Podcast
Questions and Answers
What characterizes Type I respiratory failure?
What characterizes Type I respiratory failure?
- Inadequate ventilation due to muscular dysfunction
- Inability to remove CO2 from the blood effectively
- Disruption of O2 transport from the alveolus to arterial flow (correct)
- Stimulation of respiration is impaired
Which condition is associated with Type II respiratory failure?
Which condition is associated with Type II respiratory failure?
- Pneumonia
- Chronic obstructive pulmonary disease (COPD) (correct)
- Acute respiratory distress syndrome (ARDS)
- Aspiration pneumonia
What defines the process of ventilation in the respiratory system?
What defines the process of ventilation in the respiratory system?
- Transport of gases between the alveoli and capillaries
- Mechanical act of moving air into and out of the respiratory tree (correct)
- Chemical exchange of carbon dioxide and oxygen
- Diffusion of oxygen into the bloodstream
What is a major consequence of impaired respiration in Type I respiratory failure?
What is a major consequence of impaired respiration in Type I respiratory failure?
Which of the following is an advantage of nasal oxygen delivery?
Which of the following is an advantage of nasal oxygen delivery?
What is a significant disadvantage of low-flow oxygen devices?
What is a significant disadvantage of low-flow oxygen devices?
Which outcome is NOT typically a desired result of mechanical ventilation?
Which outcome is NOT typically a desired result of mechanical ventilation?
What complication is most strongly associated with mechanical ventilation?
What complication is most strongly associated with mechanical ventilation?
What does high-flow oxygen therapy aim to achieve?
What does high-flow oxygen therapy aim to achieve?
Which device is used for non-invasive mechanical ventilation?
Which device is used for non-invasive mechanical ventilation?
What is a primary role of nutritional support in mechanically ventilated patients?
What is a primary role of nutritional support in mechanically ventilated patients?
During intubation, what critical parameter must be monitored by the nurse?
During intubation, what critical parameter must be monitored by the nurse?
What type of ventilation does not guarantee improved gas exchange?
What type of ventilation does not guarantee improved gas exchange?
What defines hypoxemia?
What defines hypoxemia?
Which condition can result from high pressure during mechanical ventilation?
Which condition can result from high pressure during mechanical ventilation?
Flashcards
Acute Respiratory Failure (ARF)
Acute Respiratory Failure (ARF)
A condition where the lungs cannot exchange oxygen and carbon dioxide effectively.
Type I Respiratory Failure
Type I Respiratory Failure
Hypoxemic failure due to impaired oxygen transport from alveoli to arterial blood.
Type II Respiratory Failure
Type II Respiratory Failure
Hypercapnic failure caused by inadequate ventilation and CO2 clearance.
Ventilation vs. Respiration
Ventilation vs. Respiration
Signup and view all the flashcards
Nasal Cannula
Nasal Cannula
Signup and view all the flashcards
FiO2
FiO2
Signup and view all the flashcards
High-flow oxygen therapy
High-flow oxygen therapy
Signup and view all the flashcards
Mechanical ventilation
Mechanical ventilation
Signup and view all the flashcards
Intubation
Intubation
Signup and view all the flashcards
Tracheostomy
Tracheostomy
Signup and view all the flashcards
Ventilator-associated pneumonia (VAP)
Ventilator-associated pneumonia (VAP)
Signup and view all the flashcards
Hypoxemia
Hypoxemia
Signup and view all the flashcards
Cyanosis
Cyanosis
Signup and view all the flashcards
Asphyxia
Asphyxia
Signup and view all the flashcards
Nutritional support in critical care
Nutritional support in critical care
Signup and view all the flashcards
Study Notes
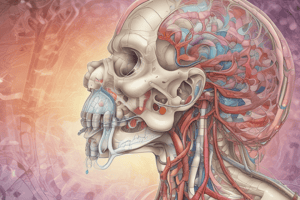
Acute Respiratory Failure (ARF)
- ARF is a critical care disorder where the lungs fail to adequately exchange oxygen and remove carbon dioxide.
- ALI (acute lung injury) and ARDS (acute respiratory distress syndrome) are severe forms of ARF, characterized by diffuse alveolar damage and profound hypoxia.
- Nurses must differentiate between ventilation (mechanical air movement) and respiration (gas exchange).
Types of Respiratory Failure
- Type I (hypoxemic): Impaired O2 transport from alveoli to blood. Causes include pneumonia, cardiogenic edema, ARDS, aspiration, and atelectasis. Associated with Impaired Gas Exchange.
- Type II (hypoxemic hypercapneic): Insufficient ventilation, often due to lung disease (COPD), neurological issues (narcotic overdose, head injury), muscular weakness, or skeletal abnormalities. CO2 builds up (hypercapnea) alongside low oxygen (hypoxemia).
Oxygen Therapy Devices
- Nasal cannula: Simple, low-flow device. Delivers O2 up to 6 LPM, but FiO2 (fractional inspired oxygen) is unpredictable.
- Simple face mask: Delivers higher FiO2 (8-12 LPM), but FiO2 is still affected by patient breathing.
- High-flow devices: Deliver oxygen at a rate exceeding the patient's inspiratory flow. Room air is mixed in less. Can create an oxygen reservoir. Includes wide nasal cannulas, nasal pillows, and face masks.
Mechanical Ventilation
- Mechanical ventilation assists individuals unable to breathe independently.
- Noninvasive (NIV) and invasive methods exist.
- NIV shows gas exchange improvement within 15 minutes.
- Invasive mechanical ventilation uses positive pressure via tubes (nasotracheal, endotracheal, tracheostomy).
Intubation Procedure
- Nasotracheal/Endotracheal tubes establish a patent airway.
- Monitoring O2 saturation (SaO2) during intubation is key. SaO2 below 90% halts the procedure, requiring manual ventilation.
- Post-intubation, auscultation ensures proper tube placement (air should be heard bilaterally).
Tracheostomy
- A tracheostomy is for patients requiring long-term ventilation (>21 days) or airway protection.
Complications of Mechanical Ventilation
- Ventilator-Associated Pneumonia (VAP): A significant complication, preventable by nursing interventions.
- Ventilator-Induced Lung Injury (VILI): Caused by excessive pressure (barotrauma) or excessive volume (volutrauma).
Nutrition in Critical Care
- Early enteral nutrition is preferred over parenteral nutrition.
- Special nutritional formulas may be necessary to address compromised organ systems (protein supplements and probiotics).
Oxygen Therapy: General Information
- Oxygen is essential for cell metabolism and tissue oxygenation.
- Oxygen is used to maintain cellular oxygenation and treat acute/chronic respiratory conditions.
- Oxygen delivery methods vary based on the patient's needs.
Hypoxemia and Related Symptoms
- Hypoxemia is inadequate blood oxygen levels. Causes include hypovolemia, hypoventilation, and issues with arterial flow.
- Cyanosis (bluish skin/mucous membranes) is caused by low blood oxygen.
- Breathlessness can be caused by various diseases (asthma, pulmonary embolism, cardiac insufficiency), high altitudes, anemia, lung diseases (pulmonary edema, pneumonia), and other conditions.
Signs and Symptoms of Respiratory Distress & Hypoxemia
- Early signs: Tachypnea, restlessness, pallor, anxiety.
- Late signs: Confusion, cyanosis, bradycardia, hypotension, cardiac dysrhythmias.
Nursing Interventions for Oxygen Therapy
- Assess and monitor for hypoxemia signs and symptoms.
- Apply oxygen delivery devices per order.
- Monitor O2 saturation (SaO2).
- Position patient for optimal breathing.
- Maintain good oral hygiene.
- Document the patient's response.
- Monitor skin integrity and provide appropriate care.
- Educate patient and family.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.