Podcast
Questions and Answers
What role does norepinephrine play in the control of heart activity during exercise?
What role does norepinephrine play in the control of heart activity during exercise?
- It stimulates vasoconstrictive response. (correct)
- It directly increases the heart rate. (correct)
- It inhibits the vasomotor center.
- It enhances the effect of vasodilation.
What initiates the baroreceptor reflex for arterial pressure control?
What initiates the baroreceptor reflex for arterial pressure control?
- Reductions in blood flow
- Decreased muscle activity
- Changes in metabolic demand
- Increased arterial pressure (correct)
Which area of the nervous system is primarily responsible for increasing arterial pressure during exercise?
Which area of the nervous system is primarily responsible for increasing arterial pressure during exercise?
- Cerebral cortex
- Reticular activating system (correct)
- Peripheral nervous system
- Autonomic nervous system
What mechanism primarily leads to vasodilation in muscle vasculature during increased metabolism?
What mechanism primarily leads to vasodilation in muscle vasculature during increased metabolism?
What effect does the activation of cardio-acceleratory areas have during heavy exercise?
What effect does the activation of cardio-acceleratory areas have during heavy exercise?
What is the primary function of the vasomotor center in the brain?
What is the primary function of the vasomotor center in the brain?
Which neurotransmitter is mainly involved in the actions of the vasomotor center?
Which neurotransmitter is mainly involved in the actions of the vasomotor center?
How does the vagus nerve influence heart activity?
How does the vagus nerve influence heart activity?
Which of the following areas is primarily associated with the vasodilator mechanisms?
Which of the following areas is primarily associated with the vasodilator mechanisms?
What area of the brain does the vasomotor center mainly reside in?
What area of the brain does the vasomotor center mainly reside in?
Which of the following is not a function of the vasomotor center?
Which of the following is not a function of the vasomotor center?
Which system primarily works alongside the vasomotor center to control circulation?
Which system primarily works alongside the vasomotor center to control circulation?
What effect does vasoconstriction primarily have on blood vessels?
What effect does vasoconstriction primarily have on blood vessels?
What is the primary result of excitation in the posterolateral portions of the hypothalamus?
What is the primary result of excitation in the posterolateral portions of the hypothalamus?
How does the anterior portion of the hypothalamus influence vasomotor activity?
How does the anterior portion of the hypothalamus influence vasomotor activity?
What is the rate at which sympathetic vasoconstrictor nerve fibers fire under normal conditions?
What is the rate at which sympathetic vasoconstrictor nerve fibers fire under normal conditions?
What effect does stimulation of the cortical motor area have on the vasomotor center?
What effect does stimulation of the cortical motor area have on the vasomotor center?
What is the term used to describe the partial state of constriction in blood vessels maintained during normal conditions?
What is the term used to describe the partial state of constriction in blood vessels maintained during normal conditions?
What happens when a spinal anesthetic is administered in relation to sympathetic nerve impulses?
What happens when a spinal anesthetic is administered in relation to sympathetic nerve impulses?
What areas of the brain can influence the vasomotor center?
What areas of the brain can influence the vasomotor center?
Which brain structures are mentioned to have an excitatory or inhibitory effect on the vasomotor center?
Which brain structures are mentioned to have an excitatory or inhibitory effect on the vasomotor center?
What could be the result of increased sympathetic vasoconstrictor tone?
What could be the result of increased sympathetic vasoconstrictor tone?
Which of the following best describes the relationship between the hypothalamus and cardiovascular function?
Which of the following best describes the relationship between the hypothalamus and cardiovascular function?
What is the primary function of the vasodilator area located in the medulla?
What is the primary function of the vasodilator area located in the medulla?
What role does the vasomotor center play in the body?
What role does the vasomotor center play in the body?
How does increased vasoconstriction typically affect heart activity?
How does increased vasoconstriction typically affect heart activity?
Which nerves primarily send sensory signals to the nucleus tractus solitarius?
Which nerves primarily send sensory signals to the nucleus tractus solitarius?
What is the effect of the reticular substance's lateral neurons on the vasomotor center?
What is the effect of the reticular substance's lateral neurons on the vasomotor center?
What distinct ability does the hypothalamus have regarding the vasomotor center?
What distinct ability does the hypothalamus have regarding the vasomotor center?
What generally happens to heart activity when the vasoconstrictor system is inhibited?
What generally happens to heart activity when the vasoconstrictor system is inhibited?
Which part of the central nervous system influences the activities of the vasomotor center?
Which part of the central nervous system influences the activities of the vasomotor center?
Which area is identified as the sensory area controlling the vasomotor center?
Which area is identified as the sensory area controlling the vasomotor center?
What is the relationship between the vasomotor center's activity and arterial pressure regulation?
What is the relationship between the vasomotor center's activity and arterial pressure regulation?
What effect does norepinephrine have on arterial pressure?
What effect does norepinephrine have on arterial pressure?
Which part of the vasomotor center is responsible for increasing heart pumping activities?
Which part of the vasomotor center is responsible for increasing heart pumping activities?
How does the vasomotor center decrease heart rate?
How does the vasomotor center decrease heart rate?
What happens when norepinephrine is destroyed?
What happens when norepinephrine is destroyed?
Which mechanism is primarily involved in controlling vascular constriction?
Which mechanism is primarily involved in controlling vascular constriction?
What effect does spinal anesthesia have on arterial pressure?
What effect does spinal anesthesia have on arterial pressure?
What role does the sympathetic nervous system play in heart activity during increased demands?
What role does the sympathetic nervous system play in heart activity during increased demands?
What does the term 'vasomotor tone' refer to?
What does the term 'vasomotor tone' refer to?
How do the dorsal motor nuclei of the vagus nerves influence heart activity?
How do the dorsal motor nuclei of the vagus nerves influence heart activity?
What is the primary response when the need to decrease heart pumping arises?
What is the primary response when the need to decrease heart pumping arises?
What is the primary area of the vasomotor center responsible for producing vasoconstrictor impulses?
What is the primary area of the vasomotor center responsible for producing vasoconstrictor impulses?
Which of the following best explains the function of sympathetic vasoconstrictor fibers?
Which of the following best explains the function of sympathetic vasoconstrictor fibers?
How does norepinephrine primarily function in the body?
How does norepinephrine primarily function in the body?
What area influences the distribution of vasoconstrictor impulses throughout the body?
What area influences the distribution of vasoconstrictor impulses throughout the body?
What characterizes the sympathetic vasoconstrictor system in relation to the total vascular system?
What characterizes the sympathetic vasoconstrictor system in relation to the total vascular system?
Which area of the brain is primarily responsible for regulating sympathetic vasoconstrictor activity?
Which area of the brain is primarily responsible for regulating sympathetic vasoconstrictor activity?
What effect does stimulation of the vasodilator center in the brain generally have on blood vessels?
What effect does stimulation of the vasodilator center in the brain generally have on blood vessels?
What primary action does the vagus nerve perform in relation to the heart?
What primary action does the vagus nerve perform in relation to the heart?
Which statement best describes the role of the sympathetic chain in relation to heart activity?
Which statement best describes the role of the sympathetic chain in relation to heart activity?
How does the activation of the vasomotor center generally influence blood pressure?
How does the activation of the vasomotor center generally influence blood pressure?
What happens to sympathetic discharge when baroreceptor signals inhibit secondary signals in the medulla?
What happens to sympathetic discharge when baroreceptor signals inhibit secondary signals in the medulla?
Which body part experiences minimized pressure decrease after baroreceptor signals are processed?
Which body part experiences minimized pressure decrease after baroreceptor signals are processed?
What is the primary physiological function of the nucleus tractus solitarius?
What is the primary physiological function of the nucleus tractus solitarius?
When baroreceptors are denervated, what is the expected outcome on arterial pressure control?
When baroreceptors are denervated, what is the expected outcome on arterial pressure control?
How is the sympathetic nervous system generally affected by baroreceptor activation?
How is the sympathetic nervous system generally affected by baroreceptor activation?
What percentage of occurrence would likely be noted when arterial pressure readings are taken?
What percentage of occurrence would likely be noted when arterial pressure readings are taken?
Which of the following best describes the relationship between baroreceptor signaling and vascular function?
Which of the following best describes the relationship between baroreceptor signaling and vascular function?
What is a likely physiological consequence of strong sympathetic discharge throughout the body?
What is a likely physiological consequence of strong sympathetic discharge throughout the body?
What change is likely seen in the interaction between secondary signals and arterial pressure regulation?
What change is likely seen in the interaction between secondary signals and arterial pressure regulation?
In the context of a pressure change, how do primary and secondary signals interact?
In the context of a pressure change, how do primary and secondary signals interact?
Hering's nerve is associated with the regulation of arterial pressure through baroreceptors.
Hering's nerve is associated with the regulation of arterial pressure through baroreceptors.
The internal carotid artery is primarily a sensory pathway for the glossopharyngeal nerve.
The internal carotid artery is primarily a sensory pathway for the glossopharyngeal nerve.
The carotid body acts as a chemoreceptor detecting changes in blood oxygen levels.
The carotid body acts as a chemoreceptor detecting changes in blood oxygen levels.
The vagus nerve is not involved in the baroreceptor system for controlling arterial pressure.
The vagus nerve is not involved in the baroreceptor system for controlling arterial pressure.
The common carotid artery bifurcates into the internal and external carotid arteries.
The common carotid artery bifurcates into the internal and external carotid arteries.
Sympathetic stimulation decreases heart rate and contractility.
Sympathetic stimulation decreases heart rate and contractility.
The parasympathetic nervous system plays a minor role in regulating the heart compared to the sympathetic nervous system.
The parasympathetic nervous system plays a minor role in regulating the heart compared to the sympathetic nervous system.
Sympathetic nerve fibers originate solely in the lumbar region of the spinal cord.
Sympathetic nerve fibers originate solely in the lumbar region of the spinal cord.
Parasympathetic nerve fibers to the heart are mainly carried by the vagus nerves.
Parasympathetic nerve fibers to the heart are mainly carried by the vagus nerves.
The sympathetic nervous system has no influence on the vascular function in most tissues.
The sympathetic nervous system has no influence on the vascular function in most tissues.
Baroreceptors respond more rapidly to stationary pressure than to rapidly changing pressure.
Baroreceptors respond more rapidly to stationary pressure than to rapidly changing pressure.
The baroreceptor feedback mechanism is least effective at arterial pressures around 150 mm Hg.
The baroreceptor feedback mechanism is least effective at arterial pressures around 150 mm Hg.
A decrease in arterial pressure can lead to loss of consciousness if not corrected quickly.
A decrease in arterial pressure can lead to loss of consciousness if not corrected quickly.
The carotid sinus reflex operates by raising the aortic pressure immediately during a decrease in arterial pressure.
The carotid sinus reflex operates by raising the aortic pressure immediately during a decrease in arterial pressure.
The rate of impulse firing from baroreceptors increases during diastole.
The rate of impulse firing from baroreceptors increases during diastole.
Baroreceptors help maintain constant arterial pressure when a person changes from lying down to standing up.
Baroreceptors help maintain constant arterial pressure when a person changes from lying down to standing up.
An acute rise in mean arterial pressure does not significantly impact the rate of impulse transmission in baroreceptors.
An acute rise in mean arterial pressure does not significantly impact the rate of impulse transmission in baroreceptors.
Baroreceptors do not respond to changes in pressure within a fraction of a second.
Baroreceptors do not respond to changes in pressure within a fraction of a second.
The body's ability to adjust arterial pressure does not vary based on the individual’s posture.
The body's ability to adjust arterial pressure does not vary based on the individual’s posture.
A temporary overcompensation occurs when arterial pressure changes due to the baroreceptor reflex.
A temporary overcompensation occurs when arterial pressure changes due to the baroreceptor reflex.
Match the following hormones with their primary effects on blood vessels:
Match the following hormones with their primary effects on blood vessels:
Match the following effects with their corresponding physiological changes in response to sympathetic nervous system activation:
Match the following effects with their corresponding physiological changes in response to sympathetic nervous system activation:
Match the following terms with their definitions:
Match the following terms with their definitions:
Match the following components of the nervous system with their roles in arterial pressure modulation:
Match the following components of the nervous system with their roles in arterial pressure modulation:
Match the following outcomes with their related mechanisms during sudden changes in arterial pressure:
Match the following outcomes with their related mechanisms during sudden changes in arterial pressure:
Match the following physiological responses to their corresponding triggers:
Match the following physiological responses to their corresponding triggers:
Match the following agents with their roles in controlling arterial pressure:
Match the following agents with their roles in controlling arterial pressure:
Match the following terms with their definitions:
Match the following terms with their definitions:
Match the following physiological reactions to their characteristics:
Match the following physiological reactions to their characteristics:
Match the following concepts with their effects on blood flow:
Match the following concepts with their effects on blood flow:
Study Notes
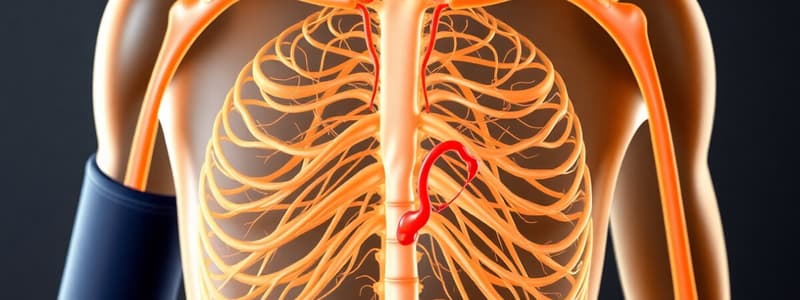
Vasomotor Center
- Located in the reticular substance of the medulla and lower portion of the pons
- Responsible for controlling vasoconstriction and vasodilation, and regulating heart activity
- Contains three areas: vasoconstrictor, vasodilator, and sensory.
Sympathetic Vasomotor Tone
- Continuous signals from the vasoconstrictor area of the vasomotor center to sympathetic vasoconstrictor nerve fibers lead to partial constriction of blood vessels
- This helps maintain a baseline level of blood pressure
- Spinal anesthesia blocks sympathetic nerve impulses, demonstrating the effect of vasoconstrictor tone on arterial pressure.
Control of the Vasomotor Center
- Higher brain centers (hypothalamus, cerebral cortex) can excite or inhibit the vasomotor center, influencing blood pressure and heart rate
- The hypothalamus has a significant role, with the posterolateral portions causing excitation and the anterior portion causing either excitation or inhibition.
- Stimulation of the motor cortex excites the vasomotor center, increasing heart rate and arterial pressure.
Functions of the Vasomotor Center
- Regulation of vascular tone through vasoconstriction and vasodilation
- Regulation of heart rate and strength of contractions through sympathetic and parasympathetic nerve fibers
- Control of blood pressure under various conditions, including exercise and stress
- Coordination of cardiovascular responses through its interplay with higher brain centers.
Baroreceptor Arterial Pressure Control
- Baroreceptors, located in large arteries, detect changes in blood pressure
- Increased blood pressure stretches baroreceptors, triggering signals to the CNS
- The CNS then sends feedback signals to the vasomotor center, adjusting heart rate and blood vessel constriction to maintain normal blood pressure.
- This is a negative feedback mechanism, meaning it reduces the stimulus that initiated it.
Sympathetic Nerve Control During Exercise
- During exercise, the vasomotor center increases sympathetic activity, leading to increased vasoconstriction, heart rate, and contractility
- This helps deliver more oxygen and nutrients to working muscles.
Anatomy of the Vasomotor Center
- The vasomotor center is located in the reticular substance of the medulla and lower third of the pons.
- It transmits parasympathetic impulses through the vagus nerves to the heart.
- It transmits sympathetic impulses through the spinal cord and peripheral sympathetic nerves to arteries, arterioles, and veins throughout the body.
- Sympathetic nerves carry vasoconstrictor nerve fibers (more numerous) and a few vasodilator fibers.
- The sympathetic vasoconstrictor effect is strongest in the kidneys, intestines, spleen, and skin.
Important Areas of the Vasomotor Center
- Vasoconstrictor area: located bilaterally in the anterolateral portions of the upper medulla.
- Neurons from this area distribute fibers throughout the body.
- Vasodilator area: located mainly in the lower medulla.
- Neurons from this area project to sympathetic vasoconstrictor neurons and inhibit vasoconstriction.
Neural Control of Blood Pressure
- The vasomotor center controls blood pressure by adjusting the degree of sympathetic vasoconstriction.
- Increased sympathetic discharge (e.g., during excitement, exercise) constricts blood vessels, increasing blood pressure.
- Decreased sympathetic discharge (e.g., during sleep) relaxes blood vessels, decreasing blood pressure.
Baroreceptors and Blood Pressure Regulation
- Baroreceptors: sensory receptors in the aortic arch and carotid sinuses that detect changes in blood pressure.
- Baroreceptor reflex: Responds to changes in blood pressure to regulate it.
- Mechanism of Baroreceptor Reflex:
- An increase in blood pressure stretches the baroreceptors.
- Impulses from the baroreceptors travel to the vasomotor center.
- Signals from the vasomotor center inhibit sympathetic vasoconstrictor activity and increase vagal activity to the heart.
- This results in vasodilation, decreased heart rate, and decreased blood pressure.
- Baroreceptor system as a pressure buffer:
- Prevents rapid changes in blood pressure.
- Reduces minute-to-minute fluctuations in blood pressure.
Denervated Baroreceptor System
- After denervation, baroreceptors are less effective at regulating blood pressure.
- This results in higher fluctuations in blood pressure.
Chemoreceptors and Blood Pressure Regulation
- Chemoreceptors: sensory receptors in the aortic arch and carotid bodies that detect changes in blood oxygen, carbon dioxide, and pH levels.
- Chemoreceptor reflex: Responds to changes in blood gas levels to regulate blood pressure.
- Mechanism of Chemoreceptor Reflex:
- Decrease in blood oxygen, increase in carbon dioxide, or decrease in pH stimulates chemoreceptors.
- Signals from the chemoreceptors travel to the vasomotor center.
- The vasomotor center increases sympathetic vasoconstrictor activity, increasing blood pressure.
CNS Ischemic Response
- Mechanism:
- Increase in intracranial pressure compresses cerebral vessels.
- This triggers a CNS ischemic pressure response.
- The vasomotor center increases sympathetic vasoconstrictor activity, increasing blood pressure.
- This alleviates cerebral ischemia.
- The CNS ischemic pressure response is a powerful mechanism to increase blood pressure in extreme cases of cerebral ischemia.
Autonomic Nervous System and Circulation Regulation
- The sympathetic nervous system plays a major role in circulatory regulation, increasing heart rate and contractility.
- Sympathetic fibers directly connect to the heart, enhancing its pumping action.
- Parasympathetic fibers influence cardiovascular function, mainly by controlling heart rate via the vagus nerve.
- Parasympathetic stimulation decreases heart rate and contractility.
Baroreceptors and Blood Pressure Regulation
- Baroreceptors, located in the carotid sinuses and aortic arch, sense changes in arterial pressure.
- Baroreceptor activation triggers a reflex that adjusts heart rate, vessel constriction, and blood pressure.
- The baroreceptor reflex helps maintain stable arterial pressure during postural changes, preventing dizziness upon standing.
Chemoreceptors and Arterial Pressure Regulation
- Chemoreceptors, located in the carotid bodies and aortic bodies, sense changes in oxygen, carbon dioxide, and hydrogen ion levels.
- Chemoreceptor activation triggers a reflex that modifies blood pressure, contributing to respiratory control.
Atrial Reflexes and Volume Regulation
- Atrial stretch receptors respond to increased atrial pressure, which often signifies increased blood volume.
- Atrial reflex activation reduces renal sympathetic nerve activity, promoting diuresis and blood volume regulation.
Nervous System Control Mechanisms and Oscillations
- Oscillations in arterial pressure, known as vasomotor waves, can be caused by fluctuations in baroreceptor and chemoreceptor reflexes.
- Delays in feedback responses can lead to oscillations in control systems, as seen in the example of an airplane's automatic pilot.
Sympathetic Vasoconstriction
- The sympathetic nervous system utilizes norepinephrine as the primary vasoconstrictor neurotransmitter.
- Norepinephrine directly acts on alpha-adrenergic receptors in vascular smooth muscle, leading to vasoconstriction.
- Adrenal medullae play a vital role in the sympathetic vasoconstrictor system.
- Sympathetic impulses stimulate the adrenal medullae, causing the release of epinephrine and norepinephrine into the bloodstream.
- These hormones act on all blood vessels, generally causing vasoconstriction.
- Notably, epinephrine can also cause vasodilation in some tissues due to its stimulation of beta-adrenergic receptors.
- A notable exception to vasoconstriction is the potential for sympathetic vasodilation in skeletal muscles during initial stages of exercise. This may be mediated by epinephrine or nitric oxide released from the vascular endothelium.
- Emotional fainting (vasovagal syncope) involves activation of the muscle vasodilator system and vagal heart inhibition, resulting in a rapid drop in arterial pressure.
- The drop in pressure reduces blood flow to the brain, leading to loss of consciousness, beginning with disturbing thoughts.
Role of the Nervous System in Rapid Arterial Pressure Control
- The nervous system is crucial for rapid increases in arterial pressure.
- The sympathetic nervous system coordinates vasoconstriction and cardioacceleration.
- This response involves simultaneous inhibition of parasympathetic vagal signals to the heart.
- Three major changes occur simultaneously:
- Systemic arterioles constrict, increasing total peripheral resistance and raising arterial pressure.
- Veins (and other large vessels) are strongly constricted, further contributing to the pressure rise.
- The rapid response of nervous control makes it a vital mechanism for immediate pressure regulation.
- Within seconds of stimulation, arterial pressure can rise significantly.
- Conversely, inhibiting nervous stimulation can quickly decrease arterial pressure by up to half within seconds.
Pressure Buffer Function of the Baroreceptor Control System
- The baroreceptor system opposes fluctuations in arterial pressure, acting as a pressure buffer.
- The nerves connecting the baroreceptors to the central nervous system are referred to as “buffer nerves.”
- Denervation of baroreceptors results in significantly increased variability in arterial pressure, demonstrating the importance of this system.
- The system greatly reduces minute-to-minute variations in pressure.
Baroreceptors and Long-Term Regulation
- The significance of baroreceptors in long-term regulation of arterial pressure remains controversial.
- Baroreceptors have been suggested to “reset” after 1 to 2 days to the prevailing pressure level, potentially reducing their long-term effectiveness.
- Despite resetting, studies suggest a persistent contribution of baroreceptors to long-term pressure control.
Chemoreceptor Reflex
- The chemoreceptor reflex can also oscillate, often alongside the baroreceptor reflex.
- The chemoreceptor reflex primarily influences vasomotor waves at low arterial pressures.
- It is important at pressure ranges of 40 to 80 mm Hg, while baroreceptor control weakens.
CNS Ischemic Pressure Control Mechanism
- Oscillation of the CNS ischemic pressure control mechanism occurs during cerebral ischemia.
- Cerebrospinal fluid pressure elevation causes compression of cerebral vessels, initiating a sympathetic surge to restore blood flow.
- When pressure rises, the sympathetic system becomes inactive.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the structure and function of the vasomotor center, including its role in controlling vasoconstriction and vasodilation. It explores how sympathetic vasomotor tone affects blood pressure and the influence of higher brain centers on the vasomotor center's activity. Test your knowledge on these physiological processes.