Podcast
Questions and Answers
What is the primary stimuli for renin release in the kidney?
What is the primary stimuli for renin release in the kidney?
- Reduction of renal perfusion pressure (correct)
- High sodium intake
- Increased renal perfusion pressure
- Hyponatremia
Which hormone stimulates the production of red blood cells in the bone marrow?
Which hormone stimulates the production of red blood cells in the bone marrow?
- Renin
- Erythropoietin (correct)
- Anti diuretic hormone (ADH)
- Vitamin D
What is the function of anti diuretic hormone (ADH) in the urinary system?
What is the function of anti diuretic hormone (ADH) in the urinary system?
- Activate vitamin D to its active form
- Stimulate formation of red blood cells in the bone marrow
- Control water excretion in the tubules (correct)
- Regulate acid base balance of the blood
Which component of fluid gain and loss is considered 'insensible' and not visible?
Which component of fluid gain and loss is considered 'insensible' and not visible?
Which of the following is a potential complication of acute renal failure (ARF)?
Which of the following is a potential complication of acute renal failure (ARF)?
What is the widely accepted criterion for ARF?
What is the widely accepted criterion for ARF?
Which diagnostic test is a critical component of the evaluation of patients with renal failure?
Which diagnostic test is a critical component of the evaluation of patients with renal failure?
What is the final stage of chronic kidney disease (CKD) known as?
What is the final stage of chronic kidney disease (CKD) known as?
What are the risk factors for end-stage renal disease (ESKD)?
What are the risk factors for end-stage renal disease (ESKD)?
Which of the following is a sign or symptom of chronic kidney disease (CKD)?
Which of the following is a sign or symptom of chronic kidney disease (CKD)?
What does a GFR of 30–59 mL/min represent in the stages of chronic kidney disease?
What does a GFR of 30–59 mL/min represent in the stages of chronic kidney disease?
Which of the following is used as a treatment for acute renal failure?
Which of the following is used as a treatment for acute renal failure?
What are the risk factors for urinary tract infection?
What are the risk factors for urinary tract infection?
Which symptoms are associated with urinary tract infection?
Which symptoms are associated with urinary tract infection?
What diagnostic test is used for assessing the urinary system?
What diagnostic test is used for assessing the urinary system?
Which medical term is related to involuntary leakage of urine?
Which medical term is related to involuntary leakage of urine?
What factors can influence the elimination pattern in relation to the urinary system?
What factors can influence the elimination pattern in relation to the urinary system?
Which assessment technique involves checking for any mass or tenderness in the urinary system?
Which assessment technique involves checking for any mass or tenderness in the urinary system?
What is a commonly used treatment for urinary tract infection?
What is a commonly used treatment for urinary tract infection?
Which factor is not associated with an increased risk of urinary tract infection?
Which factor is not associated with an increased risk of urinary tract infection?
Which type of pain is commonly associated with urinary tract infection?
Which type of pain is commonly associated with urinary tract infection?
What is used to assess fluid loss in the body?
What is used to assess fluid loss in the body?
Which of the following is a common etiology for the formation of stones in the kidney, bladder, and/or urethra?
Which of the following is a common etiology for the formation of stones in the kidney, bladder, and/or urethra?
What type of calculi can be found in the kidney, bladder, and/or urethra?
What type of calculi can be found in the kidney, bladder, and/or urethra?
Which diagnostic test is commonly used to identify urolithiasis?
Which diagnostic test is commonly used to identify urolithiasis?
What is a clinical manifestation of nephrosclerosis?
What is a clinical manifestation of nephrosclerosis?
What is a characteristic manifestation of polycystic kidney disease?
What is a characteristic manifestation of polycystic kidney disease?
What is the primary cause of hydronephrosis?
What is the primary cause of hydronephrosis?
Which phase of acute renal failure (ARF) is characterized by a rapid loss of renal function due to damage to the kidneys?
Which phase of acute renal failure (ARF) is characterized by a rapid loss of renal function due to damage to the kidneys?
What is a potential metabolic complication of acute renal failure (ARF)?
What is a potential metabolic complication of acute renal failure (ARF)?
What is a treatment method for urolithiasis involving the use of high fluid intake?
What is a treatment method for urolithiasis involving the use of high fluid intake?
What is a clinical manifestation of hydronephrosis?
What is a clinical manifestation of hydronephrosis?
What is a potential treatment for hydronephrosis involving evidence of hyperactivity and hypertrophy before dilatation and atony?
What is a potential treatment for hydronephrosis involving evidence of hyperactivity and hypertrophy before dilatation and atony?
What is a characteristic clinical manifestation of polycystic kidney disease?
What is a characteristic clinical manifestation of polycystic kidney disease?
Flashcards
Urolithiasis
Urolithiasis
Formation of stones in the kidney, bladder, and/or urethra.
Etiology of Urolithiasis
Etiology of Urolithiasis
Immobility, hypercalcemia, UTIs, urine stasis, and fractures.
Calculi composition
Calculi composition
Calcium oxalate, calcium phosphate, or uric acid.
Urolithiasis manifestations
Urolithiasis manifestations
Signup and view all the flashcards
Urolithiasis diagnosis
Urolithiasis diagnosis
Signup and view all the flashcards
Urolithiasis management
Urolithiasis management
Signup and view all the flashcards
Nephrosclerosis
Nephrosclerosis
Signup and view all the flashcards
Clinical manifestations of Nephrosclerosis
Clinical manifestations of Nephrosclerosis
Signup and view all the flashcards
Nephrosclerosis treatment
Nephrosclerosis treatment
Signup and view all the flashcards
Polycystic kidney disease
Polycystic kidney disease
Signup and view all the flashcards
Polycystic kidney disease manifestations
Polycystic kidney disease manifestations
Signup and view all the flashcards
Hydronephrosis
Hydronephrosis
Signup and view all the flashcards
Causes of Hydronephrosis
Causes of Hydronephrosis
Signup and view all the flashcards
Hydronephrosis symptoms
Hydronephrosis symptoms
Signup and view all the flashcards
Hydronephrosis diagnosis
Hydronephrosis diagnosis
Signup and view all the flashcards
Hydronephrosis treatment
Hydronephrosis treatment
Signup and view all the flashcards
Acute Renal Failure (ARF)
Acute Renal Failure (ARF)
Signup and view all the flashcards
ARF complications
ARF complications
Signup and view all the flashcards
ARF categories
ARF categories
Signup and view all the flashcards
ARF phases
ARF phases
Signup and view all the flashcards
Study Notes
- Urolithiasis is the formation of stones in the kidney, bladder, and/or urethra. More common in males, recurrence rate is 50% at 10 years.
- Etiology includes immobility, hypercalcemia, UTIs, urine stasis, and fractures. Calculi can be made of calcium oxalate, calcium phosphate, or uric acid.
- Clinical manifestations vary depending on location: kidney pelvis, urter, or bladder. Symptoms include acute pain, nausea, vomiting, fever, chills, and microscopic hematuria.
- Diagnostic tests include KUB radiograph, IVP, and renal ultrasonography. Management includes monitoring fluid intake/output, prescribed pain medication, antibiotic therapy, and diet modifications.
- Treatment methods include intravenous pain medication, relaxation exercises, hot baths, high fluid intake, antiemetics, hospital admission, lithotripsy, ureteroscopy, stone dissolution, and nephrolithotomy.
- Nephrosclerosis is the hardening of the kidney and can lead to renal failure. Hypertensive retinal changes, proteinuria, and decreased urine output are clinical manifestations. Treatment includes antihypertensive drugs and lifestyle modifications.
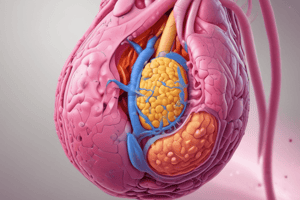
- Polycystic kidney disease is a hereditary condition with numerous fluid-filled cysts on the kidney, causing gradual destruction of function. Manifestations include flank pain, hematuria, and proteinuria, leading to end-stage renal disease and requiring dialysis or kidney transplantation.
- Hydronephrosis is the abnormal dilation of the renal pelvis and calyces due to congenital urethral obstruction, cancer, or other causes. It shows evidence of hyperactivity and hypertrophy before dilatation and atony. Symptoms are acute (colicky flank pain, hematuria, pyuria, fever, nausea and vomiting, abdominal pain) or chronic (intermittent dull flank pain, hematuria, pyuria, fever, palpable mass). Diagnosis is through ultrasound, CT scan, or cystoscopy, and treatment involves stents or urine diversion to ensure urinary drainage.
- Acute renal failure (ARF) is a rapid loss of renal function due to damage to the kidneys. Depending on duration and severity, ARF can lead to metabolic complications such as metabolic acidosis and fluid/electrolyte imbalances. ARF has three major categories: prerenal (hypoperfusion of kidney), intrarenal (damage to kidney tissue), and postrenal (obstruction to urine flow). ARF goes through four phases: initiation, oliguria, diuresis, and recovery.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.