Podcast
Questions and Answers
What is the definition of congestive heart failure?
What is the definition of congestive heart failure?
- The pathophysiologic state in which the heart is unable to pump blood at a rate commensurate with the body's metabolic needs (correct)
- The pathophysiologic state in which the heart is unable to pump blood at a rate commensurate with the body's nutritional needs
- The pathophysiologic state in which the heart is unable to pump blood at a rate commensurate with the body's oxygen delivery needs
- The pathophysiologic state in which the heart is unable to pump blood at a rate commensurate with the body's fluid balance needs
What are the three factors that determine stroke volume?
What are the three factors that determine stroke volume?
- Preload, afterload, and contractility (correct)
- Preload, cardiac output, and heart rate
- Contractility, ejection fraction, and heart rate
- Preload, afterload, and heart rate
What is the main cause of congestive heart failure in a child under 1 year old?
What is the main cause of congestive heart failure in a child under 1 year old?
- Pulmonary hypertension
- Acquired heart disease
- Congenital heart disorder (correct)
- Myocardial infarction
What is the main cause of congestive heart failure in a child over 1 year old with no congenital anomaly?
What is the main cause of congestive heart failure in a child over 1 year old with no congenital anomaly?
Which of the following is not a symptom of systemic venous congestion in congestive heart failure?
Which of the following is not a symptom of systemic venous congestion in congestive heart failure?
What is the main mechanism by which the heart is unable to maintain adequate cardiac output in congestive heart failure?
What is the main mechanism by which the heart is unable to maintain adequate cardiac output in congestive heart failure?
What is a common presenting symptom of heart failure in neonates and infants?
What is a common presenting symptom of heart failure in neonates and infants?
Which diagnostic tool is used to assess heart chamber sizes and myocardial function accurately?
Which diagnostic tool is used to assess heart chamber sizes and myocardial function accurately?
What is the main function of Digitalis in the treatment of heart failure?
What is the main function of Digitalis in the treatment of heart failure?
Which of the following is NOT a part of the '4D's' approach to treating heart failure?
Which of the following is NOT a part of the '4D's' approach to treating heart failure?
What does Furosemide (Lasix) do in the treatment of heart failure?
What does Furosemide (Lasix) do in the treatment of heart failure?
When should an apical pulse be taken in relation to the administration of Digoxin?
When should an apical pulse be taken in relation to the administration of Digoxin?
Flashcards are hidden until you start studying
Study Notes
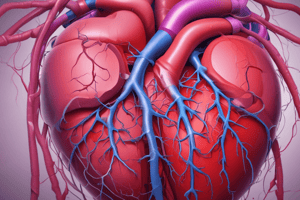
Congestive Heart Failure (CHF)
- Defined as a pathophysiologic state in which the heart is unable to pump blood at a rate commensurate with the body's metabolic needs.
- Inability to dispose of systemic or pulmonary venous return adequately, or a combination of both.
- Characterized by the heart's inability to maintain an adequate cardiac output.
Factors Affecting Cardiac Output
- Preload: volume of blood in the ventricle at the end of diastole.
- Afterload: pressure required to push blood into the arteries.
- Contractility: ventricles' ability to squeeze.
Clinical Manifestations
- Systemic Venous Congestion:
- Weight gain
- Hepatomegaly
- Edema
- Jugular vein distention
- Pulmonary Venous Congestion:
- Tachypnea
- Dyspnea
- Cough
- Wheezes
Compensatory Response
- Tachycardia
- Cardiomegaly
- Diaphoretic
- Fatigue
- Failure to grow
Assessment
- Clinical history:
- Neonates and infants: poor feeding, tachypnea, cold sweat on forehead, poor weight gain
- Older children: fatigue, exercise intolerance, dyspnea, puffy eyes and pedal edema, growth failure
Diagnostics
- Chest x-ray:
- Cardiomegaly
- Pulmonary edema
- ECG:
- Arrhythmias
- Echocardiogram:
- Assesses heart chamber sizes, measures myocardial function accurately, diagnoses congenital heart defects
- Pulse-oximetry, CBG, hyperoxia test, CBC, U&A, calcium, creatinine, LFT, thyroid function
Treatment
- Correct underlying causes of HF
- The 4D's:
- Diet (low salt, high calories)
- Digitalis (improves cardiac contractility)
- Diuretics (reduces preload)
- Dilators (reduces afterload)
- General Care:
- Rest
- Oxygenation
- Small frequent feeding
- Diet modification (sodium and fluid restriction)
- Treatment of underlying cause:
- Repair of congenital defects (VSD, ASD)
- Heart transplantation
Medications
- Diuretics:
- Furosemide (Lasix)
- Spironolactone/Aldactone
- Digitalis:
- Digoxin
- Dilators:
- ACE
- Hydralazine
- Nitroprusside
- Captopril
Digoxin Therapy
- Increases the force of the myocardial contraction
- Take an apical pulse with steth for 1 full min before every dose of digoxin
- If bradycardia is detected, withhold digoxin dose
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.