Podcast
Questions and Answers
What is a nonvascular finding that may be observed in imaging?
What is a nonvascular finding that may be observed in imaging?
- Significant arterial disease
- Cysts and hematomas (correct)
- Aneurysms
- Pseudoaneurysms
What is a possible vascular finding that can occur related to venous issues?
What is a possible vascular finding that can occur related to venous issues?
- Edema (correct)
- Enlarged lymph nodes
- Tumors (Neoplasia)
- Abscesses/Infections
Which treatment option involves the use of medications for managing thrombus?
Which treatment option involves the use of medications for managing thrombus?
- Catheter removal
- Anticoagulation (correct)
- Thrombolytic therapy
- Surgical compression
What condition may require surgical compression of the thoracic inlet?
What condition may require surgical compression of the thoracic inlet?
In what context is ultrasound used during vascular intervention?
In what context is ultrasound used during vascular intervention?
What is the primary function of the cephalic vein in the upper extremity?
What is the primary function of the cephalic vein in the upper extremity?
Which veins unite to form the brachial veins near the antecubital fossa?
Which veins unite to form the brachial veins near the antecubital fossa?
Which of the following veins is typically the site for veni-puncture?
Which of the following veins is typically the site for veni-puncture?
Which vein is a continuation of the axillary vein in the upper extremity?
Which vein is a continuation of the axillary vein in the upper extremity?
Where does the subclavian vein originate in the upper extremity?
Where does the subclavian vein originate in the upper extremity?
What is a characteristic of the brachial veins in terms of their anatomical arrangement?
What is a characteristic of the brachial veins in terms of their anatomical arrangement?
What characterizes the relationship between the internal jugular vein and the subclavian vein?
What characterizes the relationship between the internal jugular vein and the subclavian vein?
Which superficial vein primarily drains the medial aspect of the upper arm?
Which superficial vein primarily drains the medial aspect of the upper arm?
What condition is associated with extrinsic compression of the brachial plexus and can lead to symptoms of pain or neurologic deficit?
What condition is associated with extrinsic compression of the brachial plexus and can lead to symptoms of pain or neurologic deficit?
Which of these syndromes is specifically referred to as 'effort thrombosis'?
Which of these syndromes is specifically referred to as 'effort thrombosis'?
Which statement accurately describes the typical demographic for Paget-Schroetter syndrome?
Which statement accurately describes the typical demographic for Paget-Schroetter syndrome?
What is the primary ultrasound technique used for evaluating upper extremity veins?
What is the primary ultrasound technique used for evaluating upper extremity veins?
What is a common symptom of Superior Vena Cava Syndrome?
What is a common symptom of Superior Vena Cava Syndrome?
What should be assessed during patient preparation for an upper extremity examination?
What should be assessed during patient preparation for an upper extremity examination?
During an evaluation of the internal jugular and subclavian veins, what position should the patient be in?
During an evaluation of the internal jugular and subclavian veins, what position should the patient be in?
How often should the compression maneuver be repeated along the vein during examination?
How often should the compression maneuver be repeated along the vein during examination?
What is the primary role of the median cubital vein in medical procedures?
What is the primary role of the median cubital vein in medical procedures?
Which of the following best describes the appearance of veins during a diagnostic ultrasound indicating thrombosis?
Which of the following best describes the appearance of veins during a diagnostic ultrasound indicating thrombosis?
What is a common pitfall in scanning the upper extremity veins that may affect the accuracy of the examination?
What is a common pitfall in scanning the upper extremity veins that may affect the accuracy of the examination?
How does respiration affect the diameter of veins during ultrasound examination?
How does respiration affect the diameter of veins during ultrasound examination?
What imaging artifact is commonly seen in the jugular vein, which may confuse diagnosis?
What imaging artifact is commonly seen in the jugular vein, which may confuse diagnosis?
In acute thrombus, which of the following characteristics is typically observed?
In acute thrombus, which of the following characteristics is typically observed?
What is the philosophical classification of findings when vein walls do not coapt during an ultrasound?
What is the philosophical classification of findings when vein walls do not coapt during an ultrasound?
Which statement is true regarding venous scanning techniques in the upper extremity?
Which statement is true regarding venous scanning techniques in the upper extremity?
What is a key feature of spectral Doppler waveforms that indicates normal venous function?
What is a key feature of spectral Doppler waveforms that indicates normal venous function?
Which of the following observations suggests the presence of a complete thrombus in a vein?
Which of the following observations suggests the presence of a complete thrombus in a vein?
What happens to blood flow distal to an occlusive thrombosis?
What happens to blood flow distal to an occlusive thrombosis?
What appearance does a thrombus develop around an indwelling venous catheter?
What appearance does a thrombus develop around an indwelling venous catheter?
What is a characteristic feature of arterialized venous flow?
What is a characteristic feature of arterialized venous flow?
What does abnormal flow patterns in central veins typically indicate?
What does abnormal flow patterns in central veins typically indicate?
In the context of upper extremity veins, what should color Doppler show for a normal vessel?
In the context of upper extremity veins, what should color Doppler show for a normal vessel?
Which condition might cause jugular veins to demonstrate reversed flow?
Which condition might cause jugular veins to demonstrate reversed flow?
Flashcards are hidden until you start studying
Study Notes
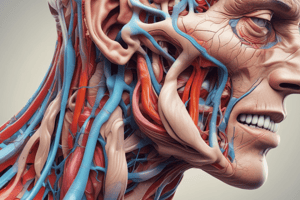
Upper Extremity Venous System
- The upper extremity venous system is comprised of superficial and deep veins.
Superficial Veins:
- Cephalic vein: Runs along the radial aspect of the forearm, uniting at the antecubital fossa, continues along the lateral border of the biceps muscle, empties into the axillary vein.
- Basilic vein: Runs along the ulnar aspect of the forearm, uniting at the antecubital fossa, continues along the medial upper arm, joins the brachial vein to form the axillary vein.
- Median cubital vein: Located in the antecubital fossa, connects the basilic and cephalic veins, a common site for venipuncture.
Deep Veins:
- Radial and Ulnar veins: Paired deep veins that accompany the radial and ulnar arteries, unite near the antecubital fossa to form the brachial veins.
- Brachial veins: Usually paired, follow the course of the brachial artery.
- Axillary vein: Usually single, begins at the junction of the brachial and basilic veins.
- Subclavian vein: Continuation of the axillary vein at the level of the terminal cephalic vein, begins just past the outer border of the first rib, receives drainage from the external jugular vein.
- Internal Jugular Vein: Located on either side of the neck lateral to the carotid artery, joins with the subclavian vein to form the brachiocephalic (innominate) vein.
- External Jugular Vein: Located more posteriorly than the IJV.
Indications for Duplex Ultrasound:
- Assessment of central catheter placement.
- Assessment prior to pacemaker placement.
- Evaluation of venous disorders.
Upper Extremity Venous Disorders:
- Thoracic Outlet Syndrome (TOS): Extrinsic compression of the brachial plexus, subclavian artery or vein in the thoracic outlet, leading to pain, neurologic deficit.
- Paget-Schroetter syndrome: A type of TOS associated with venous obstruction, also known as effort thrombosis, characterized by venous thrombosis associated with compression of the subclavian vein at the thoracic outlet, commonly seen in young, athletic, muscular males.
- Superior Vena Cava Syndrome: Occlusion or compression of the SVC, causing increased venous pressure, edema of the neck, face and arms, usually bilaterally.
Sonographic Examination Techniques:
- Similar technique as used for the lower extremity.
- Transducer compression is performed over all accessible upper extremity veins.
- Gentle compression is applied directly over the vein to coapt the vein walls.
- Compression maneuver is repeated every 2 to 3 cm along the course of each vein.
- Spectral Doppler waveforms are recorded from all major veins.
Patient Preparation:
- Explain the procedure to the patient.
- Obtain relevant history including signs and symptoms.
- Remove upper extremity clothing and jewelry, provide a gown or drape.
Patient Positioning:
- No need to tilt the bed for exam.
- Internal jugular and subclavian veins are examined with the patient lying flat.
- Arm can be positioned at the patient's side for jugular and subclavian vein evaluation.
- Abduct the arm to evaluate the remaining veins.
Scanning Technique:
- Median Cubital Vein:
- Connects cephalic and basilic veins.
- Resides in the antecubital fossa but the connection pattern varies.
- Common site for venipuncture and therefore thrombus.
- Compressed and non-compressed images are documented.
Pitfalls/Contraindications:
- Compression may not be possible in several locations.
- Color and spectral Doppler are relied upon in these areas.
- Dressings or intravenous catheters may limit access to veins.
- Color and spectral Doppler are important in cases with dressings or IV catheters.
- Normal upper extremity structures (muscles, tendons, nerves) may be visualized, avoid mistaking them for thrombosed vessels.
- Exam is contraindicated if the patient cannot be safely repositioned.
Diagnosis:
- Normal vein walls will completely compress with transducer pressure.
- Compressions are performed in the transverse plane.
- Vein walls should be smooth and thin with an anechoic vessel lumen.
- Vein diameter changes slightly with respiration.
Diagnosis - Thrombus:
- Suspect thrombus if vein walls do not coapt.
- Echogenic material within the vein lumen.
- Acute thrombus: Poorly attached to the vessel wall, thrombus is spongy, vein is dilated.
- Chronic thrombus: Brightly echogenic thrombus, well-attached, rigid, and contracted vein.
- Superficial vein thrombus appears the same as deep vein thrombosis.
- Hypoechoic areas may be present around the vein due to inflammation.
- Positive DVT/Thrombus findings are considered a medical emergency.
- Ensure the patient is safely returned to their designated room or report to the emergency room.
Diagnosis - Color and Spectral Doppler:
- Important diagnostic tools in upper extremity veins that cannot be compressed.
- Color filling should be seen in the entire vessel lumen.
- Spectral Doppler waveforms should demonstrate:
- Respiratory phasicity.
- Augmentation with distal compression.
- Pulsatility, common due to proximity to the heart.
Diagnosis - Color and Spectral Doppler - Cont:
- No spectral Doppler signals or color filling will be obtained with complete thrombus.
- Continuous flow will be seen distal to occlusive thrombosis or extrinsic compression.
- Retrograde flow is uncommon; however, jugular veins may demonstrate reversed flow if they are serving as a collateral pathway.
- Arterialized venous flow may be present in patients with hemodialysis fistula or graft.
Venous Catheters:
- Indwelling venous catheters are commonly encountered in the arm.
- Catheters appear as bright, straight, parallel echoes within the vessel lumen.
- Thrombus may develop around these catheters.
- Appears as echogenic material around the catheter surface.
- Spectral Doppler signals will be diminished and/or continuous.
- Catheter must be removed if it becomes thrombosed.
Incidental Findings and Differential Diagnosis:
- Nonvascular findings:
- Edema.
- Cysts and hematomas (may cause extrinsic compression).
- Enlarged lymph nodes.
- Tumors (neoplasia) (may cause extrinsic compression).
- Abscesses/infections (ex: cellulitis) (hyperemia may be noted).
- Vascular findings:
- Aneurysms.
- Pseudoaneurysms.
- Arteriovenous fistulas (arterialized venous flow).
- Significant arterial disease.
Treatment and Vascular Intervention with Ultrasound:
- Treatment considerations include:
- Pharmacology: Anticoagulation (heparin, warfarin (Coumadin)).
- Catheter removal.
- Thrombolytic therapy.
- Surgical compression of the thoracic inlet with or without venous reconstruction.
- Conservative treatment.
- Ultrasound is used in vascular intervention such as thrombolysis and thrombectomy. This may involve intra-procedural guidance/technical evaluation, and/or post-procedure assessment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.