Podcast
Questions and Answers
What is the primary goal of medical management for pelvic inflammatory disease?
What is the primary goal of medical management for pelvic inflammatory disease?
- To restore fertility
- To control and eradicate the infection, preventing it from spreading to other systems (correct)
- To prevent the development of adhesions and strictures
- To reduce pain and inflammation
Which of the following is a common diagnostic test used to evaluate pelvic inflammatory disease?
Which of the following is a common diagnostic test used to evaluate pelvic inflammatory disease?
- Laparoscopic visualization (correct)
- Electrocardiogram (ECG)
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) scan
Which of the following antibiotics is commonly used to treat pelvic inflammatory disease?
Which of the following antibiotics is commonly used to treat pelvic inflammatory disease?
- Azithromycin
- Amoxicillin
- Cefoxitin (Mefoxin) (correct)
- Ciprofloxacin
What is the importance of evaluating and treating the sexual partner of a client with pelvic inflammatory disease?
What is the importance of evaluating and treating the sexual partner of a client with pelvic inflammatory disease?
Which of the following nursing implications is most important when caring for a client with pelvic inflammatory disease?
Which of the following nursing implications is most important when caring for a client with pelvic inflammatory disease?
Which of the following is a potential complication of pelvic inflammatory disease?
Which of the following is a potential complication of pelvic inflammatory disease?
What is the significance of pelvic inflammatory disease for a client's fertility?
What is the significance of pelvic inflammatory disease for a client's fertility?
Which of the following is an important aspect of patient and family teaching for a client with pelvic inflammatory disease?
Which of the following is an important aspect of patient and family teaching for a client with pelvic inflammatory disease?
What is the role of corticosteroids in the treatment of pelvic inflammatory disease?
What is the role of corticosteroids in the treatment of pelvic inflammatory disease?
What is the most common causative organism for pelvic inflammatory disease?
What is the most common causative organism for pelvic inflammatory disease?
Which of the following is NOT a risk-increasing behavior for cervicitis?
Which of the following is NOT a risk-increasing behavior for cervicitis?
Which of the following is a common clinical manifestation of cervicitis?
Which of the following is a common clinical manifestation of cervicitis?
What is the primary goal of treatment for vaginal infections?
What is the primary goal of treatment for vaginal infections?
Which of the following is a common cause of senile/atrophic vaginitis?
Which of the following is a common cause of senile/atrophic vaginitis?
What medical management is recommended for senile/atrophic vaginitis?
What medical management is recommended for senile/atrophic vaginitis?
Which of the following is NOT a potential cause of pelvic inflammatory disease?
Which of the following is NOT a potential cause of pelvic inflammatory disease?
What is a common clinical manifestation of pelvic inflammatory disease?
What is a common clinical manifestation of pelvic inflammatory disease?
Which organism is most commonly associated with simple vaginitis?
Which organism is most commonly associated with simple vaginitis?
What is a common clinical manifestation of simple vaginitis?
What is a common clinical manifestation of simple vaginitis?
What is the typical appearance of the exudate in cases of trichomoniasis?
What is the typical appearance of the exudate in cases of trichomoniasis?
Which factor is important to assess in the subjective assessment of simple vaginitis?
Which factor is important to assess in the subjective assessment of simple vaginitis?
What is the typical appearance of the exudate in cases of candidiasis?
What is the typical appearance of the exudate in cases of candidiasis?
Which factor is important to assess in the objective assessment of simple vaginitis?
Which factor is important to assess in the objective assessment of simple vaginitis?
What is a common symptom of simple vaginitis that worsens with voiding or defecating?
What is a common symptom of simple vaginitis that worsens with voiding or defecating?
Which factor is important to assess in the subjective assessment of simple vaginitis?
Which factor is important to assess in the subjective assessment of simple vaginitis?
Study Notes
Simple Vaginitis
- Caused by bacterial or inflammatory organisms, including E. coli, Trichomonas vaginalis, Gardnerella, and Candida albicans
- Risk factors include infrequent changing of pads or tampons
- Clinical manifestations include:
- Pruritis
- Burning
- Edema of surrounding tissue
- Dysuria
- Exudate (yellow, white, grayish white, or curd-like)
- Symptoms worsen with voiding or defecating
- Assessment includes:
- Menstrual history
- Birth control methods
- Current medications
- Family history of diabetes
- History of vaginal infections or STIs
- Sexual history
- Diagnostic tests include:
- Gram stain of secretions
- Culture and sensitivity of secretions
- Laparoscopic visualization
- Vaginal ultrasound
- Leukocyte count
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein
Medical Management
- Goal is to control and eradicate infection, preventing spread to other systems
- Treatment includes:
- Systemic antibiotics (intravenously or intramuscularly)
- Corticosteroid to reduce inflammation
- Intercourse avoidance during treatment
- Sexual partner evaluation and treatment
- Pain control, rest, and adequate fluid intake
Nursing Implications and Patient Teaching
- Client is usually hospitalized
- Observe standard precautions
- Assess for pain and administer analgesics as ordered
- Monitor vital signs and progress of treatment
- Provide fluids and monitor fluid status
- Palliative measures for comfort (bathing, changing pads, perineal hygiene, warm douching)
- Support client with positive, non-judgmental attitude
- Patient education includes:
- Signs and symptoms to report to healthcare provider
- Importance of compliance with medication therapy
- Importance of hand washing and personal hygiene
- Importance of sexual partner evaluation and treatment
Prognosis
- Complications may include:
- Adhesions and strictures of fallopian tubes
- Ectopic pregnancy
- Infertility
- Risk of recurrence is elevated if sexual partner is not treated
Senile Vaginitis or Atrophic Vaginitis
- Caused by low estrogen levels, leading to thinning and atrophy of vulva and vagina
- Common after menopause
- Vagina is more susceptible to bacterial invasions
- Treatment includes:
- Estrogen, vaginal suppositories, and ointments
- Goals of treatment include:
- Curing infection
- Preventing reinfection
- Preventing complications
- Preventing infection of sexual partner
Cervicitis
- Inflammation of the cervix
- Causes include:
- Vaginal infections
- Sexually transmitted infections (STIs)
- Allergic reaction to cervical caps, diaphragms, pessary devices, condoms, douches, or spermicides
- Clinical manifestations include:
- Gray, white, or yellow vaginal discharge
- Dyspareunia (painful intercourse)
- Vaginal pain
- Pelvic heaviness
- Abnormal vaginal bleeding
- Treatment includes:
- Specific to causative organism
- Local vaginal application of suppositories, ointments, and creams
- Oral medication (e.g., Azithromycin or Doxycycline)
- Nursing implications and patient teaching include:
- Washing hands before and after vaginal applications
- Using vaginal medications at bedtime and remaining recumbent for more than 30 minutes
- Promoting personal hygiene and frequent warm baths
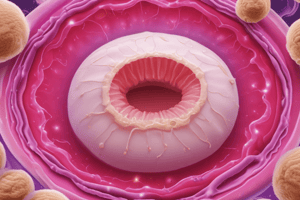
Pelvic Inflammatory Disease
- Any acute, subacute, recurrent, or chronic infection of the cervix, ovaries, fallopian tubes, or uterus
- Causes include:
- Bacterial or inflammatory organisms
- Cervical mucus destruction or alteration
- Ascending infection into the uterine cavity and other reproductive structures
- Clinical manifestations include:
- Elevation in temperature
- Chills
- Severe abdominal pain
- Malaise
- Nausea and vomiting
- Malodorous vaginal exudate (purulent to thin and mucoid)
- Lower abdominal pain, pelvic pain, dysmenorrhea, dysuria, and vulvar pruritis
- Assessment includes:
- Severity of the disorder
- Pain
- Time of onset
- Frequency (primary infection or continuous reinfection)
- Sexual history
- Recent pelvic examinations or procedures
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge on the etiology and pathophysiology of Vaginitis, including the various organisms that can cause it and the clinical manifestations associated with the condition. Learn about common causes like Escherichia coli, Trichomonas vaginalis, Gardnerella bacillus, and Candida albicans.