Podcast
Questions and Answers
What is the main difference between regeneration and repair?
What is the main difference between regeneration and repair?
- Regeneration is a slower process, whereas repair is a faster process
- Regeneration involves the formation of granulation tissue, whereas repair involves the formation of fibrous scar tissue
- Regeneration involves the proliferation of surrounding undamaged cells, whereas repair involves the formation of granulation tissue (correct)
- Regeneration is a response to minor injuries, whereas repair is a response to major injuries
What is the primary difference between primary and secondary intention healing?
What is the primary difference between primary and secondary intention healing?
- The width of the wound edges (correct)
- The presence of infection
- The size of the wound
- The type of tissue involved
Which stage of healing is characterized by the formation of a fibrin clot and is inhibited by aspirin and warfarin?
Which stage of healing is characterized by the formation of a fibrin clot and is inhibited by aspirin and warfarin?
- Haemostasis (correct)
- Granulation tissue formation
- Re-epithelialisation
- Inflammation
What is the main role of macrophages during the inflammatory stage of healing?
What is the main role of macrophages during the inflammatory stage of healing?
What is the primary mechanism by which the wound area is reduced during secondary intention healing?
What is the primary mechanism by which the wound area is reduced during secondary intention healing?
What is the duration of the granulation tissue formation stage of healing?
What is the duration of the granulation tissue formation stage of healing?
What is the primary function of macrophages in wound healing?
What is the primary function of macrophages in wound healing?
What is the result of collagen cross-linking in wound healing?
What is the result of collagen cross-linking in wound healing?
What is the primary factor affecting wound healing in Afro-Caribbean populations?
What is the primary factor affecting wound healing in Afro-Caribbean populations?
What is the primary function of fibroblasts in wound healing?
What is the primary function of fibroblasts in wound healing?
What is the primary complication of wound healing resulting in break down of the wound?
What is the primary complication of wound healing resulting in break down of the wound?
What is the primary factor affecting wound healing in patients with pre-existing medical conditions?
What is the primary factor affecting wound healing in patients with pre-existing medical conditions?
What is the primary function of endothelial cells in wound healing?
What is the primary function of endothelial cells in wound healing?
What is the primary difference between keloids and hypertrophic scarring?
What is the primary difference between keloids and hypertrophic scarring?
What is the primary systemic factor affecting wound healing?
What is the primary systemic factor affecting wound healing?
What is the primary local factor affecting wound healing?
What is the primary local factor affecting wound healing?
Flashcards are hidden until you start studying
Study Notes
Wound Healing
- Regeneration: replacement of lost or damaged tissue by that of a similar type, derived from the proliferation of surrounding undamaged cells.
- Repair: replacement of lost or damaged tissue by granulation tissue, which later matures into fibrous scar tissue.
Healing Routes
- Helpful route: healing
- Not helpful route: fibrosis/scar formation
Primary and Secondary Intention Healing
- Primary intention: wound is narrow, wound edges are in close apposition, re-epithelialisation dominates healing.
- Secondary intention: wound is more extensive, wound edges are widely separated, granulation tissue covers the wound and the wound area is reduced by contraction.
Stages of Healing
-
- Haemostasis (1 hour): platelet plug formation, fibrin clot formation
-
- Inflammation (48 hours): macrophage infiltration, debridement
-
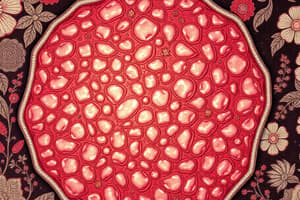
- Granulation tissue formation (2-5 days): endothelial cell and fibroblast proliferation, new blood vessels migrate from wound edges, collagen extra-cellular matrix
-
- Maturation of connective tissue (5+ days): decreased cellularity, decreased vascularity, remodelling of collagen matrix, collagen cross-linking
-
- Re-epithelialisation (1-3 days): proliferation of basal epithelial cells, migration of basal epithelial cells across wound bed, epithelial cells differentiate and stratified squamous structures reform
Haemostasis
- Consists of: platelet plug formation, fibrin clot formation
- Inhibited by: aspirin, warfarin, factor VIII deficiency
Inflammation
- Caused by: macrophage infiltration
Granulation Tissue
- Forms through: endothelial cell and fibroblast proliferation, new blood vessels migrate into damaged area, fibroblasts lay down collagen extra-cellular matrix
- Consists of: fibroblasts, blood vessels, inflammatory cells
Maturation of Connective Tissue
- Results in: decreased cellularity, decreased vascularity, remodelling of collagen matrix, collagen cross-linking
Re-epithelialisation
- Occurs through: proliferation of basal epithelial cells, migration of basal epithelial cells across wound bed, epithelial cells differentiate and stratified squamous structures reform
Factors Affecting Wound Healing
- 3 systemic factors: ageing, nutritional status, iatrogenic, pre-existing medical conditions
- 7 local factors: blood supply, infection, persistent irritation, poor wound stability, poor apposition of wound edges, direction of incision, ionising radiation
- 3 factors important in controlling wound healing: cell-cell interactions, cell-matrix interactions, autocrine/paracrine interactions
Macrophages
- 3 traditional functions: phagocytosis, protease synthesis, regulation of immune cell function
- 4 additional functions: fibroblast recruitment, extra-cellular matrix synthesis, platelet recruitment, growth of blood vessels
Complications of Wound Healing
- 5 complications: wound dehiscence, contractures, keloid/hypertrophic scar formation, weak scars, pigmentation
Keloids and Hypertrophic Scarring
- Keloid: sharply elevated, progressively enlarging scar characterised by excessive collagen formation in the dermis
- 2 differences between keloids and hypertrophic scarring: keloids may spread beyond the margins of the original wound, hypertrophic scars do not; keloids are mainly found in Afro-Caribbean populations, hypertrophic scarring affects varied population groups
- 1 similarity: seen on the face but does not affect the oral mucosa
Embryonic and Oral Mucosal Wound Healing
- Embryonic wound healing: peculiar due to absence of scarring, possibly due to immaturity of immune system
- Oral mucosal wound healing: peculiar due to less scarring than skin, no keloids/hypertrophic scarring, immune response seems different
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.