Podcast
Questions and Answers
Which of the following best describes the pathophysiology of acute pancreatitis?
Which of the following best describes the pathophysiology of acute pancreatitis?
- Infection of the liver parenchyma
- Reflux of gastric contents into the esophagus
- Inflammation of the gallbladder due to bile stasis
- Premature activation of pancreatic enzymes leading to autodigestion (correct)
What is the result of pancreatic enzyme activation within the pancreas?
What is the result of pancreatic enzyme activation within the pancreas?
- Gallbladder constriction
- Obstruction of the small intestine
- Pancreatic tissue digestion and inflammation (correct)
- Liver necrosis
A nurse suspects acute pancreatitis in a patient. Which assessment finding would support this?
A nurse suspects acute pancreatitis in a patient. Which assessment finding would support this?
- Severe epigastric pain radiating to the back (correct)
- Constant headache with fever
- Sharp right lower quadrant pain
- Painless jaundice
Which of the following processes are involved in the pathophysiology of pancreatitis? (Select all that apply)
Which of the following processes are involved in the pathophysiology of pancreatitis? (Select all that apply)
A patient develops multi-organ failure after being admitted with pancreatitis. What is the most likely underlying cause?
A patient develops multi-organ failure after being admitted with pancreatitis. What is the most likely underlying cause?
A nurse explains to a student that the pancreas can digest itself in pancreatitis. What causes this?
A nurse explains to a student that the pancreas can digest itself in pancreatitis. What causes this?
Which structure is involved in the backflow that contributes to pancreatitis?
Which structure is involved in the backflow that contributes to pancreatitis?
Why is chronic steroid use a risk factor for pancreatitis?
Why is chronic steroid use a risk factor for pancreatitis?
What is the most common cause of acute pancreatitis?
What is the most common cause of acute pancreatitis?
A nurse is reviewing a patient's chart and notes heavy alcohol use. The nurse understands that alcohol increases the risk for pancreatitis by:
A nurse is reviewing a patient's chart and notes heavy alcohol use. The nurse understands that alcohol increases the risk for pancreatitis by:
Which patient is at highest risk for developing pancreatitis?
Which patient is at highest risk for developing pancreatitis?
Which of the following are risk factors for pancreatitis? (Select all that apply)
Which of the following are risk factors for pancreatitis? (Select all that apply)
A nurse is educating a client with chronic pancreatitis. The client asks, “Why did this happen to me?” Which response best reflects the pathogenesis?
A nurse is educating a client with chronic pancreatitis. The client asks, “Why did this happen to me?” Which response best reflects the pathogenesis?
A pregnant client in her third trimester presents with upper abdominal pain and nausea. The provider suspects pancreatitis. What is the best initial nursing action?
A pregnant client in her third trimester presents with upper abdominal pain and nausea. The provider suspects pancreatitis. What is the best initial nursing action?
A nurse is analyzing hospital trends and notices an increase in pancreatitis cases. What trend could account for this?
A nurse is analyzing hospital trends and notices an increase in pancreatitis cases. What trend could account for this?
Which sign is specific for acute pancreatitis and appears as bluish discoloration around the umbilicus?
Which sign is specific for acute pancreatitis and appears as bluish discoloration around the umbilicus?
What is a common skin finding in a patient with acute pancreatitis?
What is a common skin finding in a patient with acute pancreatitis?
Which clinical signs indicate acute pancreatitis? (Select all that apply)
Which clinical signs indicate acute pancreatitis? (Select all that apply)
A patient with suspected acute pancreatitis is admitted. Which symptom would the nurse prioritize for monitoring?
A patient with suspected acute pancreatitis is admitted. Which symptom would the nurse prioritize for monitoring?
A nurse assesses Cullen's sign on a patient. What complication of pancreatitis does this suggest?
A nurse assesses Cullen's sign on a patient. What complication of pancreatitis does this suggest?
What is the cause of steatorrhea in chronic pancreatitis?
What is the cause of steatorrhea in chronic pancreatitis?
A nurse assesses a patient with chronic pancreatitis. The patient reports LUQ pain after eating a fatty meal and recent weight loss. What should the nurse suspect?
A nurse assesses a patient with chronic pancreatitis. The patient reports LUQ pain after eating a fatty meal and recent weight loss. What should the nurse suspect?
Which complication of chronic pancreatitis results from damage to the islet of Langerhans?
Which complication of chronic pancreatitis results from damage to the islet of Langerhans?
Which findings are more consistent with chronic pancreatitis? (Select all that apply)
Which findings are more consistent with chronic pancreatitis? (Select all that apply)
A patient reports dark urine and yellowing of the skin. These symptoms are most likely due to:
A patient reports dark urine and yellowing of the skin. These symptoms are most likely due to:
A patient with chronic pancreatitis is admitted. Which symptom requires the nurse's immediate attention?
A patient with chronic pancreatitis is admitted. Which symptom requires the nurse's immediate attention?
Which clinical scenario best demonstrates a progression from acute to chronic pancreatitis?
Which clinical scenario best demonstrates a progression from acute to chronic pancreatitis?
Which of the following is a potential life-threatening complication of acute pancreatitis?
Which of the following is a potential life-threatening complication of acute pancreatitis?
Which complications can occur due to chronic pancreatitis? (Select all that apply)
Which complications can occur due to chronic pancreatitis? (Select all that apply)
A nurse is caring for a patient with a known pancreatic pseudocyst. The patient suddenly reports sharp abdominal pain and dizziness. What is the priority nursing action?
A nurse is caring for a patient with a known pancreatic pseudocyst. The patient suddenly reports sharp abdominal pain and dizziness. What is the priority nursing action?
Which clinical sign would most likely indicate the development of a pancreatic abscess?
Which clinical sign would most likely indicate the development of a pancreatic abscess?
How does chronic pancreatitis contribute to malabsorption?
How does chronic pancreatitis contribute to malabsorption?
A client is diagnosed with multi-organ dysfunction from severe pancreatitis. What assessment findings would support this complication?
A client is diagnosed with multi-organ dysfunction from severe pancreatitis. What assessment findings would support this complication?
Which imaging test uses a magnetic technique to visualize the biliary and pancreatic ducts?
Which imaging test uses a magnetic technique to visualize the biliary and pancreatic ducts?
Which lab value would most likely be elevated in a patient with pancreatitis?
Which lab value would most likely be elevated in a patient with pancreatitis?
A patient presents with abdominal pain and nausea. Labs show elevated amylase and lipase. Which condition is most likely?
A patient presents with abdominal pain and nausea. Labs show elevated amylase and lipase. Which condition is most likely?
Which diagnostic tests may be used to evaluate suspected pancreatitis? (Select all that apply)
Which diagnostic tests may be used to evaluate suspected pancreatitis? (Select all that apply)
A provider orders an ERCP for a client with suspected gallstone pancreatitis. What risk should the nurse monitor for after this procedure?
A provider orders an ERCP for a client with suspected gallstone pancreatitis. What risk should the nurse monitor for after this procedure?
Which intervention is essential in the early management of acute pancreatitis?
Which intervention is essential in the early management of acute pancreatitis?
What are priority interventions for a patient with acute pancreatitis? (Select all that apply)
What are priority interventions for a patient with acute pancreatitis? (Select all that apply)
A client with acute pancreatitis is vomiting and unable to tolerate oral intake. The nurse should anticipate which intervention?
A client with acute pancreatitis is vomiting and unable to tolerate oral intake. The nurse should anticipate which intervention?
Why are proton pump inhibitors (PPIs) or H2 antagonists used in pancreatitis care?
Why are proton pump inhibitors (PPIs) or H2 antagonists used in pancreatitis care?
A nurse is teaching a client with chronic pancreatitis about dietary changes. Which of the following statements indicates correct understanding?
A nurse is teaching a client with chronic pancreatitis about dietary changes. Which of the following statements indicates correct understanding?
A patient with alcohol-induced chronic pancreatitis is admitted. Which collaborative intervention is most important to initiate early?
A patient with alcohol-induced chronic pancreatitis is admitted. Which collaborative intervention is most important to initiate early?
A client with chronic pancreatitis is scheduled for a pancreatectomy. Which nursing goal is most appropriate pre-operatively?
A client with chronic pancreatitis is scheduled for a pancreatectomy. Which nursing goal is most appropriate pre-operatively?
Flashcards
Pathophysiology of Acute Pancreatitis
Pathophysiology of Acute Pancreatitis
Premature activation of pancreatic enzymes leading to autodigestion of the pancreas.
Result of Pancreatic Enzyme Activation
Result of Pancreatic Enzyme Activation
Digestion and inflammation of pancreatic tissue, potentially leading to necrosis.
Assessment Finding for Acute Pancreatitis
Assessment Finding for Acute Pancreatitis
Severe epigastric pain that radiates to the back.
Processes in Pancreatitis Pathophysiology
Processes in Pancreatitis Pathophysiology
Signup and view all the flashcards
Cause of Multi-Organ Failure
Cause of Multi-Organ Failure
Signup and view all the flashcards
Why Pancreas Digests Itself
Why Pancreas Digests Itself
Signup and view all the flashcards
Role of Sphincter of Oddi
Role of Sphincter of Oddi
Signup and view all the flashcards
Risk Factor: Steroid Use
Risk Factor: Steroid Use
Signup and view all the flashcards
Most Common Cause of Acute Pancreatitis
Most Common Cause of Acute Pancreatitis
Signup and view all the flashcards
How Alcohol Causes Pancreatitis
How Alcohol Causes Pancreatitis
Signup and view all the flashcards
Highest Risk for Pancreatitis
Highest Risk for Pancreatitis
Signup and view all the flashcards
Why Chronic Pancreatitis Occurs
Why Chronic Pancreatitis Occurs
Signup and view all the flashcards
Initial Nursing Action
Initial Nursing Action
Signup and view all the flashcards
Trend: Pancreatitis Cases
Trend: Pancreatitis Cases
Signup and view all the flashcards
Cullen's Sign
Cullen's Sign
Signup and view all the flashcards
Common Skin Finding
Common Skin Finding
Signup and view all the flashcards
Clinical Signs: Acute Pancreatitis
Clinical Signs: Acute Pancreatitis
Signup and view all the flashcards
Cullen's Sign Suggests:
Cullen's Sign Suggests:
Signup and view all the flashcards
Intervention for Vomiting Patient
Intervention for Vomiting Patient
Signup and view all the flashcards
Why PPIs or H2 Antagonists
Why PPIs or H2 Antagonists
Signup and view all the flashcards
Study Notes
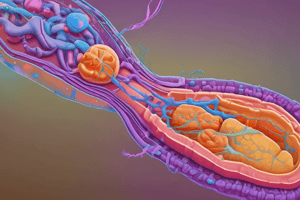
Pathophysiology of Acute Pancreatitis
- Acute pancreatitis pathophysiology is best described as the premature activation of pancreatic enzymes, leading to autodigestion
- Pancreatic enzyme activation within the pancreas results in pancreatic tissue digestion, inflammation, and potential necrosis
- Severe epigastric pain radiating to the back is a hallmark assessment finding for acute pancreatitis
- Processes involved are Hemorrhage, Necrosis, and Reflux through the Sphincter of Oddi
- Pancreatic necrosis can release inflammatory mediators, leading to multi-organ dysfunction
- Pancreatitis is caused by the premature activation of enzymes in the pancreas, causing self-digestion
- Reflux through a distended Sphincter of Oddi can cause premature enzyme activation in the pancreas
- Chronic steroid use is a risk factor because it can lead to hyperlipidemia and fat metabolism issues, contributing to pancreatic inflammation
Etiology, Incidence, and Risk Factors
- Gallstones are the number one cause of acute pancreatitis due to blockage of pancreatic ducts
- Heavy alcohol use increases pancreatitis risk by stimulating pancreatic enzyme production and causing ductal injury
- A 35-year-old female in her third trimester of pregnancy with a history of gallstones is at highest risk for developing pancreatitis
- Risk factors include infections, gallbladder disease, pregnancy, and steroid use
- Chronic pancreatitis commonly is related to repeated inflammation from alcohol use or duct obstruction, leading to irreversible damage
- For suspected pancreatitis in a pregnant client in their third trimester, notify the provider and initiate NPO status
- An increase in gallstone-related admissions can lead to more pancreatitis cases
Clinical Manifestations – Acute & Chronic Pancreatitis
- Cullen’s sign involves periumbilical bruising specific to acute pancreatitis, and is a classic sign of intra-abdominal bleeding
- A common skin finding in a patient with acute pancreatitis is cool, pale, and moist skin due to shock or systemic inflammation
- Clinical signs indicating acute pancreatitis include severe epigastric pain radiating to the back, mild jaundice, bruising on the flanks, and abdominal distention with decreased bowel sounds
- A nurse should prioritize monitoring epigastric pain radiating to the back for acute pancreatitis
- Cullen’s sign suggests retroperitoneal hemorrhage, a serious complication of acute pancreatitis
- Decreased enzyme secretion impairs fat digestion, leading to fatty stools (steatorrhea)
- LUQ pain after eating a fatty meal and recent weight loss, points to fat malabsorption due to decreased enzyme production in chronic pancreatitis
- Damage to the islet cells from chronic pancreatitis leads to impaired insulin secretion, resulting in diabetes
- Findings that are more consistent with chronic pancreatitis include LUQ abdominal pain, steatorrhea, weight loss, and DM
- Bile accumulation from impaired drainage causes jaundice and dark urine
- A blood glucose of 320 mg/dL suggests uncontrolled diabetes and requires prompt intervention
- Recurrent LUQ pain and steatorrhea after fatty meals indicates pancreatic dysfunction characteristic of chronic pancreatitis
Complications
- Pancreatic necrosis involves tissue death and can lead to systemic infection, sepsis, and multi-organ failure (life-threatening)
- Complications that can occur due to chronic pancreatitis include malabsorption, diabetes mellitus, pancreatic pseudocyst, and respiratory distress
- Notify the provider immediately for a patient with a known pancreatic pseudocyst who suddenly reports sharp abdominal pain and dizziness because it is a medical emergency of cyst rupture or hemorrhage
- A pancreatic abscess presents with signs of localized infection as indicated by fever, elevated WBCs, and increasing abdominal pain
- Impaired enzyme production in chronic pancreatitis leads to poor digestion and absorption of fats
- Confusion, decreased urine output, and jaundice are classic indicators of multi-organ involvement
Diagnostics & Laboratory Findings
- MRCP (Magnetic Resonance Cholangiopancreatography) uses a magnetic technique to visualize the biliary and pancreatic ducts
- Amylase (and lipase) are key pancreatic enzymes that are elevated during acute inflammation
- Elevated pancreatic enzymes, especially amylase and lipase, are classic markers of acute pancreatitis
- Diagnostic tests to evaluate suspected pancreatitis include CT scan, MRCP, ERCP, and ultrasound
- ERCP is invasive and may cause post-procedure pancreatitis or introduce infection due to duct manipulation
Nursing & Collaborative Interventions
- Maintaining NPO status is essential for the early management of acute pancreatitis, allowing the pancreas to rest
- Priority interventions for a patient with acute pancreatitis include IV hydration, pain control, gut rest (NG tube), and nutritional support
- TPN may be initiated when oral intake is not possible to meet nutritional needs while resting the pancreas
- PPIs reduce gastric acid secretion, which helps decrease pancreatic stimulation
- A statement that indicates correct understanding of dietary changes is to avoid alcohol and fatty foods completely
- An alcohol withdrawal protocol is crucial to prevent or manage life-threatening complications in hospitalized patients
- Maintain strict NPO status and manage pain pre-operatively because pre-op care focuses on gut rest and pain control
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.