Podcast
Questions and Answers
What positioning of the patient affects the size of the internal jugular vein (IJV)?
What positioning of the patient affects the size of the internal jugular vein (IJV)?
- Lying on the side
- Seated with legs elevated
- Sitting or standing (correct)
- Lying flat on the back
Which technique is used to evaluate the internal jugular vein?
Which technique is used to evaluate the internal jugular vein?
- Electric impedance scanning
- Transducer compression and spectral Doppler waveforms (correct)
- Manual palpation of the vein
- Only grayscale imaging
What is the primary function of the median cubital vein?
What is the primary function of the median cubital vein?
- To connect the basilic and cephalic veins (correct)
- To join the radial trunk
- To serve as a major conduit for blood flow to the hand
- To drain the forearm muscles
Why is the external jugular vein (EJV) often not included in standard examinations?
Why is the external jugular vein (EJV) often not included in standard examinations?
What documentation techniques cannot be performed for brachiocephalic veins?
What documentation techniques cannot be performed for brachiocephalic veins?
Which vein is the longest and typically serves as a landmark for anatomical differentiation?
Which vein is the longest and typically serves as a landmark for anatomical differentiation?
Where does the basilic vein originate?
Where does the basilic vein originate?
The internal jugular vein (IJV) serves as which type of pathway?
The internal jugular vein (IJV) serves as which type of pathway?
Which statement about the cephalic and basilic veins is correct?
Which statement about the cephalic and basilic veins is correct?
What is a key reason for evaluating the veins in the neck?
What is a key reason for evaluating the veins in the neck?
Where is the external jugular vein primarily documented?
Where is the external jugular vein primarily documented?
Which aspect of the forearm does the radial veins travel along?
Which aspect of the forearm does the radial veins travel along?
What anatomical region does the median cubital vein cross?
What anatomical region does the median cubital vein cross?
What anatomical feature serves as a landmark for identifying the internal jugular vein (IJV)?
What anatomical feature serves as a landmark for identifying the internal jugular vein (IJV)?
Which of the following describes the course of the basilic vein?
Which of the following describes the course of the basilic vein?
What is true about the communication between major arm veins?
What is true about the communication between major arm veins?
Which component is NOT typically associated with the normal image characteristics of the upper extremity venous system?
Which component is NOT typically associated with the normal image characteristics of the upper extremity venous system?
Which risk factor is LESS associated with venous thrombosis in the upper extremity?
Which risk factor is LESS associated with venous thrombosis in the upper extremity?
What distinguishes the upper extremity thrombus formation from that in the lower extremity?
What distinguishes the upper extremity thrombus formation from that in the lower extremity?
Paget–Schroetter syndrome is primarily associated with which condition?
Paget–Schroetter syndrome is primarily associated with which condition?
What Doppler characteristic is likely to be observed in a patient with upper extremity thrombosis?
What Doppler characteristic is likely to be observed in a patient with upper extremity thrombosis?
Which of the following symptoms is NOT commonly associated with upper extremity thrombosis?
Which of the following symptoms is NOT commonly associated with upper extremity thrombosis?
Which procedure is most likely to increase the risk of upper extremity thrombosis?
Which procedure is most likely to increase the risk of upper extremity thrombosis?
Which of the following is NOT part of Virchow's triad for thrombus formation?
Which of the following is NOT part of Virchow's triad for thrombus formation?
In which scenario would an upper extremity venous examination be indicated?
In which scenario would an upper extremity venous examination be indicated?
Upper extremity thrombus aging can be identified by which characteristic?
Upper extremity thrombus aging can be identified by which characteristic?
What characteristic should spectral Doppler exhibit?
What characteristic should spectral Doppler exhibit?
Where does the cephalic vein typically drain into?
Where does the cephalic vein typically drain into?
Which of the following techniques can help visualize the subclavian vein more effectively?
Which of the following techniques can help visualize the subclavian vein more effectively?
What is the main challenge in compressing the subclavian vein during imaging?
What is the main challenge in compressing the subclavian vein during imaging?
In which anatomical location does the cephalic vein commonly communicate with the median cubital vein?
In which anatomical location does the cephalic vein commonly communicate with the median cubital vein?
What imaging technique should be used to visualize the cephalic vein?
What imaging technique should be used to visualize the cephalic vein?
Which statement about the cephalic vein is correct?
Which statement about the cephalic vein is correct?
What aspect does the visualization of the brachiocephalic veins require?
What aspect does the visualization of the brachiocephalic veins require?
What is expected to be observed in the case of complete thrombus during a Doppler ultrasound?
What is expected to be observed in the case of complete thrombus during a Doppler ultrasound?
What characteristic appearance do indwelling venous catheters have on ultrasound?
What characteristic appearance do indwelling venous catheters have on ultrasound?
What is the appearance of acute thrombus in a vein?
What is the appearance of acute thrombus in a vein?
Which of the following may result from thrombosis around a venous catheter?
Which of the following may result from thrombosis around a venous catheter?
What should be done if a catheter becomes thrombosed?
What should be done if a catheter becomes thrombosed?
How does chronic post-thrombotic changes appear in veins?
How does chronic post-thrombotic changes appear in veins?
What is a key characteristic for diagnosing vein thrombosis?
What is a key characteristic for diagnosing vein thrombosis?
What is a common method for treating upper extremity thrombus?
What is a common method for treating upper extremity thrombus?
What appearance may be observed around a vein associated with inflammation?
What appearance may be observed around a vein associated with inflammation?
What is the expected Doppler signal in the case of partial thrombus?
What is the expected Doppler signal in the case of partial thrombus?
What is indicated by respiratory phasicity in spectral Doppler waveforms?
What is indicated by respiratory phasicity in spectral Doppler waveforms?
Which condition may lead to the presence of arterialized venous flow?
Which condition may lead to the presence of arterialized venous flow?
Which feature is characteristic of normal venous flow in Doppler studies?
Which feature is characteristic of normal venous flow in Doppler studies?
What does a residual fibrous sheath appear to resemble after catheter removal?
What does a residual fibrous sheath appear to resemble after catheter removal?
What happens to vein diameter during respiration?
What happens to vein diameter during respiration?
What indicates that a vein cannot be fully compressed?
What indicates that a vein cannot be fully compressed?
Flashcards
Cephalic Vein
Cephalic Vein
Superficial vein in the arm, longest in the arm, originates from the dorsal venous arch on the medial side of the hand, runs along the lateral side of the forearm and biceps muscle, and empties into the axillary vein.
Basilic Vein
Basilic Vein
Superficial vein in the arm, originates from the dorsal venous arch on the ulnar side of the hand, runs along the medial side of the forearm and biceps muscle, and joins the brachial vein to form the axillary vein.
Median Cubital Vein
Median Cubital Vein
Superficial vein that crosses the antecubital fossa, connecting the basilic and cephalic veins.
Ulnar Trunk
Ulnar Trunk
Signup and view all the flashcards
Radial Trunk
Radial Trunk
Signup and view all the flashcards
Upper Extremity Venous System
Upper Extremity Venous System
Signup and view all the flashcards
Upper Extremity Thrombosis
Upper Extremity Thrombosis
Signup and view all the flashcards
Paget-Schroetter Syndrome
Paget-Schroetter Syndrome
Signup and view all the flashcards
Virchow's Triad
Virchow's Triad
Signup and view all the flashcards
Venous Stasis
Venous Stasis
Signup and view all the flashcards
Hypercoagulability
Hypercoagulability
Signup and view all the flashcards
Vessel Wall Injury
Vessel Wall Injury
Signup and view all the flashcards
Subclavian Vein
Subclavian Vein
Signup and view all the flashcards
Catheter-Related Thrombosis
Catheter-Related Thrombosis
Signup and view all the flashcards
PICC Line
PICC Line
Signup and view all the flashcards
Internal Jugular Vein (IJV)
Internal Jugular Vein (IJV)
Signup and view all the flashcards
IJV Evaluation
IJV Evaluation
Signup and view all the flashcards
Valsalva Maneuver
Valsalva Maneuver
Signup and view all the flashcards
External Jugular Vein (EJV)
External Jugular Vein (EJV)
Signup and view all the flashcards
EJV Imaging
EJV Imaging
Signup and view all the flashcards
Brachiocephalic Veins
Brachiocephalic Veins
Signup and view all the flashcards
Transducer Compression
Transducer Compression
Signup and view all the flashcards
Spectral Doppler
Spectral Doppler
Signup and view all the flashcards
Brachiocephalic Vein
Brachiocephalic Vein
Signup and view all the flashcards
Subclavian Vein
Subclavian Vein
Signup and view all the flashcards
Cephalic Vein
Cephalic Vein
Signup and view all the flashcards
Transverse Compression
Transverse Compression
Signup and view all the flashcards
Color Doppler
Color Doppler
Signup and view all the flashcards
Pulsatility
Pulsatility
Signup and view all the flashcards
Phasicity
Phasicity
Signup and view all the flashcards
Scanning Technique
Scanning Technique
Signup and view all the flashcards
Normal Vein Walls
Normal Vein Walls
Signup and view all the flashcards
Vein Diameter Change
Vein Diameter Change
Signup and view all the flashcards
Thrombus Suspicion
Thrombus Suspicion
Signup and view all the flashcards
Echogenic Material
Echogenic Material
Signup and view all the flashcards
Acute Thrombus
Acute Thrombus
Signup and view all the flashcards
Chronic Post-Thrombotic Changes
Chronic Post-Thrombotic Changes
Signup and view all the flashcards
Color Doppler
Color Doppler
Signup and view all the flashcards
Spectral Doppler
Spectral Doppler
Signup and view all the flashcards
Abnormal Doppler Signals
Abnormal Doppler Signals
Signup and view all the flashcards
Partial Thrombus
Partial Thrombus
Signup and view all the flashcards
Retrograde Venous Flow
Retrograde Venous Flow
Signup and view all the flashcards
Arterialized Venous Flow
Arterialized Venous Flow
Signup and view all the flashcards
Indwelling Venous Catheter
Indwelling Venous Catheter
Signup and view all the flashcards
Catheter-Related Thrombosis
Catheter-Related Thrombosis
Signup and view all the flashcards
Reduced Doppler Signals (Catheter)
Reduced Doppler Signals (Catheter)
Signup and view all the flashcards
Thrombus Removal (Catheter)
Thrombus Removal (Catheter)
Signup and view all the flashcards
Treatment Options (Thrombus)
Treatment Options (Thrombus)
Signup and view all the flashcards
Study Notes
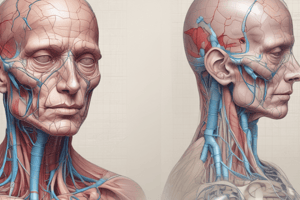
Vascular Anatomy
- Upper extremity veins originate distally and drain towards the heart.
- Vessel anatomy is described from the wrist to the chest.
- Vessel location (proximal, middle, distal) is identified from its proximity to the heart.
- Deep veins have an accompanying artery.
- Forearm and brachial veins are typically duplicated (axillary veins may also be duplicated).
Upper Extremity Veins - Memory Tricks
- Brachial veins are paired, deep veins resembling Mickey Mouse.
- Basilic vein is a singular superficial vein, resembling a snake (Basilisk).
- Radial veins are paired, deep veins on the thumb side of the forearm, like a radius.
- Ulnar veins are paired deep veins on the pinky side of the forearm.
Forearm Veins - Radial and Ulnar
- Radial and ulnar veins are paired, deep veins.
- Ulnar veins originate from the palmar venous arch in the hand and travel along the medial aspect of the forearm, joining near the elbow to form the ulnar trunk.
- Radial veins originate from the dorsal metacarpal veins and travel up the lateral aspect of the forearm, joining near the elbow to form the radial trunk.
Entire Arm Vein - Cephalic Vein
- Cephalic vein is a superficial vein, the longest in the arm.
- Originates from the medial component of the dorsal venous arch.
- Winds around the radial border of the forearm and continues along the lateral border of the biceps muscle.
- Empties into the axillary vein.
- Used as a landmark to distinguish the subclavian vein from the axillary vein.
Entire Arm Vein - Basilic Vein
- Basilic vein is a superficial vein.
- Originates from the ulnar component of the dorsal venous arch.
- Courses along the ulnar aspect of the forearm.
- Continues along the medial border of the biceps muscle.
- Joins the brachial vein to form the axillary vein.
- Both cephalic and basilic veins communicate with the median cubital vein.
Median Cubital Vein
- Superficial vein that crosses the antecubital fossa obliquely.
- Connects the basilic and cephalic veins.
- Common site for venipuncture, making it prone to thrombus formation.
- Several possible anatomical variations exist.
Upper Arm Vein Diagram
- Shows the arrangement of upper extremity veins crossing the axillary region.
- Includes subclavian, cephalic, axillary, and basilic veins, along with venae comitantes of the brachial artery.
Upper Arm Veins - Brachial Veins
- Brachial veins are deep veins, usually paired.
- They follow the course of the brachial artery.
- They usually join near the axilla to form the axillary vein.
Upper Arm Vein - Axillary Vein
- Usually a single vein.
- Starts at the junction of brachial and basilic veins.
- Runs along the shoulder until it joins the cephalic vein to become the subclavian vein, typically near the upper border of the first rib.
Chest Area Vein - Subclavian Vein
- Continuation of the axillary vein.
- Located just past the outer border of the first rib.
- Joins the internal jugular vein to form the brachiocephalic (innominate) vein at the clavicular level.
Neck Veins - Internal and External Jugular Veins
- Internal jugular vein (IJV): Runs adjacent to the common carotid artery, receives blood from the face and neck, and joins the subclavian vein to form the brachiocephalic vein.
- External jugular vein (EJV): Drains blood from the cranium, face, and neck, and empties into the subclavian vein.
Chest Area Veins - Brachiocephalic / Innominate Veins
- Formed at the junction of the internal jugular and subclavian veins at the clavicular level.
- There is one at each side of the neck.
Chest Area Vein - Superior Vena Cava (SVC)
- Formed by the junction of the right and left brachiocephalic veins.
- Courses behind the right side of the sternum.
- Enters the heart at the right atrium.
Duplex Ultrasound Imaging of the Upper Extremity Venous System
- Objectives include describing components and characteristics of the upper extremity venous system, identifying thrombus characteristics, describing Doppler waveforms, listing risk factors associated with venous thrombosis.
Background
- Protocol techniques for upper extremity veins are similar to those for lower extremity.
- Three differences: 1) Thrombi in lower extremities are often caused by stasis; upper extremity thrombi are not related to stasis. 2) Superficial veins are more often affected in the arms than legs. 3) Venous anatomy of the upper extremity is more variable than the lower extremity.
Pathophysiology
- Virchow's triad: venous stasis, hypercoagulability, and vessel wall injury.
- Upper extremity thrombosis is more often caused by injury to the vessel walls.
- Catheter or needle insertion into arm veins is another frequent cause of upper extremity thrombosis.
Paget-Schroetter Syndrome
- Venous thrombosis connected to compression of the subclavian vein at the thoracic outlet.
- Also referred to as venous thoracic outlet syndrome (VTOS) or effort thrombosis.
- Typically occurs in young, athletic, muscular males, but can be found in other individuals.
Catheters as Causes of Upper Extremity Thrombosis
- Subclavian and internal jugular veins are frequently accessed for indwelling catheters and pacemaker wire introduction.
- Peripherally inserted central catheters (PICCs) can also cause thrombosis.
Signs & Symptoms
- Similar to those in lower extremity.
- May include unilateral arm or hand swelling, superficial palpable cord, erythema, pain, tenderness, facial swelling, dilated chest wall collaterals.
Other Indications for an UEV Examination
- Asymptomatic patients may be examined prior to central catheter placement or pacemaker placement.
- Duplex may be used to confirm the abovementioned devices.
- Upper extremity veins may be evaluated in patients suspected of pulmonary embolism.
- PE symptoms include chest pain, tachypnea, or tachycardia.
Sonographic Examination Techniques
- Similar techniques are used for upper extremity as for lower extremity.
- Transducer compression is performed over all possible vein areas.
- Gentle transducer compression directs the compression over veins allowing walls to come together.
- The compression is repeated every 2-3 cm along the vein.
- Spectral Doppler waveforms are recorded from all major veins.
Patient Preparation
- Explain the examination procedure to the patient.
- Obtain relevant history, including questioning about signs and symptoms.
- Remove upper extremity clothes and jewelry; provide a gown or drape.
Patient Positioning
- There is no need to tilt the bed for examination.
- Internal jugular and subclavian veins are examined with the patient lying flat.
- For the jugular and subclavian veins, patients’ arm can be positioned at their side.
- The arm is abducted for evaluation of the remaining veins.
Equipment
- Two transducers are recommended.
- Midrange (5-10 MHz) linear array for internal jugular, brachiocephalic, subclavian, axillary, deep, and brachial veins.
- Higher frequency (10-18 MHz) linear array for superficial veins (cephalic and basilic) and small forearm veins (radial and ulnar).
- Curved or sector arrays are beneficial for deeper vessels near the clavicle and sternum.
Scanning Technique - Internal Jugular Veins
- Veins in the neck should be evaluated because thrombi from the arm can extend up; they are an important collateral pathway.
- The common carotid artery may be used as a landmark.
- The IJV will collapse if the patient is sitting or standing; Valsalva will increase IJV size.
- Evaluation should include transverse views with transducer compression in addition to spectral Doppler waveforms.
IJV Transverse Images
- Figure 18-1. A transverse view with color of the internal jugular vein (IJV) and the common carotid artery (CCA).
- Figure 18-2. Grayscale transverse image showing the location of the internal jugular vein (IJV) beside the common carotid artery (CCA).
IJV Spectral Doppler Image
- Figure 18-3: Spectral Doppler waveform from the internal jugular vein.
Scanning Technique - External Jugular Veins
- Lighten transducer pressure and slide the probe posteriorly from the internal jugular vein.
- Should run without an accompanying artery, close to the skin surface.
- The external jugular vein usually terminates into the subclavian vein.
- Transverse views with transducer compression and spectral Doppler should be used.
Scanning Technique - Brachiocephalic Veins
- Challenging because positioned behind bony landmarks.
- Most often evaluated at the confluence of the internal jugular and subclavian veins.
- Compressions cannot be performed.
- Documentation depends on grayscale, color-flow imaging, and spectral Doppler waveforms.
- Spectral Doppler should demonstrate phasicity and pulsatility.
Brachiocephalic Veins Color Doppler
- Figure 18-4: A color image of the brachiocephalic vein, demonstrating internal jugular veins, subclavian veins.
Brachiocephalic Veins Spectral Doppler
- Figure 18-5: Spectral Doppler waveform from the brachiocephalic vein.
Scanning Technique - Subclavian Vein
- Visualized above and below the clavicle.
- Accompanied by the subclavian artery.
- Cephalic vein terminates into the subclavian vein past the clavicle.
- Can be challenging to compress.
- The patient can perform a sniff or quick, deep breath using pursed lips to collapse the subclavian vein.
- Color and spectral Doppler should be documented.
Transverse Subclavian Vein
- Figure 18-6: Shows a transverse view of the subclavian artery (SCA) and subclavian vein (SCV).
Cephalic Vein Draining Into Subclavian Vein
- Figure 18-7 A: Grayscale image of the cephalic vein terminating into the subclavian vein (SCV).
- Figure 18-7 B: Color-flow imaging at the cephalic vein termination.
Scanning Technique - Cephalic Vein
- Travels superficially along the skin, near the anterolateral border of the biceps muscle.
- Communicates with the median cubital vein in the antecubital fossa.
- Usually travels as two vessels, one on the volar and one on the dorsal aspect of the forearm.
- Document in transverse with transducer compressions and color/spectral Doppler.
Transverse Compression of Cephalic Vein
- Figure 18-8: A transverse image showing the cephalic vein in the upper arm and compressed.
Sagittal Color image of Cephalic Vein
- Figure 18-9: A longitudinal view of the cephalic vein with added color.
Median Cubital Vein
- Connects the cephalic and basilic veins.
- Located in the antecubital fossa with variable connection patterns.
- Common venipuncture site, therefore prone to thrombus formation.
- Compressed and noncompressed images should be documented.
Transverse Median Cubital Vein
- Figure 18-10: Transverse view of the median cubital vein (MCV) as it passes over the brachial artery and brachial vein.
Scanning Technique - Axillary Vein
- Terminates at the junction of the cephalic and subclavian veins.
- Deep vein accompanied by the axillary artery.
- Courses deeply from shoulder to axilla.
- Basilic vein terminates into axillary vein near the distal axilla.
- Compressed and noncompressed images should be documented with color and spectral Doppler information.
Transverse Color Image of the Axillary Vein
- Figure 18-11: A transverse view of the axillary artery (A) and vein (V) with color over the shoulder.
Transverse Color Axillary Vein from Within the Axilla
- Figure 18-12: A transverse view of the axillary artery (red) and vein (blue) within the axilla, showing separation between the two vessels.
Scanning Technique - Brachial Veins
- Terminates when the basilic vein enters to become the axillary vein.
- Usually small, paired, deep veins with an accompanying brachial artery.
- Formed at the junction of the two radial and two ulnar arteries near the antecubital fossa.
- Document with compressed and noncompressed images.
- Color and spectral Doppler can be included.
Transverse Color Brachial and Basilic Veins
- Figure 18-13: Transverse view of the brachial artery (A) and veins (V) in the upper arm and basilic vein.
Scanning Technique - Radial Veins
- Courses along the volar aspect of the forearm.
- Paired deep veins that course alongside the radial artery.
- Very small, rarely involved in venous thrombosis.
- Often not included in routine upper extremity venous examinations.
Transverse Color Radial Veins
- Figure 18-14: A transverse view of the radial artery (A) and veins (V) showing the cephalic vein.
Scanning Technique - Ulnar Veins
- Travels along the volar aspect of the forearm.
- Deep, paired veins that travel with the accompanying ulnar artery.
- Often very small and not examined unless indicated by presenting symptoms.
Transverse Ulnar Veins
- Figure 18-15: A transverse view of the ulnar artery (A) and veins (V), including the basilic vein.
Scanning Technique - Basilic Vein
- Terminates into the axillary vein in the upper arm.
- Courses medially and superficially without a companion artery.
- Usually the largest vein in the upper arm region.
- Communicates with the cephalic vein via the median cubital vein in the antecubital fossa.
- Typically has two branches in the forearm (one volar, one dorsal).
- Document with compressed and noncompressed images.
- Color and spectral Doppler can be used.
Transverse Basilic Vein
- Figure 18-16: A transverse view of the basilic vein in the upper arm, along with the brachial artery and veins.
Pitfalls
- Compression is not possible in several upper extremity locations.
- Color and spectral Doppler are crucial during examinations in these areas.
- Dressings and catheters may limit access to veins.
- Adjacent nerve bundles can be mistaken for a thrombosed vein.
Diagnosis
- Diagnostic criteria are the same for upper extremity as for lower extremity veins.
- Normal vein walls compress completely under transducer pressure.
- Transversal plane compressions are performed.
- Vein walls must be smooth and thin with an anechoic vessel lumen.
- Vein diameter can change slightly with respiration.
Diagnosing Thrombus
- If vein walls do not compress, a thrombus is suspected.
- Echogenic material within the vein lumen is observed.
- Acute thrombus: poorly attached to the vessel wall, spongy, dilated, varying echogencity, and smooth surface.
- Chronic post-thrombotic changes: brightly echogenic thrombus, well attached, rigid, irregular surfaced, and contracted vein.
- Superficial vein thrombus appears similar to deep vein thrombus.
- Hypoechoic areas may surround the vein due to inflammation.
Transverse IJV with Compression
- Figure 18-17: Transverse view of a patent internal jugular vein (IJV), non-compressed and compressed.
Transverse & Sagittal IJV with Thrombus
- Figure 18-18: A: Transverse, B: Longitudinal views showing an acute thrombus in the IJV.
Axillary Vein Chronic Post-Thrombotic Changes
- Figure 18-19: A & B: Non-compressed and compressed views showing chronic post-thrombotic changes in the axillary vein.
Color and Spectral Doppler
- Important diagnostic tools for upper extremity veins that cannot be compressed.
- Color should be visible throughout the vessel lumen.
- Spectral Doppler should show respiratory phasicity and augmentation with distal compression.
- Pulsatility is common due to proximity to the heart.
Subclavian Vein Spectral Doppler
- Figure 18-21: Doppler spectral waveform from the subclavian vein, showing normal pulsatile flow.
Abnormal Color and Spectral Doppler
- In complete thrombi, no spectral Doppler signals or color filling are present.
- Partial thrombi can exhibit continuous flow.
- Retrograde flow in the jugular veins is uncommon, but can occur if they serve as collateral pathways.
- Arterialized venous flow may present in patients with hemodialysis fistulas or grafts.
Venous Catheters
- Indwelling venous catheters are common in the arm.
- Catheters appear as bright, straight, parallel echoes within the vessel lumen.
- Thrombus can develop around the catheter, presenting as echogenic material around the catheter surface.
- Spectral Doppler signals are diminished or continuous.
- Thrombosed catheters should be removed.
Normal Venous Catheter on Ultrasound
- Figure 18-22: A longitudinal view of a catheter within a vein.
Thrombus forming on a Venous Catheter
- Figure 18-23: A longitudinal view of a thrombus forming on a venous catheter.
Residual Fibrous Sheath after Removing a Venous Catheter with Thrombus
- Figure 18-25: Shows a longitudinal view of remnant fibrous sheath left after removing a catheter; it resembles the original catheter.
Treatments For Upper Extremity Thrombus
- Treatment considerations include anticoagulation, catheter removal, thrombolytic therapy, surgical compression or venous reconstruction, and conservative treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.