extrahepatic biliary tree, starting from the liver?
Which of the following is the correct sequence of structures in the extrahepatic biliary tree, starting from the liver?
- Right and left hepatic ducts → common hepatic duct → cystic duct → common bile duct (correct)
- Cystic duct → common hepatic duct → right and left hepatic ducts → common bile duct
- Common bile duct → cystic duct → common hepatic duct → right and left hepatic ducts
- Right and left hepatic ducts → cystic duct → common hepatic duct → common bile duct
What is the primary function of bile salts in the context of intestinal absorption?
What is the primary function of bile salts in the context of intestinal absorption?
- To solubilize water-insoluble lipids, promoting dietary lipid absorption. (correct)
- To directly break down dietary fats into smaller molecules.
- To neutralize stomach acid in the duodenum.
- To act as a barrier preventing absorption of water insoluble lipids.
What percentage of secreted bile salts are typically reabsorbed in the ileum and returned to the liver?
What percentage of secreted bile salts are typically reabsorbed in the ileum and returned to the liver?
Lecithin (phosphatidylcholine), a component of bile is known for which of the following properties?
Lecithin (phosphatidylcholine), a component of bile is known for which of the following properties?
Which of the following conditions is a complication directly associated with cholelithiasis?
Which of the following conditions is a complication directly associated with cholelithiasis?
Which of the following chemical components is most commonly found in gallstones?
Which of the following chemical components is most commonly found in gallstones?
What is a primary mechanism leading to the formation of cholesterol gallstones?
What is a primary mechanism leading to the formation of cholesterol gallstones?
Which of the following factors is directly associated with decreased bile acid secretion, potentially leading to gallstone formation?
Which of the following factors is directly associated with decreased bile acid secretion, potentially leading to gallstone formation?
Which condition is often an incidental finding following a cholecystectomy and presents as yellow streaks of cholesterol deposits on the gallbladder mucosa?
Which condition is often an incidental finding following a cholecystectomy and presents as yellow streaks of cholesterol deposits on the gallbladder mucosa?
Which of the following processes describes why cholesterol is described as insoluble?
Which of the following processes describes why cholesterol is described as insoluble?
The MOST important step in the pathogenesis of gallbladder stones is:
The MOST important step in the pathogenesis of gallbladder stones is:
Cholecystectomy may be curative for acute cholecystitis within how many hours?
Cholecystectomy may be curative for acute cholecystitis within how many hours?
In cases of calculous acute cholecystitis, what directly initiates the pathological process?
In cases of calculous acute cholecystitis, what directly initiates the pathological process?
Bile stasis and ischemia are factors in acute acalculous cholecystitis, however they are NOT provoked by:
Bile stasis and ischemia are factors in acute acalculous cholecystitis, however they are NOT provoked by:
What is a common gross morphological feature observed in the gallbladder during acute cholecystitis?
What is a common gross morphological feature observed in the gallbladder during acute cholecystitis?
Gallstones can cause what complication?
Gallstones can cause what complication?
Chronic inflammation of the gallbladder is most commonly a result of:
Chronic inflammation of the gallbladder is most commonly a result of:
Which part of the pancreas is closest to the superior mesenteric artery and portal vein?
Which part of the pancreas is closest to the superior mesenteric artery and portal vein?
What is the primary substance produced by the exocrine pancreas?
What is the primary substance produced by the exocrine pancreas?
Which digestive enzyme is responsible for activating other enzymes?
Which digestive enzyme is responsible for activating other enzymes?
Which zones is the pancreas divided?
Which zones is the pancreas divided?
In which of the following conditions affecting the pancreas, are fat necrosis and hemorrhage key findings?
In which of the following conditions affecting the pancreas, are fat necrosis and hemorrhage key findings?
What is the MOST common cause of acute pancreatitis?
What is the MOST common cause of acute pancreatitis?
Late sequelae of acute pancreatitis is:
Late sequelae of acute pancreatitis is:
What term describes a pancreatic condition histologically characterized by parenchymal fibrosis and atrophy?
What term describes a pancreatic condition histologically characterized by parenchymal fibrosis and atrophy?
Which form of pancreatitis is associated with mutations from PRSS1 and CFTR?
Which form of pancreatitis is associated with mutations from PRSS1 and CFTR?
Severe abdominal pain, steatorrhea and weight loss is MOST associated with:
Severe abdominal pain, steatorrhea and weight loss is MOST associated with:
Which of the following describes Duct Adenocarcinoma?
Which of the following describes Duct Adenocarcinoma?
A pancreatic tumor arising from endocrine cells would be characterized as what type of tumor?
A pancreatic tumor arising from endocrine cells would be characterized as what type of tumor?
What is the prognosis for Exocrine Pancreas: Ductal adenocarcinoma?
What is the prognosis for Exocrine Pancreas: Ductal adenocarcinoma?
Hepatocellular carcinoma comprises what percentage of primary malignant liver tumors?
Hepatocellular carcinoma comprises what percentage of primary malignant liver tumors?
Malignancies arising from the biliary tree (epithelial derived) are classified as:
Malignancies arising from the biliary tree (epithelial derived) are classified as:
What is the MOST common malignant tumor in the liver?
What is the MOST common malignant tumor in the liver?
Focal Nodular Hyperplasia is often associated with what class of drug?
Focal Nodular Hyperplasia is often associated with what class of drug?
Which type of liver tumor is characterized by well circumscribed red brown lesion with blood vessels?
Which type of liver tumor is characterized by well circumscribed red brown lesion with blood vessels?
Which of the following liver conditions is usually subcapsular, and may be pedunculated with a risk of rupture/abdominal bleeding?
Which of the following liver conditions is usually subcapsular, and may be pedunculated with a risk of rupture/abdominal bleeding?
Which of the following components is MOST associated with gallstone formation?
Which of the following components is MOST associated with gallstone formation?
A patient is diagnosed with cholelithiasis. Which of the following factors is LEAST likely to be associated with their condition?
A patient is diagnosed with cholelithiasis. Which of the following factors is LEAST likely to be associated with their condition?
Which of the following is a potential complication of gallstones located in the common bile duct?
Which of the following is a potential complication of gallstones located in the common bile duct?
Which of the following best describes the cause of acute acalculous cholecystitis?
Which of the following best describes the cause of acute acalculous cholecystitis?
Which of the following features is typically observed during gross examination of a gallbladder with acute cholecystitis?
Which of the following features is typically observed during gross examination of a gallbladder with acute cholecystitis?
Long-standing inflammation of the gallbladder is MOST often associated with what condition?
Long-standing inflammation of the gallbladder is MOST often associated with what condition?
According to the content provided, what percentage of chronic cholecystitis cases are associated with stones?
According to the content provided, what percentage of chronic cholecystitis cases are associated with stones?
What is the MOST likely cause of acute pancreatitis in a patient with a history of chronic alcohol abuse who presents with severe abdominal pain?
What is the MOST likely cause of acute pancreatitis in a patient with a history of chronic alcohol abuse who presents with severe abdominal pain?
A patient with severe epigastric pain is diagnosed with acute pancreatitis. Which of the following signs is MOST indicative of a late sequelae?
A patient with severe epigastric pain is diagnosed with acute pancreatitis. Which of the following signs is MOST indicative of a late sequelae?
Which of the following histological findings is MOST associated with chronic pancreatitis?
Which of the following histological findings is MOST associated with chronic pancreatitis?
If a pancreatic duct empties into common bile duct instead of directly into the ampulla, what can this cause?
If a pancreatic duct empties into common bile duct instead of directly into the ampulla, what can this cause?
Bicarbonate and a lot of enzymes are contained in what?
Bicarbonate and a lot of enzymes are contained in what?
Pancreatic ductal adenocarcinoma is derived from what cells?
Pancreatic ductal adenocarcinoma is derived from what cells?
Which of these is a risk factor for pancreatic ductal adenocarcinoma?
Which of these is a risk factor for pancreatic ductal adenocarcinoma?
Which of the following is the MOST common location of pancreatic ductal adenocarcinoma?
Which of the following is the MOST common location of pancreatic ductal adenocarcinoma?
In the context of pancreatic tumors, what is a PanNET?
In the context of pancreatic tumors, what is a PanNET?
Which of the following characteristics is MOST likely associated with a pancreatic neuroendocrine tumor (PanNET)?
Which of the following characteristics is MOST likely associated with a pancreatic neuroendocrine tumor (PanNET)?
Which of the following best describes hilar cholangiocarcinoma?
Which of the following best describes hilar cholangiocarcinoma?
What is a key difference between fibrolamellar HCC and the more common forms of HCC?
What is a key difference between fibrolamellar HCC and the more common forms of HCC?
A patient presents with multiple liver tumors. What is the MOST likely type of malignant liver lesion?
A patient presents with multiple liver tumors. What is the MOST likely type of malignant liver lesion?
Where are well circumscribed red brown lesions with blood vessels, most likely?
Where are well circumscribed red brown lesions with blood vessels, most likely?
A patient's imaging reveals a benign liver lesion with a central scar. Which of the following conditions is MOST likely?
A patient's imaging reveals a benign liver lesion with a central scar. Which of the following conditions is MOST likely?
A patient has enlarged liver lesions and reports vague symptoms, what can this be attributed to?
A patient has enlarged liver lesions and reports vague symptoms, what can this be attributed to?
A patient's liver biopsy shows granular cytoplasm, what can this be attributed to?
A patient's liver biopsy shows granular cytoplasm, what can this be attributed to?
Trypsin catalyzes activation of what enzymes?
Trypsin catalyzes activation of what enzymes?
With liver cell adenoma, what is a potential consequence of this?
With liver cell adenoma, what is a potential consequence of this?
If an individual has firm fibrosis, small in size, stones, and loss of glands, what is this a key finding of?
If an individual has firm fibrosis, small in size, stones, and loss of glands, what is this a key finding of?
What is the treatment regarding acute pancreatitis?
What is the treatment regarding acute pancreatitis?
A patient liver panel comes back with 90% of the 1 degree malignant tumor. What does this mean?
A patient liver panel comes back with 90% of the 1 degree malignant tumor. What does this mean?
Which of the following does NOT occur in the pancreas
Which of the following does NOT occur in the pancreas
Which location relates to the pancreas divided into the head, body and tail
Which location relates to the pancreas divided into the head, body and tail
A patient's liver panel returns and the doctors discovered it has metastatic liver, what is this composed of?
A patient's liver panel returns and the doctors discovered it has metastatic liver, what is this composed of?
Autoimmune causes what diseases
Autoimmune causes what diseases
In Cholangiocarcinoma, what do the doctors look for first?
In Cholangiocarcinoma, what do the doctors look for first?
What causes Cholestasis?
What causes Cholestasis?
In metabolic liver disease, what can a patient receive
In metabolic liver disease, what can a patient receive
What is the origin of all pancreatic neuroendocrine
What is the origin of all pancreatic neuroendocrine
Which one is found on the Livers
Which one is found on the Livers
Which of the following findings is more related to malignant behavior
Which of the following findings is more related to malignant behavior
Which of the following is the correct order of the gallbladder's anatomical regions, starting from the most distal point?
Which of the following is the correct order of the gallbladder's anatomical regions, starting from the most distal point?
A patient's gallbladder is surgically removed. Which duct directly conducts bile from the gallbladder?
A patient's gallbladder is surgically removed. Which duct directly conducts bile from the gallbladder?
What is the MOST critical role of cholecystokinin (CCK) in gallbladder function?
What is the MOST critical role of cholecystokinin (CCK) in gallbladder function?
A patient's ileum is damaged, impairing its normal function. How does this MOST directly affect bile salt circulation?
A patient's ileum is damaged, impairing its normal function. How does this MOST directly affect bile salt circulation?
What is the primary function of lecithin in bile that aids in the digestion process?
What is the primary function of lecithin in bile that aids in the digestion process?
What condition arises when gallstones obstruct the cystic duct, leading to inflammation?
What condition arises when gallstones obstruct the cystic duct, leading to inflammation?
What is an early pathological event in the formation of cholesterol gallstones?
What is an early pathological event in the formation of cholesterol gallstones?
Which factor is MOST likely to contribute to decreased bile acid secretion?
Which factor is MOST likely to contribute to decreased bile acid secretion?
In acute cholecystitis, what event directly precipitates gallbladder ischemia and necrosis?
In acute cholecystitis, what event directly precipitates gallbladder ischemia and necrosis?
Predict what key components should be identified in the gross examination of acute cholecystitis?
Predict what key components should be identified in the gross examination of acute cholecystitis?
A patient with a history of gallstones presents with recurrent episodes of RUQ pain after meals. What is the MOST likely diagnosis?
A patient with a history of gallstones presents with recurrent episodes of RUQ pain after meals. What is the MOST likely diagnosis?
Which of the following locations is part of the normal anatomy of the pancreas?
Which of the following locations is part of the normal anatomy of the pancreas?
What condition may result from abnormalities where the pancreatic duct empties into the common bile duct instead of directly into the ampulla?
What condition may result from abnormalities where the pancreatic duct empties into the common bile duct instead of directly into the ampulla?
What is the expected outcome regarding most pancreatic tumors?
What is the expected outcome regarding most pancreatic tumors?
What is the MOST likely consequence of the pancreas releasing trypsinogen in the pancreas?
What is the MOST likely consequence of the pancreas releasing trypsinogen in the pancreas?
What liver condition is associated with the use of anabolic steroids?
What liver condition is associated with the use of anabolic steroids?
A pathological report of the liver shows well circumscribed red brown lesion with blood vessels, what condition could this be?
A pathological report of the liver shows well circumscribed red brown lesion with blood vessels, what condition could this be?
If there are several tumors in the Liver panel, what condition can this be?
If there are several tumors in the Liver panel, what condition can this be?
What is the difference in patients with Hepatocelluar Carcinoma?
What is the difference in patients with Hepatocelluar Carcinoma?
What tissue is being referred to about malignancies arising from the biliary tree (epithelial derived)?
What tissue is being referred to about malignancies arising from the biliary tree (epithelial derived)?
Flashcards
What function does the gallbladder perform?
What function does the gallbladder perform?
Stores and releases bile, emptying into the cystic duct.
What are the main parts of the gallbladder?
What are the main parts of the gallbladder?
Fundus, body and neck. Wall is 1-2 mm thick.
What is the role of the cystic duct?
What is the role of the cystic duct?
Connects gallbladder to common hepatic duct (CHD).
What happens to most of secreted bile salts?
What happens to most of secreted bile salts?
Signup and view all the flashcards
What are the key components of bile salts?
What are the key components of bile salts?
Signup and view all the flashcards
What is the main component of cholesterol stones?
What is the main component of cholesterol stones?
Signup and view all the flashcards
What are the main mechanisms of forming gallstones?
What are the main mechanisms of forming gallstones?
Signup and view all the flashcards
What complications can gallstones cause?
What complications can gallstones cause?
Signup and view all the flashcards
What characterizes cholesterolosis?
What characterizes cholesterolosis?
Signup and view all the flashcards
What role does cholesterol play in cells?
What role does cholesterol play in cells?
Signup and view all the flashcards
What are factors associated with increased cholesterol secretion?
What are factors associated with increased cholesterol secretion?
Signup and view all the flashcards
What indicates acute cholecystitis?
What indicates acute cholecystitis?
Signup and view all the flashcards
What causes calculous acute cholecystitis?
What causes calculous acute cholecystitis?
Signup and view all the flashcards
What causes acalculous acute cholecystitis?
What causes acalculous acute cholecystitis?
Signup and view all the flashcards
What are symptoms of acute cholecystitis
What are symptoms of acute cholecystitis
Signup and view all the flashcards
What are the gross features of acute cholecystitis?
What are the gross features of acute cholecystitis?
Signup and view all the flashcards
What is chronic cholecystitis?
What is chronic cholecystitis?
Signup and view all the flashcards
What are some properties of chronic cholecystitis
What are some properties of chronic cholecystitis
Signup and view all the flashcards
What are the major functions of the pancreas?
What are the major functions of the pancreas?
Signup and view all the flashcards
What does the exocrine function of pancreas provide?
What does the exocrine function of pancreas provide?
Signup and view all the flashcards
What is acute pancreatitis?
What is acute pancreatitis?
Signup and view all the flashcards
What are the common causes of acute pancreatis?
What are the common causes of acute pancreatis?
Signup and view all the flashcards
What are symptoms of acute pancreatitis?
What are symptoms of acute pancreatitis?
Signup and view all the flashcards
What histological sign indicates acute pancreatitis?
What histological sign indicates acute pancreatitis?
Signup and view all the flashcards
What is chronic pancreatitis?
What is chronic pancreatitis?
Signup and view all the flashcards
How does distribution of chronic pancreatitis subtypes differ?
How does distribution of chronic pancreatitis subtypes differ?
Signup and view all the flashcards
Name a pancreatic tumor.
Name a pancreatic tumor.
Signup and view all the flashcards
Where does ductal adenocarcinoma typically occur in pancreas?
Where does ductal adenocarcinoma typically occur in pancreas?
Signup and view all the flashcards
What causes Hepatocellular Carcinoma?
What causes Hepatocellular Carcinoma?
Signup and view all the flashcards
What causes Cholangiocarcinoma?
What causes Cholangiocarcinoma?
Signup and view all the flashcards
How do you identify Hemangioma?
How do you identify Hemangioma?
Signup and view all the flashcards
Study Notes
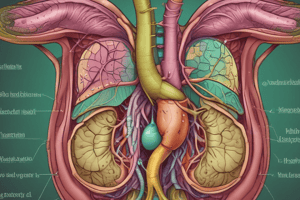
Gallbladder Anatomy and Function
- Gallbladder wall is 1 to 2 mm thick
- The gallbladder is pear-shaped
- The gallbladder has fundus, a body, and a neck; its wall contains mucosa, muscularis, and serosa
- The distal fundus goes beyond the anterior liver border
- The central body makes up most of the gallbladder
- The neck joins the cystic duct and narrows
- The extrahepatic biliary tree is outside the liver
- Right and left hepatic ducts join to form the common hepatic duct (CHD) in the porta hepatis (hilum of the liver)
- The common hepatic duct joins with the cystic duct to form the common bile duct
- The cystic duct links the gallbladder to the CHD
- The common bile duct results from the fusion of the CHD and cystic duct
- The common bile duct is 2 to 9 cm long
- The common bile duct runs behind the duodenum, through the pancreas head, and into the duodenum via the ampulla of Vater to discharge gallbladder contents
- The gallbladder stores and releases bile
- The gallbladder empties into the cystic duct
- The extrahepatic biliary tree serves to transport bile
- Cholecystokinin stimulates gallbladder contraction and stored bile release
- Bile is required for dietary fat intestinal absorption, but the gallbladder itself is not
- 95% of secreted bile acids are reabsorbed in the ileum, returning to the liver via portal blood, a process known as enterohepatic circulation
- The body eliminates Cholesterol evey day
Bile Salts and Lecithin
- Bile salts include cholates, chenodeoxycholates, deoxycholates, lithocholates, and ursodeoxycholates
- Bile salts: Major hepatic products of cholesterol metabolism
- Bile salts are water-soluble sterols
- Bile Salts solubilize water-insoluble lipids secreted by the liver into the biliary tree
- Bile salts promote dietary lipid absorption in the gut
- Lecithin (phosphatidylcholine) is hydrophobic and nonaqueous
- Lecithin (phosphatidylcholine) has minimal water solubility
Gallstones Composition and Formation
- Gallstones are composed of cholesterol, calcium, and bilirubin
- Cholesterol stones: Made mainly of cholesterol monohydrate, found in the gallbladder in >90% of the instances
- Black pigment stones: Composed of bilirubin polymers and calcium, located in the gallbladder and found in approximately 2% of the cases
- Brown pigment stones: Contain calcium bilirubinate, are located in infected bile ducts, and are present in approximately 10% of the instances
- Gallstone formation Mechanisms: Increased cholesterol secretion, Decreased bile acid secretion, or Combination of both
- Factors associated with increased cholesterol secretion in gallstone formation include age, obesity, estrogen treatment, female sex, and pregnancy
- Factors associated with decreased bile acid secretion include terminal ileum inflammatory bowel disease and prolonged fasting
- Cholesterol supersaturation in bile is the most important step that results in gallstone development
Complications of Gallstones
- Gallstones can cause impaction in the cystic duct, that results in acute cholecystitis
- Gallstones can cause billeary obstruction
- Gallstones can cause gallstone pancreatitis
Acute Cholecystitis
- Acute cholecystitis is an abrupt destructive process of the gallbladder
- Acute cholecystitis is frequently caused by stones blocking the cystic duct
- In acute cholecystitis, ~50% of cases are complicated by bacterial infection
- Essential features of acute cholecystitis is Inflammation of gallbladder by stones, ischemia, or substances
- Essential features of acute cholecystitis is Gallbladder wall thickening and pericholecystic fluid
- Essential features of acute cholecystitis include Complications such as perforation
- Acalculous cholecystitis: Seen more frequently in acalculous cholecystitis
- Cholecystectomy within 72 hours is typically curative for cholecystitis
Acute Cholecystitis Pathophysiology
- Calculous acute cholecystitis is caused by blockage of the neck or cystic duct
- Calculus blockage is often caused by gallstones or biliary sludge
- calculus blockage promotes Continued mucus production by the gallbladder with no outlet
- Calculus blockage creates Increased pressure within the gallbladder
- Calculus blockage inhibits Venous stasis, Arterial stasis and causes Gallbladder ischemia and necrosis
- Acalculous acute cholecystitis is is not caused by blockage of the cystic duct, its caused by Bile stasis and ischemia
- Acalculous acute cholecystitis is caused by Blood clotting disorders, No collateral blood supply (complete reliance on cystic artery), Cystic duct anomalies/congenital anomalies, Sphincter anomalies, Cystic Fibrosis, Viruses and Cocaine
- Symptoms of acute cholecystitis: include Right upper quadrant pain, nausea, vomiting, anorexia, and fever
- Other indications of acute cholecystitis include Leukocytosis and Hyperbilirubinemia with elevated liver function tests
- acute cholecystitis can result in Distention/edema
- acute cholecystitis can result in Serosa: Exudate and Hemorrhage
- acute cholecystitis can result in Wall-thickening
- acute cholecystitis can result in Mucosa: ulcers, stones, bile, hemorrhage
- acute cholecystitis complications include Rupture, Fistula, Abscess, Infected stones into biliary tree and Pancreatitis
- acute cholecystitis has mortality rate of 20%
Chronic Cholecystitis
- Chronic cholecystitis is Chronic inflammation of the gallbladder
- Chronic cholecystitis is the most common disease of the gallbladder
- Chronic cholecystitis is more common in the Female sex
- Chronic cholecystitis is Associated with stones in > 90% of cases
- Chronic cholecystitis is Often associated with repeated acute cholecystitis episodes
- Chronic cholecystitis Usually has vague RUQ pain, bloating, and indigestion as symptoms
- In Chronic cholecystitis the Gallbladder can be thickened or shrunken, strong clinical suspicion
Pancreas Location and Anatomy
- The pancreas is 15 cm in length, shaped like the letter J and sideways
- The loop of the sideways J of the pancreas is around the duodenum
- The pancreas parts are divided into the head, body and tail
- The pancreas is a Retroperitoneal organ (except tail)
- The retroperitoneal pancreas is close to the superior mesenteric artery and portal vein
- The Anterior body of the pancreas touches the posterior wall of the stomach
- The Posterior of the pancreas touches aorta, splenic vein and left kidney
- The Pancreatic tail extends to the splenic hilum
- The Orifice of the bile duct is called ampulla of Vater, with a sphincter of Oddi to release bile and pancreatic juice into the duodenum
- Anomalies of the Pancreas: Duct empties into common bile duct, not into ampulla directly
- Anomalies of the Pancreas: Abnormal bud fusion causes annular or heterotopic pancreas
- The pancreas has exocrine and endocrine functions
- Pancreas is divided into the head, neck, body and tail
- Pancreas drains secretions by the main pancreatic duct (with "vent") in major duodenal papilla (papilla of Vater)
- 5-10% of people have accessory pancreatic duct with orifice in minor duodenal papilla
- Pancreas is embedded in fibrous capsule passing in fibrous septa, separating lobuli
Pancreas Function, Exocrine and Endocrine
- Pancreas has exocrine and endocrine functions
- The exocrine function consists of 99% of the cells
- Exocrine function produces pancreatic juice from acinar cells
- Pancreatic juice contains bicarbonate and a lot of enzymes including proteolytic enzymes (trypsinogen, chymotrypsinogen, carboxypeptidase, elastase), lipolytic enzymes (lipase, esterase, phospholipase), saccharide degrading enzyme (amylase), nucleic acid degrading enzymes (DNAse, RNAse)
- Enzymes must be activated in the intestine before they perform their fucntions
- Trypsin catalyzes activation of the other enzymes
- The endocrine function consists of 1% of cells
- The endocrine function consists of a lot of types of hormones
- Hormones are released into the blood
- Glucagon production increases blood glucose concentration; insulin production decreases blood glucose, glucose intake in adipocytes and muscle cells
- Somatostatin production inhibits smooth muscle motility and antagonize gastrointestinal hormones
- Pancreatic polypeptide production regulates pancreatic juice and bile release
- Vasoactive intestinal polypeptide induces glycogenolysis and hyperglycemia to stimulates GI fluid secretion and causes secretory diarrhea
- P substance and serotonin -stimulatates gastrointestinal motility
- Gastrin -stimultes gastric juice release
- Pancreatic polypeptide -stimulates secretion of gastric and intestinal enzymes and inhibits intestinal motility
- Ghrelin - regulation of hunger and energetic metabolism
Acute Pancreatitis
- Acute pancreatitis is inflammatory disease of the exocrine pancreas
- Acute pancreatitis causes acute onset of severe abdominal pain to pancreatic necrosis
- Acute pancreatitis Reversibly injures pancreatic parenchyma
- Acute pancreatitis is caused by gallstones, alcohol and hypertriglyceridemia
- Main histological features of acute pancreatitis: Acute inflammatory cells with hemorrhage and necrosis
- Acute pancreatitis treatment is supportive
- In acute pancreatitis, 20-70% of ptiennts experiece a gallstone attack
- Acute pancreatitis affects the West and the male sex
- Peak prevalence for acute pancreatitis is in the fifth and sixth decades
- Second most common cause is alcohol accounting for 30% of cases
- Mortality of acute pancreatitis ranges from 3% to 20%
Acute pancreatitis symptoms
- Mild to severe epigastric pain
- Nausea and vomiting
- High white blood cell count
- Diffuse fat necrosis
- Peripheral vascular collapse
- Acute tubular necrosis
- Shock
- Electrolyte disturbances
- Endotoxemia
- Releases of cytokines
- Hypocalcemia
- Hyperglycemia.
- Pancreatic pseudocyst
- Walled-off necrosis
- Peripancreatic fluid collection
- Includes ARDS, acute kidney injury, and DIC
- Diffuse stippled,
- hemorrhagic, and
- black-brown necrosis
Chronic Pancreatitis
- Chronic pancreatitis is the fibroinflammatory syndrome
- Fibroinflammatory Syndrome is histologically parenchymal fibrosis, atrophy, and duct changes with pancreatis
- Fibroinflammatory Syndrome causes pain and symptoms of pancreatic insufficiency
- Pancreatic fibroinflammatory disease causes fibrosis, loss of acinar tissue and duct changes (stenosis)
- chronic pancreatitis histological diagnosis isn't efficient. Clinical and radiological data needs to happen
- Aicoholic pancreatitis: Young to middle aged males
- Obstructive pancreatitis: M = F; wide age range
- Hereditary pancreatitis: M = F; PRSS1 and CFTR related, where it affects very young children
- Hereditary pancreatitis: : M = F; SPINK1 related, where it affects adult patients
- Paraduodenal pancreatitis: Middle aged males with a history of alcohol abuse and smoking
- Alcoholic and hereditary chronic pancreatitis affects the whole pancreas
- Obstructive pancreatitis affects the gland past the obstruction site
- Paraduodenal pancreatitis centers in the groove area
- Alcoholic pancreatitis is caused by prolonged alcohol abuse and other cofactors such as smoking
- Obstructive pancreatitis is by obstruction of man or secondary pancreatic ducts due to mass forming lesions or intraductal stones
- Hereditary pancreatitis comes from germline mutations in PRSS1
- Paraduodenal pancreatitis results from the chronic obstruction of the mini papilla.
- Severe abdominal pain occurs often, often radiates to the interscapular region
- Paraduodenal pancreatitis may be associated with signs and symptoms of duodenal stenosis such as postprandial vomit
- Risk of developing pancreatic ductal adenocarcinoma is increase 10 fold for patients with chronic pancreatitis
- Risk and diagnostic factors are steatorrhea, weight loss, bloating and diabetes
Tumor Types and Pancreatic Ductal Adenocarcinoma (PDAC)
- Neoplasms can arise from any type of cell in the pancreas
- Pancreatic duodenal adenovarsinoma
- Exocrine cells
- Pancreatic ductal adenocarcinoma/PDAC tumor
- A pancreatic ductal adenocarcinoma (PDAC) is an invasive pancreatic epithelial neoplasm with glandular(ductal)differentiation
- It arises from pancreatic ductal epithelia, with elements, desmoplasia, and necrosis
- Poor prognosis: The 5 year survival rate is 6%
- 50% of cases: Head tumors
- 85% of cases distention of the biliary tree and progressive jaundice Heredity syndromes are
- Pertuz-Jeghers
- Familial atypical mole melanoma
- And Lynch syndrome To perform a curative surgery it's called "whipple Resection" This surgery removes cancerous tumors from organs other as well as the stomach and intestines And the sub total pancreaticoduodenectomy with a 2% of morality
Liver Tumors
- Hemangiomas
- Liver cell adenomas Well circumscribed tumors in women tumors is the hepatic adenoma
- It consist of benign Hepatocytes
- Usually asymptomatic and is Incidental diagnosis Hepatocellular Carcinoma A cancerous cells is "cerosis" for the liver <2% of women get cancer but in it most prevalent in Asia One of the biggest reason is "chronic liver cancer 90% of it is primary with liver tumors
- It's a malignancy arising from the thebillery tree It's very uncommon to find
- A 50 - 60 % of of intrapedal cholangiocarcinoma for for hilar cholangioclarcinoa. Metastatic Carcinoma 98% come from the liver from another organ
- Such as the lungs,breasts and colon If someone takes medication while pregnant they can have enlarged
- It's called focal nodular tumor (FNH)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.