Podcast
Questions and Answers
At physiological pH, what charges do amino acids typically carry?
At physiological pH, what charges do amino acids typically carry?
- Positive charge on the amino group, negative charge on the carboxy group. (correct)
- Positive charge on the carboxy group, negative charge on the amino group.
- Positive charge on both the amino and carboxy groups.
- Negative charge on both the amino and carboxy groups.
Which of the following amino acids is considered purely ketogenic?
Which of the following amino acids is considered purely ketogenic?
- Lysine (correct)
- Phenylalanine
- Isoleucine
- Tryptophan
During periods of growth, the body requires higher amounts of which of the following amino acids?
During periods of growth, the body requires higher amounts of which of the following amino acids?
- Leucine and lysine
- Phenylalanine and valine
- Aspartic acid and glutamic acid
- Arginine and histidine (correct)
How does excess nitrogen from amino acid catabolism get processed by the body?
How does excess nitrogen from amino acid catabolism get processed by the body?
In ornithine transcarbamylase deficiency, excess carbamoyl phosphate is converted to which of the following, leading to increased levels in blood and urine?
In ornithine transcarbamylase deficiency, excess carbamoyl phosphate is converted to which of the following, leading to increased levels in blood and urine?
A patient presents with hyperammonemia, and lab results show decreased BUN levels, lethargy, and cerebral edema. Which urea cycle enzyme is most likely deficient?
A patient presents with hyperammonemia, and lab results show decreased BUN levels, lethargy, and cerebral edema. Which urea cycle enzyme is most likely deficient?
Which of the following immunosuppressants directly inhibits dihydroorotate dehydrogenase, affecting pyrimidine synthesis?
Which of the following immunosuppressants directly inhibits dihydroorotate dehydrogenase, affecting pyrimidine synthesis?
What is the primary mechanism of action of 6-mercaptopurine (6-MP) and its prodrug azathioprine in suppressing the immune system?
What is the primary mechanism of action of 6-mercaptopurine (6-MP) and its prodrug azathioprine in suppressing the immune system?
In the Cahill cycle, what is transported from the muscle to the liver?
In the Cahill cycle, what is transported from the muscle to the liver?
Which of the following treatments helps reduce ammonia levels in patients with hyperammonemia by acidifying the GI tract and trapping $NH_4^+$ for excretion?
Which of the following treatments helps reduce ammonia levels in patients with hyperammonemia by acidifying the GI tract and trapping $NH_4^+$ for excretion?
Melanin synthesis depends directly on which amino acid derivative?
Melanin synthesis depends directly on which amino acid derivative?
Carbidopa is often administered with L-DOPA to treat Parkinson's disease. What is the role of carbidopa in this treatment?
Carbidopa is often administered with L-DOPA to treat Parkinson's disease. What is the role of carbidopa in this treatment?
A newborn screening reveals elevated levels of phenylalanine. What supplementation is required to prevent neurological damage?
A newborn screening reveals elevated levels of phenylalanine. What supplementation is required to prevent neurological damage?
A patient with phenylketonuria (PKU) needs to avoid a certain artificial sweetener. What is the name of this sweetener and why?
A patient with phenylketonuria (PKU) needs to avoid a certain artificial sweetener. What is the name of this sweetener and why?
A patient is diagnosed with alkaptonuria. Which of the following substances accumulates in tissues resulting in bluish-black discoloration, especially in cartilage and sclera?
A patient is diagnosed with alkaptonuria. Which of the following substances accumulates in tissues resulting in bluish-black discoloration, especially in cartilage and sclera?
Which disorder is characterized by a deficiency in tyrosinase and results in hypopigmentation?
Which disorder is characterized by a deficiency in tyrosinase and results in hypopigmentation?
A child is diagnosed with maple syrup urine disease. What are the three amino acids that are elevated?
A child is diagnosed with maple syrup urine disease. What are the three amino acids that are elevated?
A child presents with urine that smells like maple syrup. Which enzyme is most likely deficient?
A child presents with urine that smells like maple syrup. Which enzyme is most likely deficient?
A patient is diagnosed with methylmalonic acidemia and placed on a low VOMIT diet. Which of the following amino acids should be restricted?
A patient is diagnosed with methylmalonic acidemia and placed on a low VOMIT diet. Which of the following amino acids should be restricted?
What vitamin deficiency leads to increased homocysteine levels?
What vitamin deficiency leads to increased homocysteine levels?
Which of the following conditions is associated with decreased homocysteine levels and lower risk of cardiac diseases?
Which of the following conditions is associated with decreased homocysteine levels and lower risk of cardiac diseases?
A patient is diagnosed with homocystinuria due to cystathionine beta-synthase deficiency. What signs may he exhibit?
A patient is diagnosed with homocystinuria due to cystathionine beta-synthase deficiency. What signs may he exhibit?
Which of the following is the MOST common and severe manifestation of homocystinuria and requires restriction of methionine and addition of cysteine?
Which of the following is the MOST common and severe manifestation of homocystinuria and requires restriction of methionine and addition of cysteine?
A patient is diagnosed with cystinuria, secondary to impaired reabsorption of certain amino acids in the renal PCT and intestines. Which amino acids are involved?
A patient is diagnosed with cystinuria, secondary to impaired reabsorption of certain amino acids in the renal PCT and intestines. Which amino acids are involved?
A lab analysis reveals elevated homocysteine and normal methylmalonic acid levels. Which vitamin deficiency is most likely the cause?
A lab analysis reveals elevated homocysteine and normal methylmalonic acid levels. Which vitamin deficiency is most likely the cause?
Which genetic disorder associated with amino acid degradation results in liver damage, including hepatitis progressing to cirrhosis, and kidney issues like aminoaciduria?
Which genetic disorder associated with amino acid degradation results in liver damage, including hepatitis progressing to cirrhosis, and kidney issues like aminoaciduria?
A patient tests positive for mousy odor. What amino acid degradation disorder does this indicate?
A patient tests positive for mousy odor. What amino acid degradation disorder does this indicate?
Which level of protein structure is determined by the sequence of amino acids?
Which level of protein structure is determined by the sequence of amino acids?
What maintains the protein sequence?
What maintains the protein sequence?
Secretion of the Preproinsulin protein requires a cleavage of 'presignal'. What is the next step in the process, leading to insulin secretion?
Secretion of the Preproinsulin protein requires a cleavage of 'presignal'. What is the next step in the process, leading to insulin secretion?
What type of interactions primarily stabilize the secondary structure of a protein?
What type of interactions primarily stabilize the secondary structure of a protein?
The alpha helix is very common and stable, except when what amino acid is present because it will not allow the formation?
The alpha helix is very common and stable, except when what amino acid is present because it will not allow the formation?
How are adjacent strands aligned in beta-pleated sheets?
How are adjacent strands aligned in beta-pleated sheets?
What stabilizes the collagen triple helix?
What stabilizes the collagen triple helix?
What type of interactions stabilize the tertiary structure of a protein, leading to its specific 3D conformation?
What type of interactions stabilize the tertiary structure of a protein, leading to its specific 3D conformation?
What is the name of each polypeptide chain that is a subunit or monomer of a protein?
What is the name of each polypeptide chain that is a subunit or monomer of a protein?
What specific step in pro-collagen formation directly relies on vitamin C?
What specific step in pro-collagen formation directly relies on vitamin C?
What is function of the enzyme(s) pro collagen peptidases and where is its action performed?
What is function of the enzyme(s) pro collagen peptidases and where is its action performed?
What causes the oxidative deamination of lysines and hydroxylysines?
What causes the oxidative deamination of lysines and hydroxylysines?
What is the result if there is excessive and decreased cross-linking?
What is the result if there is excessive and decreased cross-linking?
What deficiency leads to Alport syndrome and Goodpasture syndrome is known to target, or attack, this product
What deficiency leads to Alport syndrome and Goodpasture syndrome is known to target, or attack, this product
A person presents with hyper extensible skin and hypermobile joints. Genetic results show a mutation. What is the syndrome and what genetic abnormality is known?
A person presents with hyper extensible skin and hypermobile joints. Genetic results show a mutation. What is the syndrome and what genetic abnormality is known?
What results in unopposed elastase activity which can cause COPD?
What results in unopposed elastase activity which can cause COPD?
What are aggregates of misfolded proteins resistant to?
What are aggregates of misfolded proteins resistant to?
Flashcards
Amino Acid Structure
Amino Acid Structure
An amino acid contains a carboxyl group, an amino group, and a side chain bonded to an alpha-carbon.
Amino Acid Charge at pH
Amino Acid Charge at pH
At physiological pH amino acids have a positive charge on their amino group and a negative charge on their carboxy group.
What are Peptide Bonds?
What are Peptide Bonds?
Peptide bonds are covalent chemical bonds linking amino acid residues in a chain.
Essential Amino Acids
Essential Amino Acids
Signup and view all the flashcards
Glucogenic Amino Acids
Glucogenic Amino Acids
Signup and view all the flashcards
Glucogenic and Ketogenic AA
Glucogenic and Ketogenic AA
Signup and view all the flashcards
Ketogenic Amino Acids
Ketogenic Amino Acids
Signup and view all the flashcards
Acidic Amino Acids
Acidic Amino Acids
Signup and view all the flashcards
Basic Amino Acids
Basic Amino Acids
Signup and view all the flashcards
Urea Cycle Mnemonic
Urea Cycle Mnemonic
Signup and view all the flashcards
Excess Carbamoyl Phosphate
Excess Carbamoyl Phosphate
Signup and view all the flashcards
Ornithine Transcarbamylase findings
Ornithine Transcarbamylase findings
Signup and view all the flashcards
Carbamoyl Phosphate Synthetase deficiencies
Carbamoyl Phosphate Synthetase deficiencies
Signup and view all the flashcards
Ornithine Transcarbamoylase deficiencies
Ornithine Transcarbamoylase deficiencies
Signup and view all the flashcards
Leflunomide
Leflunomide
Signup and view all the flashcards
5-Fluorouracil (5-FU)
5-Fluorouracil (5-FU)
Signup and view all the flashcards
6-Mercaptopurine (6-MP)
6-Mercaptopurine (6-MP)
Signup and view all the flashcards
Mycophenolate and Ribavirin
Mycophenolate and Ribavirin
Signup and view all the flashcards
Hydroxyurea
Hydroxyurea
Signup and view all the flashcards
What is Cahill cycle.
What is Cahill cycle.
Signup and view all the flashcards
Hyperammonemia Presentation
Hyperammonemia Presentation
Signup and view all the flashcards
Hyperammonemia Treatment
Hyperammonemia Treatment
Signup and view all the flashcards
What is Tyrosine?
What is Tyrosine?
Signup and view all the flashcards
What is PKU?
What is PKU?
Signup and view all the flashcards
Alkaptonuria
Alkaptonuria
Signup and view all the flashcards
What is Albinism
What is Albinism
Signup and view all the flashcards
Maple syrup urine disease (MSUD)
Maple syrup urine disease (MSUD)
Signup and view all the flashcards
Organic acidemias
Organic acidemias
Signup and view all the flashcards
What is Homocystinuria
What is Homocystinuria
Signup and view all the flashcards
Homocystinuria TX
Homocystinuria TX
Signup and view all the flashcards
What is Cystinuria?
What is Cystinuria?
Signup and view all the flashcards
What is Primary structure
What is Primary structure
Signup and view all the flashcards
CHAIN 1: GIVEQ CCTSI CSLYQ LENYC N. CHAIN 2: FVNQH LCGSH LVEAL YLVCG ERGFF YTPKT.
CHAIN 1: GIVEQ CCTSI CSLYQ LENYC N. CHAIN 2: FVNQH LCGSH LVEAL YLVCG ERGFF YTPKT.
Signup and view all the flashcards
Secondary structure
Secondary structure
Signup and view all the flashcards
The a-helix
The a-helix
Signup and view all the flashcards
The beta pleated sheet
The beta pleated sheet
Signup and view all the flashcards
What is Quaternary structure
What is Quaternary structure
Signup and view all the flashcards
Structure of Hemoglobin
Structure of Hemoglobin
Signup and view all the flashcards
RER: Formation of Pro-collagen
RER: Formation of Pro-collagen
Signup and view all the flashcards
Lysyl/prolyl oxidase
Lysyl/prolyl oxidase
Signup and view all the flashcards
Study Notes
Amino Acids
- Amino acids have a carboxyl group, an amino group, and a side chain, all bonded to an alpha-carbon atom.
- At a physiological pH, amino acids have a positive charge on their amino group and a negative charge on their carboxy group.
- Peptide bonds link adjacent amino acid residues in a protein chain.
- Proteins usually have 20 amino acids.
- The L-amino acid configuration exists in proteins.
Amino Acid Classes
- Only L-amino acids are in proteins.
- The essential amino acids PVT TIM HaLL are: Phenylalanine, Valine, Tryptophan, Threonine, Isoleucine, Methionine, Histidine, Leucine, Lysine.
- Glucogenic amino acids are: Methionine, histidine, valine.
- Glucogenic/ketogenic amino acids: Isoleucine, phenylalanine, threonine, tryptophan.
- Leucine and lysine are the only purely ketogenic amino acids.
- Aspartic acid and glutamic acid are acidic amino acids.
- Acidic amino acids are negatively charged at body pH.
- Arginine, histidine, and lysine are basic.
- Arginine is most basic.
- Histidine has no charge at body pH.
- Arginine and histidine are required during growth periods.
- Arginine and lysine are found in histones, which bind negatively charged DNA.
Catabolism of Amino Acids
- Amino acid catabolism generates common metabolites (eg, pyruvate, acetyl-CoA) that serve as metabolic fuels.
- Excess nitrogen is converted to urea and excreted by the kidneys.
Urea Cycle
- The urea cycle converts excess nitrogen from amino acid catabolism into urea for excretion.
- Key intermediates in the urea cycle: Ornithine, Citrulline, Arginine, Aspartate.
Ornithine Transcarbamylase Deficiency
- Most common urea cycle disorder.
- It is X-linked recessive, while other urea cycle enzyme deficiencies are autosomal recessive.
- It interferes with the body's ability to eliminate ammonia and is often evident in the first few days of life, but may appear later.
- Excess carbamoyl phosphate is converted to orotic acid, part of the pyrimidine synthesis pathway.
- Findings include elevated orotic acid in blood and urine, decreased BUN, and symptoms of hyperammonemia, but no megaloblastic anemia (vs orotic aciduria).
Clinical Features of Urea Cycle Defects
- Increased ammonia levels ([NH4+]) lead to hyperammonemia.
- Blood glutamine levels are increased.
- BUN levels are decreased.
- Cerebral edema often occurs.
- Symptoms include lethargy, convulsions, coma, and potentially death.
- Carbamoyl phosphate synthetase deficiency: No orotic aciduria, autosomal recessive.
- Ornithine transcarbamoylase deficiency: Orotic aciduria, X-linked recessive, Carbamoyl-P leaks out of the mitochondria, and affects pyrimidine pathway.
De Novo Pyrimidine & Purine Synthesis
- Several immunosuppressive, antineoplastic, and antibiotic drugs function by interfering with nucleotide synthesis.
- Leflunomide inhibits dihydroorotate dehydrogenase in pyrimidine synthesis.
- 5-fluorouracil (5-FU) and its prodrug capecitabine form 5-F-dUMP, inhibiting thymidylate synthase (↓ dTMP).
- 6-mercaptopurine (6-MP) and its prodrug azathioprine inhibit de novo purine synthesis.
- Azathioprine is metabolized via a purine degradation pathway and can cause immunosuppression when administered with a xanthine oxidase inhibitor.
- Mycophenolate and ribavirin inhibit inosine monophosphate dehydrogenase.
- Hydroxyurea inhibits ribonucleotide reductase, affecting both purine and pyrimidine synthesis.
- Methotrexate (MTX), trimethoprim (TMP), and pyrimethamine inhibit dihydrofolate reductase and lower deoxythymidine monophosphate [dTMP] levels.
- Methotrexate affects humans, trimethoprim affects bacteria, and pyrimethamine affects protozoa.
- CPS1 is found in the mitochondria in the liver for the urea cycle.
- CPS2 is found in the cytosol and is responsible for pyrimidine synthesis found in most cells.
Transport of Ammonia by Alanine
- Alanine transports ammonia from muscle to the liver.
- In the muscle, amino acids are converted to α-ketoacids while α-ketoglutarate is converted to glutamate. Glutamate is converted to alanine.
- Glucose is converted to pyruvate, then Lactate, the lactate goes through the Cori Cycle
- In the liver, alanine is converted back to pyruvate and then to glucose, α-ketoglutarate is formed, and urea is produced.
Hyperammonemia
- Hyperammonemia can be acquired (e.g., liver disease) or hereditary (e.g., urea cycle enzyme deficiencies).
- Symptoms include flapping tremor (asterixis), slurring of speech, somnolence, vomiting, cerebral edema, and blurred vision.
- Elevated NH3 alters the amounts of α-ketoglutarate, glutamate, GABA, and glutamine, leading to CNS toxicity through increased GABAergic tone, TCA cycle inhibition, and cerebral edema.
- Treatment involves limiting protein in the diet.
- Lactulose can acidify the GI tract to trap NH4+ for excretion.
- Antibiotics (e.g., rifaximin) can reduce ammoniagenic bacteria.
- Benzoate, phenylacetate, or phenylbutyrate can react with glycine or glutamine, forming products that the kidneys excrete.
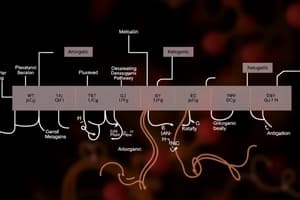
Amino Acid Derivatitives
- Phenylalanine becomes Tyrosine via BH4, Tyrosine becomes Dopa via BH4, Dopa becomes Dopamine via B6, Dopamine becomes NE via Vitamin C, and NE becomes Epi via SAM.
- Tyrosine also becomes thyroxine and melanin.
- Tryptophan becomes Niacin via B2 & B6 and Serotonin via BH4, Serotonin can become Melatonin via B.
- Histidine becomes Histamine via B6.
- Glycine becomes Porphyrin via B6 and then Heme.
- Glutamate becomes GABA via B6 and Glutathione.
- Arginine becomes Creatine, Urea, and Nitric oxide via BH4.
Catecholamine Synthesis/Tyrosine Catabolism
- Phenylalanine becomes Tyrosine via Phenylalanine hydroxylase & BH4.
- Tyrosine becomes DOPA via Tyrosine hydroxylase & BH4.
- DOPA becomes Dopamine via DOPA decarboxylase & B6.
- Dopamine becomes Norepinephrine via Dopamine B-hydroxylase & Vitamin C.
- Norepinephrine becomes Epinephrine via Phenylethanolamine-N-methyltransferase & SAM.
- Carbidopa inhibits DOPA decarboxylase.
- Albinism is a result of a deficiency of Tyrosinase
- PKU is a result of a deficiency of Phenylalanine hydroxylase (PAH)
Phenylketonuria (PKU)
- PKU is caused by a deficiency of phenylalanine hydroxylase (PAH); as a result, tyrosine becomes essential, and phenylalanine levels increase, leading to increased phenyl ketones in the urine.
- Autosomal recessive.
- Screening occurs 2-3 days after birth (normal at birth because of the maternal enzyme during fetal life).
- Findings include intellectual disability, microcephaly, seizures, hypopigmented skin, eczema, and a musty body odor.
- Treatment includes decreasing phenylalanine and increasing tyrosine in the diet and tetrahydrobiopterin supplementation.
- Phenyl ketones include phenylacetate, phenyllactate, and phenylpyruvate.
- The disorder of aromatic amino acid metabolism leads to a musty body odor.
- Patients with PKU must avoid the artificial sweetener aspartame because it contains phenylalanine.
Alkaptonuria
- Congenital homogentisate oxidase deficiency in tyrosine to fumarate degradative pathway.
- Leads to pigment-forming homogentisic acid buildup in tissue. Autosomal recessive.
- Findings include bluish-black connective tissue, ear cartilage, and sclerae (ochronosis); urine turns black on prolonged exposure to air.
- May have debilitating arthralgias (homogentisic acid toxic to cartilage).
Albinism
- Deficiency in tyrosinase.
- Autosomal recessive.
- No DOPA converted to melanin.
- The two types of albinism are occulocutaneous and ocular.
- Absence of melanin in hair (white), eye (photophobia, nystagmus), and skin (pink) results in hypopigmentation with an increased risk of UV light-related skin cancer.
Branched Chain Amino Acids
- The branched chain amino acids are Leucine, Valine, and Isoleucine.
- They go through branch chain aminotransferase but not in the liver to create keto acid.
- Then TPP, Lipoate, FAD, and NAD+ convert the keto acid to Keto acyl CoA via branch chain α-Keto acid dehydrogenase Complex, a deficiency here results in Maple Syrup Disease in which urine has the odor of maple syrup.
Propionate Connection
- Propionate is converted to Propionyl-CoA through the use of CoA-SH, Mg2+, and Acyl-CoA synthetase.
- Propionyl-CoA is then converted to D-Methyl-malonyl-CoA through the use of Biotin, ATP, and Propionyl-CoA Carboxylase.
- D-Methyl-malonyl-CoA is converted to L-Methyl-malonyl-CoA through the use of METHYLMALONYL-CoA RACEMASE.
- L-Methyl-malonyl-CoA is converted to Succinyl-CoA through the use of B12 coenzyme and METHYLMALONYL-CoA ISOMERASE.
Clinical Correlations for Branched Chain Deficiencies
- Deficiency in Branched chain α-keto dehydrogenase-Maple syrup causes the urine to have the odor of maple syrup.
- Symptoms: include feeding difficulties, lethargy, vomiting, encephalopathy-mental retardation, seizure, hypoglycemia, protein intolerance, ketosis, coma, and ultimately death.
- Deficiency in Propionic carboxylase- Propionic Acidemia results in No conversion of Propionic acid to methyl malonyl CoA then to succinyl CoA.
- Symptoms: Neurologic and developmental complications.
- Treatment: with a low-protein diet; L-Carnitine improves (β-oxidation of fatty acids) and the intake of methionine, valine, isoleucine and odd-chain fatty acids is increased.
- Deficiency in methyl malonyl CoA mutase(isomerase) in this pathway lead to methyl malonyl acidemia.
- The patient will experience Neurologic Arid developmental complications.
- Rule out vitamin B12 deficiency as a cause.
Maple Syrup Urine Disease
- Maple Syrup Urine Disease is caused by the Blocked degradation of branched amino acids (Isoleucine, leucine, valine) due to branched-chain α-ketoacid dehydrogenase (B₁).
- This leads to an increase of α-ketoacids in the blood, especially those of leucine.
- Treatment includes restriction of isoleucine, leucine, valine in diet, and thiamine supplementation
- Autosomal recessive.
- Presentation in infants vomiting and poor feeding will produce urine that smells like maple syrup/bunt sugar. It causes progressive neurological decline.
Organic Acidemias
- Protein metabolism of Valine, Odd-chain fatty acids, Methionine, Isoleucine, and Threonine can result in Methylmalonic Acidemia and Propionic Acidemia
- Commonly present in infancy with poor feeding, vomiting, hypotonia, high anion gap metabolic acidosis, hepatomegaly, and seizures. Results in Organic acid accumulation.
- Results in inhibition of gluconeogenesis, leading to fasting blood glucose levels, ↑ ketoacidosis → resulting in high anion gap metabolic acidosis
- Leads to urea cycle inhibition, resulting in hyperammonemia.
- Treatment: low-protein diet limited in substances that metabolize into propionyl-CoA: Valine, Odd-chain fatty acids, Methionine, Isoleucine, and Threonine (VOMIT).
Methionine-Methyl Trap
- Methionine is synthesized from Homocysteine, and the enzyme Methionine synthase requires THF4 and Cobalamin.
- Methionine is then converted to S-adenosyl methionine using ATP
- S-adenosyl methionine is converted to S-adenosyl homocysteine using a Methyl transferase.
- S-adenosyl homocysteine is then converted back to Homocysteine.
- Serine is converted to Cystathionine using the Cystathionine synthase and requires Vitamin B6.
- Cystathionine is converted to Cysteine using Cystathionase and requires Vitamin B6.
Recall of Methionine
- α1-antitrypsin-increases the oxidized form of Methionine when there is Lung- smoking, resulting in increased lung damage.
- Cardiac situations are linked to decreased homocysteine, thus there are fewer cardiac diseases
- Alcoholism (cirrhosis) is linked to decreased B9 and increased homocysteine.
- Megaloblastic anemia can be result of Deficient Vit B9
Abormal Cystathionine Function
- Deficiency of Cystathionine β-Synthase can lead to Homocystinuria which can be caused by autosomal recessive. and results marked increase in homocysteine and metabolism.
- Clinical Features: Homocysteine damages endothelial cells which causes thrombosis resulting in thrombotic vascular diseases, there is a 50% chance of developing a myocardial infarction, stroke, or serious blood clot before the age of 30 years, osteoporosis(skeletal deformities), ectopia lentis- abnormalities of the ocular lens (dislocation(similar to Marfan syndrome), arachnodactyly ("spider fingers"), and mental retardation.
- Treatment: Requires High doses of vitamin B6, restriction of methionine, addition of cysteine
Homocystinuria
- There are 4 Causes (all autosomal recessive):
- Cystathionine synthase deficiency (treatment: ↑ methionine, ↓ cysteine, ↑ B6, B12, and folate in diet
- ↑ affinity of cystathionine synthase for pyridoxal phosphate (treatment: ↑↑ B6 and ↓ cysteine in diet)
- Methionine synthase (homocysteine methyltransferase) deficiency (treatment: ↑ methionine in diet)
- Methylenetetrahydrofolate reductase (MTHFR) deficiency (treatment: ↑ folate in diet)
- In all forms there is an excess homocysteine.
- HOMOCYstinuria: ↑↑ Homocysteine in urine, Osteoporosis, Marfanoid habitus, Ocular changes (downward and inward lens subluxation), Cardiovascular effects (thrombosis and atherosclerosis → stroke and MI), kyphosis, intellectual disability, hypopigmented skin. In homocystinuria, lens subluxes "down and in" (vs Marfan, "up and fans out").
Cystinuria
- Hereditary Defect is the renal PCT and intestinal amino acid transporter prevents reabsorption of Cystine, Ornithine, Lysine, and Arginine (COLA).
- Cystine is made of 2 cysteines connected by a disulfide bond.
- Excess cystine in the urine can lead to recurrent precipitation of hexagonal cystine stones A
- Treatment: requires urinary alkalinization (eg, potassium citrate, acetazolamide) and chelating agents (eg, penicillamine) ↑ solubility of cystine stones; good hydration; diet low in methionine.
- Autosomal recessive. Common (1:7000).
- Cystinuria detected with urinary sodium- cyanide nitroprusside test and proton nuclear magnetic resonance spectroscopy of urine.
Homocysteine vs Methylmalonic
- Folate and B12 both become homocysteine
- B12 becomes methylmalonic acid
Deficiencies of Folate and B12
- Hematocrit goes down in both Folate Deficiency and B12 Deficiency
- MCV goes up in both Folate Deficiency and B12 Deficiency
- Homocysteine goes up in both Folate Deficiency and B12 Deficiency
- Methylmalonic Acid stays normal in Folate Deficiency and goes up in B12 Deficiency
- Neuro Symptoms stays None in Folate Deficiency and appears in B12 Deficiency
Summary On Genetic Disorders
- Tyrosinosis (AR) leads Liver damage (hepatitis progressing to cirrhosis and hepatocellular carcinoma) and kidneys (aminoaciduria and renal tubular acidosis).
- Maple syrup urine disease (AR) presents with Feeding difficulties vomiting and urine smells of maple syrup Treat by restricting Isoleucine Leucine and Valine
- Homocystinuria Defective homocysteine metabolism. High homocysteine with downward lens dislocation.
- Propionic acidemia: Neurologic and developmental complications; Treatment: low-protein diet;
- Methylmalonic acidemia :Defective methylmalonic acid metabolism. Neurologic and developmental complications: Treatment: low-protein diet;
More Genetic Disorders
- Classic PKU (autosomal recessive, AR): Leads Mental retardation, fair skin and urine smells like mousy odor
- Albinism (AR) can not covert tyrosine which results Absence of melanin in hair
- Alkaptonuria (AR) Homogentiside 1 urine (turns black when oxidized by light) Articular cartilage and sclera darken (ochronosis)
Structure and Properties of Proteins
- The sequence of the amino acids in a polypeptide chain denotes its primary structure.
- The primary structure is linear, ordered, and 1-dimensional.
- By convention, the primary structure is written from the amino end to the carboxyl end.
- A perfectly linear amino acid polymer is neither functional nor energetically favorable due to the need for folding.
Primary Structure of Insulin
- The primary structure of human insulin has two chains:
- CHAIN 1: GIVEQ CCTSI CSLYQ LENYC N
- CHAIN 2: FVNQH LCGSH LVEAL YLVCG ERGFF YTPKT
Insulin
- Preproinsulin is synthesized in the RER of pancreatic β cells.
- The "presignal" is cleaved, resulting in proinsulin formation.
- Proinsulin is stored in secretory granules.
- Proinsulin is cleaved, resulting in the exocytosis of insulin and C-peptide equally.
- Elevated levels of both insulin and C-peptide are seen in endogenous insulin secretion (e.g., type 2 DM, insulin secretagogues, insulinoma), whereas exogenous insulin lacks C-peptide.
- Insulin is synthesized in the pancreas and cleared by both the liver and kidneys.
Protein Secondary Structure
- Secondary structure defines the configurational relationships between residues about 3-4 amino acids apart in linear structure.
- It is stabilized by non-covalent bonding.
- Secondary structures are non-linear and 3-dimensional.
- Secondary structures are localized to regions of an amino acid chain.
- They form and are stabilized by hydrogen bonding, electrostatic interactions, and van der Waals interactions.
Alpha Helix
- It is a spiral structure composed of polypeptides that forms the backbone and side chains of amino acids extending between NH and C=O groups.
- It's the most common and stable conformation of a polypeptide chain.
- Abundant in hemoglobin and myoglobin and absent in chymotrypsin.
- Proline and hydroxyproline will not allow the alpha -helix.
Beta Pleated Sheet
- The polypeptide is almost fully extended.
- Hydrogen bonds between NH and C=O groups of neighboring polypeptide segments stabilize it.
- Adjacent strands can run in the same direction (parallel) or opposite direction (anti-parallel) with regard to the amino and carboxy terminal.
Collagen Triple Helix
- Its amino acid sequence is Gly-X-Y repeating structure
- And has 2º structure stabilized by interchain hydrogen
Tertiary Structure
- Non-linear and 3 DIMENSIONAL
- It is global but restricted to the amino acid polymer
- Formed and stabilized by hydrogen bonding and non-covalent interactions toward hydrophobic packing towards solvents.
Quaternary Structure
- Certain polypeptides aggregate to form one functional unit.
- The structure is non-linear.
- It is global and across distinct amino acid polymers
- Formed by hydrogen bonding, covalent bonding, hydrophobic packing, and hydrophilic exposure.
Hemoglobin Structure
- Hemoglobin structure is stabilized by H-bonding, electrostatic bonds, hydrophobic interactions, and Van Der Walls forces.
- Each polypeptide chain is termed a subunit or monomer.
- Hemoglobin is made of 2 α subunits and 2 β subunits.
Extracelluar Pro-Collagen
- Hydroxylation of proline and lysine in collagen requires a di-oxygenase with Fe and requires Vitamin C keeps the iron reduced.
- Glycosylation – hydroxylysine with glucose is needed
- Spontaneous disulfide bond formation at the C-terminal peptides and the Golgi for assembly
Crosslinks in Collagen
- Cross links are formed by lysyl/prolyl oxidase requires copper as a co enzyme
- Oxidative deamination of lysines and hydroxylysines forms Allysine (aldehyde) This reacts with amino group of a nearby lysine or hydroxylysine to form interchain cross-link Which is important for collagen tensil strength
Cross Linking
- Excessive cross links cause problems in OLD AGE and result in the Hardening of ligaments (STIFF) and Prone to tear
- Whereas less cross-linking leads to Weak collagen and Menke's disease
Synthesis of Collagen
- Collagen is synthesized with translation of Gly-X-Y Usually pro, lys, or hydro
- It needs hydroxylization which needs vitamin C - deficiency is scurvy
- needs Glycosulation problems is it needs to osteogenesis imperfecto triple helix problems
- Exocytosis , alignment and crosslinked
- problems with cross will leads Menkes disease - lysyl oxidate
Scab - Collagen Types
- Type 1 bone and tendons Type 2 Cartlidge Type 3 arteries (eee = 3e's) Type 4 bm basement membranes floors.
Osteogenesis Imperfecta
- Genetic bone disorder (brittle bone caused by a variety of gene defects (most commonly COLIAI and COLIA2). Most common form is autosomal dominant
- Patients can't BITE: Bones = multiple fractures, (eye) = blue sclerae, Teeth = dental imperfections, Ear = hearing loss
Elhers -Danilo Syndrome
- Genetic Collaged is faulty
- can be caused to be hyper extinsible for a mutation in Collagen v
Elastin
- 3D chains that are linked
- lysyl oxidase is needed
- desmoes account for elastic
Elastin Structure Function
- Elastin inter converts number or de conformation ( dis disordered)
- Crosslinking is less Stable returns to deconsformatn
Elasin Criss-linking
- Lysinonoreudine and Desmozine - some lysed oxidized requires
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.