Podcast
Questions and Answers
What are the three phases of healing that decision-making should align with after repair of tendons?
What are the three phases of healing that decision-making should align with after repair of tendons?
- Inflammatory, fibroplasia, remodelling (correct)
- Inflammation, fibrosis, restructuring
- Infection, fibroplasia, renovation
- Inflammatory, fibrosis, remodeling
What is classified as 'early' motion following flexor injury?
What is classified as 'early' motion following flexor injury?
- 0–5 days
- 4–5 days (correct)
- 5–10 days
- 1–2 weeks
Which tendon excursion issue is likely to increase after repair or re-insertion in zone I of the flexor digitorum profundus tendon?
Which tendon excursion issue is likely to increase after repair or re-insertion in zone I of the flexor digitorum profundus tendon?
- Joint instability
- Muscle atrophy
- Adhesion formation (correct)
- Ligament laxity
What type of regimen is considered unsuitable for a vulnerable repair in zone I of the flexor digitorum profundus tendon?
What type of regimen is considered unsuitable for a vulnerable repair in zone I of the flexor digitorum profundus tendon?
What undesirable consequence can occur after injury and surgery at zone I of the flexor digitorum profundus tendon?
What undesirable consequence can occur after injury and surgery at zone I of the flexor digitorum profundus tendon?
Which factor influences decision-making after tendon repair based on an individual's response to injury and the severity of soft tissue and bone involvement?
Which factor influences decision-making after tendon repair based on an individual's response to injury and the severity of soft tissue and bone involvement?
What is a crucial factor in determining the fate of flexor and extensor tendon systems?
What is a crucial factor in determining the fate of flexor and extensor tendon systems?
Which of the following complications may arise due to inadequate intervention in tendon injuries?
Which of the following complications may arise due to inadequate intervention in tendon injuries?
What is emphasized as being as crucial as the repair technique in tendon injuries?
What is emphasized as being as crucial as the repair technique in tendon injuries?
What has recent advances improved in the surgical and rehabilitation treatment of acute tendon injuries?
What has recent advances improved in the surgical and rehabilitation treatment of acute tendon injuries?
What plays a significant role in enhancing final outcomes following tendon repair?
What plays a significant role in enhancing final outcomes following tendon repair?
What is vital to determine safe splint position and motion progression during early phases of tendon healing?
What is vital to determine safe splint position and motion progression during early phases of tendon healing?
What is the recommended splint position for Zone 1 flexor tendon injuries?
What is the recommended splint position for Zone 1 flexor tendon injuries?
What is the primary objective of current rehabilitation regimens at Zone II level for tendon repairs?
What is the primary objective of current rehabilitation regimens at Zone II level for tendon repairs?
Why is a passive regimen considered a safer option in vulnerable repairs?
Why is a passive regimen considered a safer option in vulnerable repairs?
What should be avoided in the presence of nerve injury with zones 4 and 5 flexor tendon injuries?
What should be avoided in the presence of nerve injury with zones 4 and 5 flexor tendon injuries?
What should patients be discouraged from doing when there are injuries to the pulley system?
What should patients be discouraged from doing when there are injuries to the pulley system?
'Confining motion to the PIP joint only will encourage cross adherence' implies that this approach may lead to:
'Confining motion to the PIP joint only will encourage cross adherence' implies that this approach may lead to:
'The strength of the repair decreases as the angle of tension increases' suggests that high tension can:
'The strength of the repair decreases as the angle of tension increases' suggests that high tension can:
'One of the primary objectives of current rehabilitation regimens at this level is the preservation of differential tendon glide' implies that this preservation aims to:
'One of the primary objectives of current rehabilitation regimens at this level is the preservation of differential tendon glide' implies that this preservation aims to:
'Passive flexion must be restored before active digital flexion exercises are initiated' indicates that active motion should not start until:
'Passive flexion must be restored before active digital flexion exercises are initiated' indicates that active motion should not start until:
'Emphasise active DIP joint flexion to ensure tendon glide' highlights that focusing on DIP joint flexion helps prevent:
'Emphasise active DIP joint flexion to ensure tendon glide' highlights that focusing on DIP joint flexion helps prevent:
What amount of motion is needed to retain extensor tendon excursion after repair in zones 5–7 and T4–5 of the thumb?
What amount of motion is needed to retain extensor tendon excursion after repair in zones 5–7 and T4–5 of the thumb?
In which zones is immobilization crucial after extensor tendon repair?
In which zones is immobilization crucial after extensor tendon repair?
What is the focus of the Safe Controlled Motion (SCM) program in the first three postoperative weeks?
What is the focus of the Safe Controlled Motion (SCM) program in the first three postoperative weeks?
Which zones may result in significant extension lag even with minimal tendon attenuation?
Which zones may result in significant extension lag even with minimal tendon attenuation?
What is the purpose of active hold (place and hold) during rehabilitation after extensor tendon repair?
What is the purpose of active hold (place and hold) during rehabilitation after extensor tendon repair?
Which factor equates with loss of active extension after extensor tendon gapping?
Which factor equates with loss of active extension after extensor tendon gapping?
What is a common concern for patients with injuries involving zones F1–2?
What is a common concern for patients with injuries involving zones F1–2?
When does Safe Splint Position (SSP) need to be established for all zones?
When does Safe Splint Position (SSP) need to be established for all zones?
How should the MP joints be positioned to facilitate digital flexion and inhibit the development of claw deformity in injuries involving finger tendons and nerve injuries?
How should the MP joints be positioned to facilitate digital flexion and inhibit the development of claw deformity in injuries involving finger tendons and nerve injuries?
Which position is generally considered the best compromise in splinting the wrist post-injury to prevent tension on nerve repair?
Which position is generally considered the best compromise in splinting the wrist post-injury to prevent tension on nerve repair?
What is the primary concern with wrist extension post-injury in relation to tendon prolapse?
What is the primary concern with wrist extension post-injury in relation to tendon prolapse?
In zone IV injuries, what type of lacerations are not common?
In zone IV injuries, what type of lacerations are not common?
What is the main purpose of positioning the MP joints in 60°–70° of flexion post-injury?
What is the main purpose of positioning the MP joints in 60°–70° of flexion post-injury?
Why should adhesions between tendons be prevented after surgery?
Why should adhesions between tendons be prevented after surgery?
What is a potential consequence of significant intrinsic muscle involvement in injuries?
What is a potential consequence of significant intrinsic muscle involvement in injuries?
What is crucial in preventing claw deformity and achieving a greater range of IP joint flexion post-injury?
What is crucial in preventing claw deformity and achieving a greater range of IP joint flexion post-injury?
What approach is recommended if there is doubt about the ability of a repair to withstand active motion post-surgery?
What approach is recommended if there is doubt about the ability of a repair to withstand active motion post-surgery?
What should be included in the rehabilitation regimen for zone V injuries involving neurovascular structures?
What should be included in the rehabilitation regimen for zone V injuries involving neurovascular structures?
What splint position is recommended for zone F7 injuries according to the provided text?
What splint position is recommended for zone F7 injuries according to the provided text?
What is essential for the surgeon to avoid in relation to tendon excursion after resecting part of the retinaculum?
What is essential for the surgeon to avoid in relation to tendon excursion after resecting part of the retinaculum?
Which injuries should be treated using the relative motion extension yoke splint?
Which injuries should be treated using the relative motion extension yoke splint?
What is emphasized as having the greatest impact on the final outcome after tendon repair according to the text?
What is emphasized as having the greatest impact on the final outcome after tendon repair according to the text?
What is advised as the standard rehabilitation program for most repaired tendon injuries?
What is advised as the standard rehabilitation program for most repaired tendon injuries?
For extensor tendon repairs, what method is suggested due to the lack of standard protocols according to the text?
For extensor tendon repairs, what method is suggested due to the lack of standard protocols according to the text?
What is the purpose of combining DIP extension with 20° of PIP flexion in a splint?
What is the purpose of combining DIP extension with 20° of PIP flexion in a splint?
Which type of injury often requires immobilization for 6–12 weeks, regardless of repair?
Which type of injury often requires immobilization for 6–12 weeks, regardless of repair?
What deformity results from failure to repair or position the PIP joint properly after injuries in zones F3 and T3–4?
What deformity results from failure to repair or position the PIP joint properly after injuries in zones F3 and T3–4?
What happens when there is a loss of central tendon integrity in zone 3 injuries?
What happens when there is a loss of central tendon integrity in zone 3 injuries?
In zone T3–4 injuries, what contributes to the development of a boutonnière deformity?
In zone T3–4 injuries, what contributes to the development of a boutonnière deformity?
What is encouraged in the first 0–5 days postoperative period for zone F3 central tendon division?
What is encouraged in the first 0–5 days postoperative period for zone F3 central tendon division?
What is essential to limit tendon excursion in zones 4–7 after repair?
What is essential to limit tendon excursion in zones 4–7 after repair?
What is the primary function of the relative motion extension yoke splint?
What is the primary function of the relative motion extension yoke splint?
Why is the relative motion extension yoke splint unsuitable when all EDC, EIP, and EDM have been repaired?
Why is the relative motion extension yoke splint unsuitable when all EDC, EIP, and EDM have been repaired?
What happens during immediate splint controlled motion (ICAM) using the relative motion extension yoke splint?
What happens during immediate splint controlled motion (ICAM) using the relative motion extension yoke splint?
Study Notes
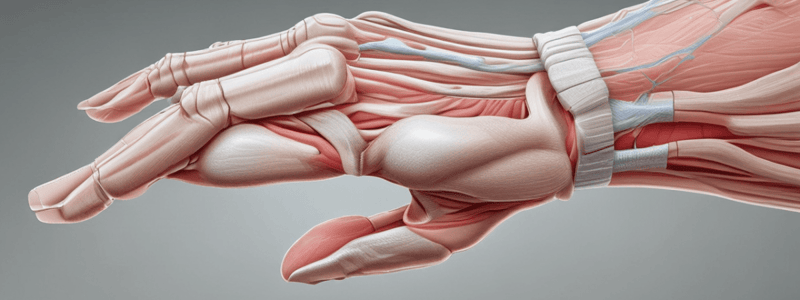
Flexor Tendon Rehabilitation
- Surgeon's assessment of repair quality, motion in adjacent joints, and individual's biological response influence decision-making for splint design and early motion.
- Decision-making should align with phases of healing: inflammatory (0-5 days), fibroplasia (3-21 days), and remodelling (21 days-3 months).
Zone I Flexor Tendon Rehabilitation
- Open lacerations of FDP tendon in zone I are subdivided into three levels: under A4 pulley, just distal to A4 pulley, and at or close to the insertion.
- Exercises focus on achieving passive, followed by active, distal interphalangeal joint (DIP) motion.
- Undesirable consequences of injury and surgery at this level include tendon tethering and DIP joint flexion deformity.
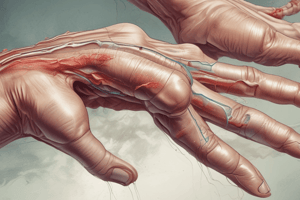
Zone II Flexor Tendon Rehabilitation
- Immobilization for 6-12 weeks is common for F1-2 injuries.
- The safe splint position (SSP) in the 0-5 days period immobilizes the IP in hyperextension, with MP motion unloading the EPL repair during motion through the intrinsic muscle insertions into the extensor apparatus.
Zone III and IV Flexor Tendon Rehabilitation
- A boutonnière deformity results from failure to repair or properly position the PIP joint after injuries in zones F3 and T3-4.
- The SSP in the 0-5 days period for the zone F3 central tendon (CT) division, with or without lateral band (LB) involvement, is with the PIP and DIP immobilized in neutral extension.
Zone IV Flexor Tendon Rehabilitation
- Tendon excursion in zones 4-7 is greatest, necessitating controlled motion after repair to discourage adhesions.
- The relative motion, or immediate controlled active motion (ICAM), splint is effective in limiting excursion of the tendon repaired in zones 4-7.
Extensor Tendon Rehabilitation
- Normal tendon excursion in proximal digit zones is greater than in distal zones.
- The estimated amount of motion needed to retain extensor tendon excursion after repair is 5 mm in zones 5-7 and T4-5 of the thumb and 4 mm in zones F3-4.
- Adhesions become obstacles to tendon excursion in some zones, with immediate to early motion essential to regain normal excursion.
Safe Splint Position (SSP) and Splint Controlled Motion (SCM)
- SSP shields the repair from gapping forces and must be established at the time of repair or within 5 days for all zones.
- SCM commences during the first three postoperative weeks in all zones, with out-of-splint controlled motion exercises starting after 3 weeks for most zones.
- The purpose of SCM is safe tendon excursion, distally and proximally, and active motion is preferable as it produces greater tendon excursion and is more effective in preventing adhesions and preserving motion.### Zone F4–6 and F7 Extensor Tendon Decision Algorithm
- The algorithm ensures safe splint position and controlled motion progression during the first 3 postoperative weeks.
- The wrist retinaculum can limit tendon excursion in all extensor compartments, and surgeons must resect part of the retinaculum to avoid this problem.
Wrist Retinaculum and Tendon Repairs
- Positioning the wrist in neutral or up to 20° extension prevents bunching of retinacular tendons during proximal excursion.
- The relative motion extension yoke splint is recommended for zone F7 injuries with the wrist in neutral, and for T5 EPL injuries with the wrist neutral and the thumb column in radial extension.
Decision-Making for Splint Controlled Motion (SCM)
- Decisions made within the first 3 weeks after tendon repair have the greatest impact on final outcome.
- Early motion requires clinicians to be informed, observant, and guided by goniometric measurement.
- Algorithms like Fig. 2, Fig. 3, and Fig. 4 can aid decision-making.
Rehabilitation and Tendon Repairs
- Immediate to early motion is the standard rehabilitation program for most repaired tendon injuries.
- Active motion regimens are ideal for flexor tendons in all zones, but not always suitable for extensor tendon repairs.
- There are no standard protocols for extensor tendon repairs, and therapists must communicate with surgeons and consider individual patient needs.
- Optimal tendon glide must not compromise safety.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Explore the critical decisions made by clinicians, surgical and rehabilitation treatments, and potential complications of acute flexor and extensor tendon injuries. Understand the importance of timely interventions to prevent deformity, loss of motion, and other functional limitations.