Podcast
Questions and Answers
At what gestational age is amniocentesis typically indicated to assess inborn errors of metabolism and chromosomal abnormalities?
At what gestational age is amniocentesis typically indicated to assess inborn errors of metabolism and chromosomal abnormalities?
- 14-17 weeks (correct)
- 28 weeks
- 8-12 weeks
- 20 weeks
What is a primary reason for conducting fetal movement monitoring during pregnancy?
What is a primary reason for conducting fetal movement monitoring during pregnancy?
- To predict the delivery date
- To assess fetal well-being (correct)
- To measure amniotic fluid levels
- To determine fetal weight
For which group of pregnant women is amniocentesis particularly indicated due to potential genetic risks?
For which group of pregnant women is amniocentesis particularly indicated due to potential genetic risks?
- Women with multiple pregnancies
- Women with prior cesarean sections
- Women aged 35 years and older (correct)
- Women aged 20 years and younger
Which assessment technique cannot be performed during chorionic villus sampling (CVS)?
Which assessment technique cannot be performed during chorionic villus sampling (CVS)?
What is the significance of the Lecithin/Sphingomyelin (L/S) ratio in fetal assessments?
What is the significance of the Lecithin/Sphingomyelin (L/S) ratio in fetal assessments?
What should be done before performing amniocentesis if the patient's age of gestation (AOG) is more than 20 weeks?
What should be done before performing amniocentesis if the patient's age of gestation (AOG) is more than 20 weeks?
What potential complication should be monitored after amniocentesis?
What potential complication should be monitored after amniocentesis?
What is used to guide the needle placement during the amniocentesis procedure?
What is used to guide the needle placement during the amniocentesis procedure?
What indicates a reactive nonstress test (NST) result?
What indicates a reactive nonstress test (NST) result?
Which position is recommended for the mother to avoid vena cava compression during monitoring?
Which position is recommended for the mother to avoid vena cava compression during monitoring?
What is a key factor for classifying a contration stress test (CST) as negative?
What is a key factor for classifying a contration stress test (CST) as negative?
What characterizes a nonreactive nonstress test?
What characterizes a nonreactive nonstress test?
What is the purpose of a contraction stress test (CST)?
What is the purpose of a contraction stress test (CST)?
What is an equivocal CST result indicative of?
What is an equivocal CST result indicative of?
How often should the mother's blood pressure be monitored during a contraction stress test?
How often should the mother's blood pressure be monitored during a contraction stress test?
Which factor does NOT contribute to an unsatisfactory CST result?
Which factor does NOT contribute to an unsatisfactory CST result?
What common fear may arise for a woman in the third trimester of pregnancy as she prepares for delivery?
What common fear may arise for a woman in the third trimester of pregnancy as she prepares for delivery?
Which of the following statements about paternal reactions during the first trimester is accurate?
Which of the following statements about paternal reactions during the first trimester is accurate?
What is the primary purpose of performing a Nonstress Test (NST)?
What is the primary purpose of performing a Nonstress Test (NST)?
How is fetal movement typically monitored at home by expectant mothers?
How is fetal movement typically monitored at home by expectant mothers?
What is considered the normal range for fetal heart rate (FHR) during pregnancy?
What is considered the normal range for fetal heart rate (FHR) during pregnancy?
At what stage can ultrasound most reliably diagnose a pregnancy?
At what stage can ultrasound most reliably diagnose a pregnancy?
What method is used to ensure adequate visualization during a transabdominal ultrasound?
What method is used to ensure adequate visualization during a transabdominal ultrasound?
Which of the following is not typically assessed in a biophysical profile?
Which of the following is not typically assessed in a biophysical profile?
What is the technique referred to as the Sandovsky Method used for?
What is the technique referred to as the Sandovsky Method used for?
What type of ultrasound procedure is best performed when the bladder is empty?
What type of ultrasound procedure is best performed when the bladder is empty?
Flashcards are hidden until you start studying
Study Notes
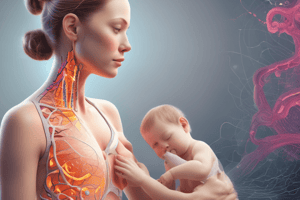
Amniocentesis
- Procedure involves aspirating amniotic fluid with a needle inserted through the abdominal and uterine walls.
- Performed between 14-17 weeks to detect inborn errors of metabolism, chromosomal abnormalities, open neural tube defects (NTD).
- After 28 weeks, amniocentesis can be used to identify sex-linked disorders and determine lung maturity.
- Indicated for pregnant women over 35, couples with a child with a genetic disorder, one or both parents with a genetic disorder, and mothers carrying X-linked disorders.
- Ultrasound is used prior to the procedure to locate a safe site for needle insertion.
- Potential complications: cramping, fluid leakage, minor irritation, and a slight risk of miscarriage.
- Before the procedure, the bladder should be emptied if gestational age (AOG) is over 20 weeks.
- Monitor for signs and symptoms of hemorrhage, labor, premature placental separation, fetal distress, amniotic fluid embolism, infection, and potential injury to maternal intestines/bladder or fetus after the procedure.
- Administer RhoGAM to Rh-negative mothers.
Chorionic Villus Sampling (CVS)
- Involves transcervical aspiration of chorionic villi, allowing for first-trimester (8-12 weeks) diagnosis of genetic disorders.
- Offers comparable diagnostic capabilities to amniocentesis, except for NTD detection due to the absence of amniotic fluid retrieval.
- Full bladder is required before the procedure.
- Ultrasound is utilized for guidance, similar to Amniocentesis.
- Post-procedure monitoring is the same as Amniocentesis.
Estriol Levels
- Serial 24-hour maternal urine samples or serum specimens are used to assess fetoplacental status.
- Falling estriol levels usually indicate deterioration.
Percutaneous Umbilical Blood Sampling (PUBS)
- Second and third trimester procedure involving aspirating cord blood for testing genetic conditions, chromosomal abnormalities, fetal infections, hemolytic and hematological disorders.
- Ultrasound is used for identifying the location of the cord.
Lecithin/Sphingomyelin Ratio (L/S) 2:1
- Important components of surfactant, a phosphoprotein that reduces surface tension within the lungs, facilitating extrauterine expiration.
Psychological Tasks of Pregnancy - Third Trimester
Preparing for Delivery and Parenthood
- "I am going to be a mother": Possible new fears regarding labor and delivery, with fantasies about the baby's appearance.
- Women begin planning for the baby's arrival; selecting a layette, choosing names, making plans for feeding and sleeping arrangements.
Paternal Reactions to Pregnancy
First Trimester
- Ambivalence and anxiety about their role change.
- Concern for identification with the mother's discomfort (Couvade syndrome).
Second Trimester
- Increased confidence and interest in the mother's care.
- Difficulty relating to the fetus.
- "Jealousy"
Assessment of Fetal Growth
- Assessing Fetal Well-being:
- Fetal movement
- Fetal heart rate
- Ultrasound
- Nonstress test (NST)
- Electrocardiography (ECG)
- MRI
- Amnioscopy
- Fetoscopy
- Biophysical profile
- Maternal serum alpha-fetoprotein (MSAFP)
- Triple screening (AFP, estriol, and HCG)
- Chorionic villi sampling
- Percutaneous umbilical blood sampling (PUBS)
Fetal Movement
- Fetal movement felt by the mother is called Quickening, which typically begins at 18-20 weeks and peaks between 28-38 weeks.
- Primigravida (first pregnancy) experience quickening at 20 weeks (5 months).
- Multigravida (multiple pregnancies) experience quickening at 16 weeks (4 months).
- Mothers should be advised to observe fetal movement.
- A healthy fetus moves at least 10 times a day.
Fetal Movement Methods
Sandovsky Method
- Mother lies in a left lateral recumbent position.
- Fetus normally moves at least twice every 10 minutes, or an average of 10-12 times per hour.
Cardiff Method
- Count to ten: Record the time it takes for the mother to feel 10 fetal movements; typically completed within 60 minutes.
Fetal Heart Rate (FHR)
- Normal range: 120-160 beats per minute.
- Doppler can detect FHR between 10-12 weeks (3 months).
- Fetoscope can detect FHR at 18-20 weeks (4 months).
- Stethoscope can detect FHR at 20 weeks (5 months).
Ultrasound
- Uses sound waves to visualize uterine content.
- Two types:
- Transabdominal Ultrasound: Full bladder required. Client lies on their back.
- Transvaginal Ultrasound: Probe inserted into the vagina. Lithotomy position required. Empty bladder.
- Ultrasound is most effective between 8-18 weeks.
Ultrasound Uses
- Diagnose pregnancy as early as 6 weeks.
- Confirm the presence, size, and location of the placenta and amniotic fluid.
- Assess fetal growth and screen for gross defects (hydrocephalus, anencephaly, spinal cord, heart, kidney, and bladder defects).
- Determine fetal presentation and position.
- Predict maturity by measuring biparietal diameter (BPD).
- Identify pregnancy complications or fetal abnormalities.
Nonstress Test (NST)
- Measures the response of fetal heart rate to fetal movement.
- Evaluates fetal well-being.
- Assesses placental function and oxygenation.
Nonstress Test (NST) Procedure
- External ultrasound transducer and tocodynamometer applied to the mother for at least 20 minutes to monitor FHR and uterine activity.
- Obtain baseline blood pressure and monitor frequently.
- Position the mother in semi-Fowler's or side-lying position to prevent vena cava compression.
- Mother presses a button when feeling fetal movement, which is recorded on the monitor as a reference point for FHR response.
NST Results
Reactive NST: Normal/Negative
- Indicates a healthy fetus.
- Requires 2 or more FHR accelerations, at least 15 beats per minute lasting at least 15 seconds from the beginning to the end, associated with fetal movement, during a 20-minute period.
Nonreactive NST: Abnormal
- No accelerations or accelerations less than 15 bpm or lasting less than 15 seconds occur in a 40-minute observation.
Unsatisfactory
- FHR tracing quality is poor, preventing proper interpretation.
Contraction Stress Test (CST) or Oxytocin Challenge Test (OCT)
- Assesses placental oxygenation and function.
- Determines fetal tolerance of labor and overall well-being.
- Fetal exposure to the stressor of contractions assesses placental perfusion under simulated labor conditions.
CST or OCT Procedure
- External fetal monitor applied for a 20-30 minute baseline recording.
- Uterine contractions are induced by administering dilute oxytocin or through nipple stimulation until three palpable contractions lasting 40 seconds or more occur within a 10-minute period.
- Frequent maternal blood pressure readings are taken, and the mother is closely monitored during oxytocin administration.
CST Results
Negative CST: Normal
- No late or variable deceleration of FHR.
Positive CST: Abnormal
- Late or variable FHR deceleration with 50% or more of the contractions in the absence of uterine hyperstimulation.
Equivocal
- FHR deceleration with less than 50% of the contractions, or hyper-stimulated uterine activity is present.
Unsatisfactory
- Adequate uterine contractions cannot be achieved or the FHR tracing is insufficient for proper interpretation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.