Podcast
Questions and Answers
What is one of the main roles of an audiologist in vestibular assessment?
What is one of the main roles of an audiologist in vestibular assessment?
- Conducting purely auditory tests without considering balance
- Focusing solely on hearing rehabilitation
- Screening, assessment, diagnosis, and management of balance system disorders (correct)
- Managing balance system disorders in isolation
Which vestibular assessment tool involves analyzing the response of the vestibular system to caloric stimulation?
Which vestibular assessment tool involves analyzing the response of the vestibular system to caloric stimulation?
- Pure Tone Audiometry (PTA)
- Vestibular Evoked Myogenic Potentials (VEMP)
- Video Nystagmography (VNG)
- Caloric test (correct)
What is the resting potential rate of vestibular hair cells?
What is the resting potential rate of vestibular hair cells?
- 50-60 spikes/sec
- 100-120 spikes/sec
- 70-100 spikes/sec (correct)
- 30-50 spikes/sec
Which assessment tool directly evaluates the granular movements of the head?
Which assessment tool directly evaluates the granular movements of the head?
What characteristic is true about vestibular organs in the context of their function?
What characteristic is true about vestibular organs in the context of their function?
What is the purpose of vestibular compensation?
What is the purpose of vestibular compensation?
Which of the following is a critical factor for effective VOR adaptation?
Which of the following is a critical factor for effective VOR adaptation?
What differentiates one vestibular pathology from another?
What differentiates one vestibular pathology from another?
In cases of bilateral vestibular loss, what is a key characteristic observed?
In cases of bilateral vestibular loss, what is a key characteristic observed?
How can a good history-taking contribute to vestibular disorder management?
How can a good history-taking contribute to vestibular disorder management?
When describing dizziness, which of the following is likely to indicate a vestibular origin?
When describing dizziness, which of the following is likely to indicate a vestibular origin?
What aspect of vestibular disorders is often assessed by analyzing the time course of symptoms?
What aspect of vestibular disorders is often assessed by analyzing the time course of symptoms?
Which associated symptom could suggest a vestibular pathology?
Which associated symptom could suggest a vestibular pathology?
Which of the following pathologies is characterized by an association with sudden onset vertigo without hearing loss?
Which of the following pathologies is characterized by an association with sudden onset vertigo without hearing loss?
What is a common trigger specifically associated with BPPV?
What is a common trigger specifically associated with BPPV?
Which symptom is not associated with Menière's disease?
Which symptom is not associated with Menière's disease?
What is a possible cause of BPPV?
What is a possible cause of BPPV?
In which scenario is balance likely to be worsened for individuals with vestibular dysfunction?
In which scenario is balance likely to be worsened for individuals with vestibular dysfunction?
Which of the following is not a common associated symptom of labyrinthitis?
Which of the following is not a common associated symptom of labyrinthitis?
What type of episodic occurrence is Menière's disease known to involve?
What type of episodic occurrence is Menière's disease known to involve?
Which of these is a potential trigger for migraines that may relate to vestibular disorders?
Which of these is a potential trigger for migraines that may relate to vestibular disorders?
Which symptom is commonly associated with Meniere's disease?
Which symptom is commonly associated with Meniere's disease?
What is the primary goal of acute treatment for vestibular neuritis?
What is the primary goal of acute treatment for vestibular neuritis?
Which of the following lifestyle changes is recommended to manage Meniere's disease?
Which of the following lifestyle changes is recommended to manage Meniere's disease?
How does benign paroxysmal positional vertigo (BPPV) typically present?
How does benign paroxysmal positional vertigo (BPPV) typically present?
What is a cause of Meniere's disease identified in the content?
What is a cause of Meniere's disease identified in the content?
Flashcards are hidden until you start studying
Study Notes
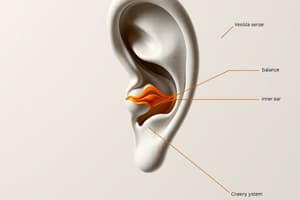
Vestibular System Assessment and Rehabilitation
- Audiologists play a critical role in vestibular assessment and rehabilitation.
- Audiologists are part of an interdisciplinary team and their role focuses on:
- Screening
- Assessment
- Diagnosis
- Management of individuals with balance system disorders.
- Audiologists perform a variety of tests to evaluate vestibular function:
- Pure tone audiometry (PTA): Measures hearing sensitivity.
- Acoustic Brainstem Response (ABR): Evaluates the function of the auditory nerve and brainstem.
- Electrocochleography (ECochG): Measures the electrical activity of the cochlea.
- Video Nystagmography (VNG): Records eye movements to assess vestibular function.
- Caloric test: Evaluates the function of the semicircular canals.
- Vestibular Evoked Myogenic Potentials (VEMP): Tests the function of the saccule and utricle.
- Video Head Impulse Test: Assesses the vestibulo-ocular reflex (VOR).
- Key learning issues in vestibular physiology:
- Vestibular hair cells have a high tonic firing rate (70-100 spikes/sec).
- Vestibular organs work in pairs.
- The VOR and vestibular spinal reflex (VSR) are closely related.
- Vestibular compensation mechanisms:
- Adaptation: The brain adapts to changes in sensory input.
- Habituation: The brain learns to ignore repetitive stimuli.
- Substitution: The brain uses other sensory systems to compensate for lost vestibular function.
- Critical periods in VOR adaptation:
- Recovery from unilateral vestibular lesions is faster with increased sensory input.
- Patients should be encouraged to move around in well-lit areas to engage their VOR and VSR.
- Bilateral vestibular loss:
- Individuals with bilateral vestibular loss cannot recalibrate their VOR.
- They often rely on other sensory systems (proprioception and vision) for balance.
- Differentiating vestibular disorders:
- Dizziness is a nonspecific term.
- Important to gather detailed information from patients:
- Time course of dizziness
- Associated symptoms
- Triggers
- A good history can help determine:
- Potential pathologies
- Potential problems during testing
- Necessary tests
- Management recommendations
- Description of dizziness:
- Vertigo: A sense of spinning or rotation, likely of vestibular origin.
- Lightheadedness: A feeling of faintness, potentially related to anxiety or cardiac issues.
- Disequilibrium: A feeling of imbalance, potentially due to proprioceptive loss or vestibular problems.
- Time course of dizziness:
- Different vestibular pathologies have different time courses.
- For example, Meniere’s attacks do not last for seconds, while BPPV does not last for hours.
- Associated symptoms:
- Different pathologies have different associated symptoms.
- BPPV is not associated with fluctuating hearing loss, Meniere’s does not involve facial palsy, and SCD does not involve migraines.
- Triggers for dizziness:
- Triggers can be pathology specific.
- BPPV can be triggered by head position changes, SCD by loud noise or pressure, and migraines by smell, light, food, or hormonal changes.
- Co-morbidities:
- Stress and anxiety are highly associated with vestibular disorders.
- Quick head movement usually indicates a vestibular origin.
- Causes of dizziness:
- Trauma, head colds, and viral infections can all cause vestibular disorders.
- Impact of visual cues:
- Balance is often poorer in the dark due to the lack of visual cues.
- Common vestibular disorders:
- Labyrinthitis: Inflammation of the inner ear, causing sudden onset vertigo, hearing loss, and tinnitus.
- Vestibular neuronitis: Inflammation of the vestibular nerve, causing sudden onset vertigo without hearing loss.
- Meniere’s disease: A condition that causes vertigo, hearing loss, and tinnitus.
- Benign Paroxysmal Positional Vertigo (BPPV): A condition caused by displaced otoconia in the inner ear, leading to brief spells of vertigo with head movements.
- Labyrinthitis:
- Cause: Viral infections (e.g., herpes zoster oticus, influenzal otitis).
- Symptoms: Sudden onset vertigo, hearing loss, tinnitus.
- Recovery: Typically in three stages:
- An acute period with severe vertigo and vomiting lasting 1-2 days.
- A sub-acute period with less severe symptoms lasting 2 weeks.
- A chronic compensation period lasting months or years.
- Vestibular Neuronitis:
- Cause: Viral infection, often part of the herpes family.
- Symptoms: Sudden onset vertigo, nausea, vomiting, tinnitus.
- Recovery: Usually within a few days, but recurrent episodes are possible.
- Treatment of labyrinthitis and vestibular neuritis:
- Symptomatic treatment with anti-emetics for nausea and vestibular suppressants to reduce dizziness.
- The use of vestibular retraining therapy.
- Meniere’s disease:
- Characterized by paroxysmal attacks of vertigo.
- Often associated with hearing loss and tinnitus.
- Attacks last for a few hours and occur in clusters.
- Diagnosis of Meniere’s disease:
- Definite Meniere’s disease: Two or more episodes of vertigo lasting 20 minutes to 12 hours, documented low-medium frequency sensorineural hearing loss (SNHL), and fluctuating aural symptoms (hearing, tinnitus, fullness) in the affected ear.
- Probable Meniere’s disease: Two or more episodes of vertigo lasting 20 minutes to 12 hours, fluctuating aural symptoms in the affected ear, and no better explanation by another diagnosis.
- Cause of Meniere’s disease:
- Endolymphatic hydrops: Build-up of fluid in the inner ear.
- Treatment of Meniere’s disease:
- Avoiding overtiredness, stress, coffee, tea, red wine, and cheese.
- Benign Paroxysmal Positional Vertigo (BPPV):
- Described as a benign, paroxysmal, positional vertigo.
- Occurs with a change in head position.
- Characterized by sudden, brief spells of vertigo.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.