Podcast
Questions and Answers
What is the primary role of the urinary system?
What is the primary role of the urinary system?
- To absorb nutrients
- To produce hormones
- To digest food
- To ensure optimal properties of blood (correct)
What is one of the functions of the kidneys in regulating the balance between water and electrolytes?
What is one of the functions of the kidneys in regulating the balance between water and electrolytes?
- Regulating the levels of inorganic ions such as sodium (correct)
- Reabsorbing bicarbonate from urine
- Excreting hydrogen ions from urine
- Producing vitamin D
What is the role of the kidneys in maintaining pH balance?
What is the role of the kidneys in maintaining pH balance?
- Excreting hydrogen ions and reabsorbing bicarbonate from urine (correct)
- Releasing excess water and electrolytes
- Maintaining blood pressure
- Synthesizing glucose from amino acids
What is the function of the enzyme renin?
What is the function of the enzyme renin?
What is the function of the kidneys in conversion of vitamin D?
What is the function of the kidneys in conversion of vitamin D?
What do the kidneys do during periods of fasting or starvation?
What do the kidneys do during periods of fasting or starvation?
What is the function of the hilum in the kidneys?
What is the function of the hilum in the kidneys?
What covers the kidneys?
What covers the kidneys?
What is the outer layer of the kidney composed of?
What is the outer layer of the kidney composed of?
What is the function of the renal pelvis?
What is the function of the renal pelvis?
What is the term for the darker outer region of the kidney?
What is the term for the darker outer region of the kidney?
What is the function of the glomerulus?
What is the function of the glomerulus?
What is the term for the space within Bowman's capsule?
What is the term for the space within Bowman's capsule?
What is the function of the proximal convoluted tubule?
What is the function of the proximal convoluted tubule?
What is the term for the process of transporting substances from the blood into the tubular fluid?
What is the term for the process of transporting substances from the blood into the tubular fluid?
What is the term for the U-shaped structure in the nephron?
What is the term for the U-shaped structure in the nephron?
What is the final segment of the nephron?
What is the final segment of the nephron?
What is the term for the functional units that filter blood and form urine?
What is the term for the functional units that filter blood and form urine?
What is the main function of the loop of Henle?
What is the main function of the loop of Henle?
What type of epithelium lines the thin descending limb of the loop of Henle?
What type of epithelium lines the thin descending limb of the loop of Henle?
What is the function of the ureters?
What is the function of the ureters?
What type of muscle layer is found in the muscularis of the ureters?
What type of muscle layer is found in the muscularis of the ureters?
What is the function of the detrusor muscle in the urinary bladder?
What is the function of the detrusor muscle in the urinary bladder?
What type of epithelium lines the urinary bladder?
What type of epithelium lines the urinary bladder?
What is the function of the urothelium?
What is the function of the urothelium?
What is the main function of the urethra?
What is the main function of the urethra?
What is the function of peristalsis in the ureters?
What is the function of peristalsis in the ureters?
What is the function of the umbrella cells in the urothelium?
What is the function of the umbrella cells in the urothelium?
What is the function of the renal arteries?
What is the function of the renal arteries?
What is the purpose of the glomerulus?
What is the purpose of the glomerulus?
What is the function of the efferent arterioles?
What is the function of the efferent arterioles?
What is the purpose of the visceral layer of the glomerular capsule?
What is the purpose of the visceral layer of the glomerular capsule?
What is the function of the mesangial cells?
What is the function of the mesangial cells?
What is the purpose of the proximal convoluted tubule?
What is the purpose of the proximal convoluted tubule?
What is the function of the peritubular capillaries?
What is the function of the peritubular capillaries?
What is the function of the podocytes?
What is the function of the podocytes?
What is the function of the interlobular arteries?
What is the function of the interlobular arteries?
What is the function of the arcuate arteries?
What is the function of the arcuate arteries?
What is the primary function of the kidneys in regulating the balance between water and electrolytes?
What is the primary function of the kidneys in regulating the balance between water and electrolytes?
What is the role of the kidneys in excretion of metabolic wastes?
What is the role of the kidneys in excretion of metabolic wastes?
What is the function of the enzyme renin?
What is the function of the enzyme renin?
What is the function of the kidneys during periods of fasting or starvation?
What is the function of the kidneys during periods of fasting or starvation?
What is the outer layer of the kidney composed of?
What is the outer layer of the kidney composed of?
What is the function of the ureters?
What is the function of the ureters?
What is the role of the kidneys in maintaining blood pressure?
What is the role of the kidneys in maintaining blood pressure?
What is the role of the kidneys in converting vitamin D?
What is the role of the kidneys in converting vitamin D?
What is the primary function of myofibroblasts in the kidney?
What is the primary function of myofibroblasts in the kidney?
What is the name of the region surrounding the renal pelvis and calyces?
What is the name of the region surrounding the renal pelvis and calyces?
What is the term for the parallel rays extending from the medulla into the cortex?
What is the term for the parallel rays extending from the medulla into the cortex?
What is the function of the Bowman's capsule?
What is the function of the Bowman's capsule?
What is the term for the process of transporting substances from the tubular fluid back into the blood?
What is the term for the process of transporting substances from the tubular fluid back into the blood?
What is the function of the ascending limb of the loop of Henle?
What is the function of the ascending limb of the loop of Henle?
What is the term for the functional units that filter blood and form urine?
What is the term for the functional units that filter blood and form urine?
What is the role of the distal convoluted tubule in the nephron?
What is the role of the distal convoluted tubule in the nephron?
What is the term for the process of transporting substances from the blood into the tubular fluid?
What is the term for the process of transporting substances from the blood into the tubular fluid?
What is the final segment of the nephron that receives filtrate from multiple nephrons?
What is the final segment of the nephron that receives filtrate from multiple nephrons?
What is the primary function of the renal corpuscle?
What is the primary function of the renal corpuscle?
What is the name of the epithelial capsule that surrounds the glomerulus?
What is the name of the epithelial capsule that surrounds the glomerulus?
What is the purpose of the mesangial cells in the glomerulus?
What is the purpose of the mesangial cells in the glomerulus?
What is the name of the capillary network that surrounds the proximal convoluted tubule?
What is the name of the capillary network that surrounds the proximal convoluted tubule?
What is the term for the space between the visceral and parietal layers of the glomerular capsule?
What is the term for the space between the visceral and parietal layers of the glomerular capsule?
What is the function of the podocytes in the glomerulus?
What is the function of the podocytes in the glomerulus?
What is the name of the arteries that branch from the renal arteries and enter the renal cortex?
What is the name of the arteries that branch from the renal arteries and enter the renal cortex?
What is the function of the slit diaphragms in the glomerulus?
What is the function of the slit diaphragms in the glomerulus?
What is the term for the network of capillary loops that surround the loops of Henle and collecting ducts?
What is the term for the network of capillary loops that surround the loops of Henle and collecting ducts?
What is the function of the proximal convoluted tubule cells?
What is the function of the proximal convoluted tubule cells?
What is the primary function of the cells lining the distal convoluted tubule?
What is the primary function of the cells lining the distal convoluted tubule?
Which layer of the urinary bladder wall allows for its expansion?
Which layer of the urinary bladder wall allows for its expansion?
What type of epithelium lines the ureters?
What type of epithelium lines the ureters?
What is the function of the umbrella cells in the urothelium?
What is the function of the umbrella cells in the urothelium?
What type of muscle layer is found in the muscularis of the ureters?
What type of muscle layer is found in the muscularis of the ureters?
What is the function of the urethra in males?
What is the function of the urethra in males?
What is the term for the rhythmic contractions of the ureter walls that move urine efficiently?
What is the term for the rhythmic contractions of the ureter walls that move urine efficiently?
What is the main function of the urinary bladder?
What is the main function of the urinary bladder?
What type of epithelium lines the thin ascending limb of the loop of Henle?
What type of epithelium lines the thin ascending limb of the loop of Henle?
What is the function of the transitional epithelium in the urinary system?
What is the function of the transitional epithelium in the urinary system?
What is the primary mechanism by which the kidneys regulate the acid-base balance?
What is the primary mechanism by which the kidneys regulate the acid-base balance?
Which of the following processes is NOT a primary function of the kidneys?
Which of the following processes is NOT a primary function of the kidneys?
What is the name of the enzyme secreted by the kidneys that helps increase blood pressure?
What is the name of the enzyme secreted by the kidneys that helps increase blood pressure?
During periods of fasting or starvation, what process do the kidneys perform to help maintain blood sugar levels?
During periods of fasting or starvation, what process do the kidneys perform to help maintain blood sugar levels?
What is the term for the process by which the kidneys filter out waste products and excess water and electrolytes from the blood?
What is the term for the process by which the kidneys filter out waste products and excess water and electrolytes from the blood?
What is the primary function of the kidneys in maintaining blood pressure?
What is the primary function of the kidneys in maintaining blood pressure?
What is the term for the process by which the kidneys convert vitamin D to its active form?
What is the term for the process by which the kidneys convert vitamin D to its active form?
What is the structure through which nerves enter the kidney and the ureter exits?
What is the structure through which nerves enter the kidney and the ureter exits?
What is the main function of the fibroblasts in the kidney?
What is the main function of the fibroblasts in the kidney?
Which of the following structures is responsible for the initial filtration of blood?
Which of the following structures is responsible for the initial filtration of blood?
What is the main function of the renal medulla?
What is the main function of the renal medulla?
What is the term for the process of reabsorbing essential substances from the tubular fluid back into the blood?
What is the term for the process of reabsorbing essential substances from the tubular fluid back into the blood?
Which of the following hormones regulates sodium reabsorption in the distal convoluted tubule?
Which of the following hormones regulates sodium reabsorption in the distal convoluted tubule?
What is the primary function of the interlobar arteries?
What is the primary function of the interlobar arteries?
What is the function of the visceral layer of the glomerular capsule?
What is the function of the visceral layer of the glomerular capsule?
What is the term for the functional units that collect and transport urine from the kidneys to the urinary bladder?
What is the term for the functional units that collect and transport urine from the kidneys to the urinary bladder?
What is the function of the mesangial cells?
What is the function of the mesangial cells?
What is the primary function of the renal cortex?
What is the primary function of the renal cortex?
Which of the following structures separates the renal pyramids?
Which of the following structures separates the renal pyramids?
What is the function of the peritubular capillaries?
What is the function of the peritubular capillaries?
What is the function of the podocytes?
What is the function of the podocytes?
What is the term for the process of transporting substances from the blood into the tubular fluid?
What is the term for the process of transporting substances from the blood into the tubular fluid?
Which of the following structures is responsible for the final concentration of urine?
Which of the following structures is responsible for the final concentration of urine?
What is the function of the arcuate arteries?
What is the function of the arcuate arteries?
What is the function of the efferent arterioles?
What is the function of the efferent arterioles?
What is the function of the glomerular capsule?
What is the function of the glomerular capsule?
What is the function of the renal corpuscle?
What is the function of the renal corpuscle?
What is the function of the interlobar arteries?
What is the function of the interlobar arteries?
What is the primary function of the thin descending limb and thin ascending limb in the loop of Henle?
What is the primary function of the thin descending limb and thin ascending limb in the loop of Henle?
What is the characteristic of the epithelial cells in the thick ascending limb of the loop of Henle?
What is the characteristic of the epithelial cells in the thick ascending limb of the loop of Henle?
What is the primary function of the distal convoluted tubule?
What is the primary function of the distal convoluted tubule?
What is the characteristic of the muscularis layer in the ureters?
What is the characteristic of the muscularis layer in the ureters?
What is the primary function of the urothelium?
What is the primary function of the urothelium?
What is the characteristic of the detrusor muscle in the urinary bladder?
What is the characteristic of the detrusor muscle in the urinary bladder?
What is the function of the umbrella cells in the urothelium?
What is the function of the umbrella cells in the urothelium?
What is the characteristic of the epithelial cells in the urethra?
What is the characteristic of the epithelial cells in the urethra?
What is the primary function of the urinary bladder?
What is the primary function of the urinary bladder?
What is the mechanism by which the ureters transport urine from the kidneys to the bladder?
What is the mechanism by which the ureters transport urine from the kidneys to the bladder?
Flashcards are hidden until you start studying
Study Notes
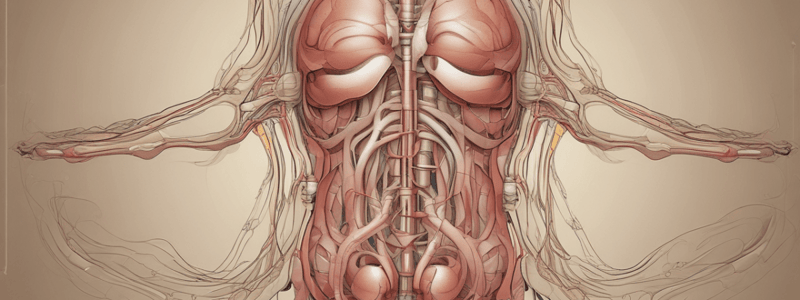
The Urinary System
- Consists of: 2 kidneys, 2 ureters, bladder, and urethra
- Primary role: Ensure optimal blood properties, regulate water and electrolyte balance, and excrete metabolic wastes and bioactive substances
Functions of the Urinary System
- Regulate water and electrolyte balance
- Excrete metabolic wastes, excess water, and electrolytes in urine
- Excrete bioactive substances, including drugs
- Secretion of renin, erythropoietin, and vitamin D
- Maintain pH levels and regulate blood pressure
Kidneys
- Covered by a thin fibrous layer, with an outer layer of fibroblasts and collagen fibers, and an inner layer of myofibroblasts
- Hilum: where nerves enter and ureter exits
- Renal pelvis: divides into 2-3 major calyces, which then turn into minor calyces
- Renal cortex: outer darker region containing renal corpuscles and tubules
- Renal medulla: inner region consisting of aligned linear tubules and ducts
- Renal pyramids: 8-15, with bases meeting at the cortex by the corticomedullary junction
Nephron
- Functional unit that filters blood and forms urine
- Consists of a renal corpuscle and a long renal tubule
- Renal corpuscle: glomerulus and Bowman's capsule
- Glomerulus: a tuft of capillaries where blood filtration begins
- Bowman's capsule: a double-walled capsule that surrounds the glomerulus and collects the filtrate
Renal Tubule
- Divided into several segments, each with specific functions in processing the filtrate
- Proximal convoluted tubule (PCT): reabsorbs a majority of the filtrate, including water, ions, and nutrients
- Loop of Henle: a U-shaped structure that extends into the medulla
- Distal convoluted tubule (DCT): continues to reabsorb ions and water, under the influence of hormones
- Collecting duct: the final segment that receives filtrate from multiple nephrons
Nephron Functions
- Filtration: occurs in the renal corpuscle, where blood pressure forces water and small solutes through the glomerular capillary walls
- Tubular reabsorption: substances are transported from the tubular fluid back into the blood
- Tubular secretion: substances are transported from the blood into the tubular fluid
Blood Flow in the Kidneys
- Renal arteries: transport oxygenated blood from the heart and aorta to the kidneys
- Renal veins: transport filtered deoxygenated blood from the kidneys to the heart
- Interlobular arteries: radiate from the arcuate arteries, extending deep into the cortex
- Afferent arterioles: lead into the glomerulus, and efferent arterioles exit from the glomerulus
Renal Corpuscle
- Contains a tuft of capillaries called glomerulus, surrounded by a epithelial capsule called the glomerular capsule
- Glomerular capsule: has a visceral layer and a parietal layer, with a capsular space between them
- Podocytes: stellate epithelium that creates the filtration apparatus of the kidney
- Slit pores: regulate the passage of substances during filtration
Proximal Convoluted Tubule (PCT)
- Cells are highly specialized for reabsorption and secretion
- Structure: dense brush border, abundant mitochondria, and extensive membrane invaginations
- Function: reabsorbs a majority of the filtrate, including water, ions, and nutrients
Loop of Henle
- Located in the medulla
- Thin descending limb and thin ascending limb: simple squamous epithelium and organelles
- Thick ascending limb: simple cuboidal epithelium and many mitochondria
Distal Convoluted Tubule (DCT)
- Lined with simple cuboidal cells that are smaller and flatter compared to the ones in the PCT
- Function: performs regulated reabsorption while influenced by the hormone aldosterone
Ureters
- Muscular tubes that transport urine from the renal pelvis to the urinary bladder
- Structure: mucosa, muscularis, and adventitia
- Function: move urine towards the bladder via peristaltic contractions and prevent backflow into the kidneys
Urinary Bladder
- Structure: mucosa, muscularis, and adventitia
- Function: stores urine and expels it during micturition
Urothelium (Transitional Epithelium)
- Found in the renal pelvis, ureters, bladder, and parts of the urethra
- Structure: basal cells, intermediate cells, and umbrella cells
- Function: protects underlying tissues from the toxic effects of urine and allows the bladder to stretch and contract
Urethra
- Structure: varies in males and females, but includes a prostatic urethra, membranous urethra, and spongy urethra
- Function: conducts urine from the bladder to the exterior, and in males, serves as a conduit for semen during ejaculation
The Urinary System
- Consists of: 2 kidneys, 2 ureters, bladder, and urethra
- Primary role: Ensure optimal blood properties, regulate water and electrolyte balance, and excrete metabolic wastes and bioactive substances
Functions of the Urinary System
- Regulate water and electrolyte balance
- Excrete metabolic wastes, excess water, and electrolytes in urine
- Excrete bioactive substances, including drugs
- Secretion of renin, erythropoietin, and vitamin D
- Maintain pH levels and regulate blood pressure
Kidneys
- Covered by a thin fibrous layer, with an outer layer of fibroblasts and collagen fibers, and an inner layer of myofibroblasts
- Hilum: where nerves enter and ureter exits
- Renal pelvis: divides into 2-3 major calyces, which then turn into minor calyces
- Renal cortex: outer darker region containing renal corpuscles and tubules
- Renal medulla: inner region consisting of aligned linear tubules and ducts
- Renal pyramids: 8-15, with bases meeting at the cortex by the corticomedullary junction
Nephron
- Functional unit that filters blood and forms urine
- Consists of a renal corpuscle and a long renal tubule
- Renal corpuscle: glomerulus and Bowman's capsule
- Glomerulus: a tuft of capillaries where blood filtration begins
- Bowman's capsule: a double-walled capsule that surrounds the glomerulus and collects the filtrate
Renal Tubule
- Divided into several segments, each with specific functions in processing the filtrate
- Proximal convoluted tubule (PCT): reabsorbs a majority of the filtrate, including water, ions, and nutrients
- Loop of Henle: a U-shaped structure that extends into the medulla
- Distal convoluted tubule (DCT): continues to reabsorb ions and water, under the influence of hormones
- Collecting duct: the final segment that receives filtrate from multiple nephrons
Nephron Functions
- Filtration: occurs in the renal corpuscle, where blood pressure forces water and small solutes through the glomerular capillary walls
- Tubular reabsorption: substances are transported from the tubular fluid back into the blood
- Tubular secretion: substances are transported from the blood into the tubular fluid
Blood Flow in the Kidneys
- Renal arteries: transport oxygenated blood from the heart and aorta to the kidneys
- Renal veins: transport filtered deoxygenated blood from the kidneys to the heart
- Interlobular arteries: radiate from the arcuate arteries, extending deep into the cortex
- Afferent arterioles: lead into the glomerulus, and efferent arterioles exit from the glomerulus
Renal Corpuscle
- Contains a tuft of capillaries called glomerulus, surrounded by a epithelial capsule called the glomerular capsule
- Glomerular capsule: has a visceral layer and a parietal layer, with a capsular space between them
- Podocytes: stellate epithelium that creates the filtration apparatus of the kidney
- Slit pores: regulate the passage of substances during filtration
Proximal Convoluted Tubule (PCT)
- Cells are highly specialized for reabsorption and secretion
- Structure: dense brush border, abundant mitochondria, and extensive membrane invaginations
- Function: reabsorbs a majority of the filtrate, including water, ions, and nutrients
Loop of Henle
- Located in the medulla
- Thin descending limb and thin ascending limb: simple squamous epithelium and organelles
- Thick ascending limb: simple cuboidal epithelium and many mitochondria
Distal Convoluted Tubule (DCT)
- Lined with simple cuboidal cells that are smaller and flatter compared to the ones in the PCT
- Function: performs regulated reabsorption while influenced by the hormone aldosterone
Ureters
- Muscular tubes that transport urine from the renal pelvis to the urinary bladder
- Structure: mucosa, muscularis, and adventitia
- Function: move urine towards the bladder via peristaltic contractions and prevent backflow into the kidneys
Urinary Bladder
- Structure: mucosa, muscularis, and adventitia
- Function: stores urine and expels it during micturition
Urothelium (Transitional Epithelium)
- Found in the renal pelvis, ureters, bladder, and parts of the urethra
- Structure: basal cells, intermediate cells, and umbrella cells
- Function: protects underlying tissues from the toxic effects of urine and allows the bladder to stretch and contract
Urethra
- Structure: varies in males and females, but includes a prostatic urethra, membranous urethra, and spongy urethra
- Function: conducts urine from the bladder to the exterior, and in males, serves as a conduit for semen during ejaculation
The Urinary System
- Consists of: 2 kidneys, 2 ureters, bladder, and urethra
- Primary role: Ensure optimal blood properties, regulate water and electrolyte balance, and excrete metabolic wastes and bioactive substances
Functions of the Urinary System
- Regulate water and electrolyte balance
- Excrete metabolic wastes, excess water, and electrolytes in urine
- Excrete bioactive substances, including drugs
- Secretion of renin, erythropoietin, and vitamin D
- Maintain pH levels and regulate blood pressure
Kidneys
- Covered by a thin fibrous layer, with an outer layer of fibroblasts and collagen fibers, and an inner layer of myofibroblasts
- Hilum: where nerves enter and ureter exits
- Renal pelvis: divides into 2-3 major calyces, which then turn into minor calyces
- Renal cortex: outer darker region containing renal corpuscles and tubules
- Renal medulla: inner region consisting of aligned linear tubules and ducts
- Renal pyramids: 8-15, with bases meeting at the cortex by the corticomedullary junction
Nephron
- Functional unit that filters blood and forms urine
- Consists of a renal corpuscle and a long renal tubule
- Renal corpuscle: glomerulus and Bowman's capsule
- Glomerulus: a tuft of capillaries where blood filtration begins
- Bowman's capsule: a double-walled capsule that surrounds the glomerulus and collects the filtrate
Renal Tubule
- Divided into several segments, each with specific functions in processing the filtrate
- Proximal convoluted tubule (PCT): reabsorbs a majority of the filtrate, including water, ions, and nutrients
- Loop of Henle: a U-shaped structure that extends into the medulla
- Distal convoluted tubule (DCT): continues to reabsorb ions and water, under the influence of hormones
- Collecting duct: the final segment that receives filtrate from multiple nephrons
Nephron Functions
- Filtration: occurs in the renal corpuscle, where blood pressure forces water and small solutes through the glomerular capillary walls
- Tubular reabsorption: substances are transported from the tubular fluid back into the blood
- Tubular secretion: substances are transported from the blood into the tubular fluid
Blood Flow in the Kidneys
- Renal arteries: transport oxygenated blood from the heart and aorta to the kidneys
- Renal veins: transport filtered deoxygenated blood from the kidneys to the heart
- Interlobular arteries: radiate from the arcuate arteries, extending deep into the cortex
- Afferent arterioles: lead into the glomerulus, and efferent arterioles exit from the glomerulus
Renal Corpuscle
- Contains a tuft of capillaries called glomerulus, surrounded by a epithelial capsule called the glomerular capsule
- Glomerular capsule: has a visceral layer and a parietal layer, with a capsular space between them
- Podocytes: stellate epithelium that creates the filtration apparatus of the kidney
- Slit pores: regulate the passage of substances during filtration
Proximal Convoluted Tubule (PCT)
- Cells are highly specialized for reabsorption and secretion
- Structure: dense brush border, abundant mitochondria, and extensive membrane invaginations
- Function: reabsorbs a majority of the filtrate, including water, ions, and nutrients
Loop of Henle
- Located in the medulla
- Thin descending limb and thin ascending limb: simple squamous epithelium and organelles
- Thick ascending limb: simple cuboidal epithelium and many mitochondria
Distal Convoluted Tubule (DCT)
- Lined with simple cuboidal cells that are smaller and flatter compared to the ones in the PCT
- Function: performs regulated reabsorption while influenced by the hormone aldosterone
Ureters
- Muscular tubes that transport urine from the renal pelvis to the urinary bladder
- Structure: mucosa, muscularis, and adventitia
- Function: move urine towards the bladder via peristaltic contractions and prevent backflow into the kidneys
Urinary Bladder
- Structure: mucosa, muscularis, and adventitia
- Function: stores urine and expels it during micturition
Urothelium (Transitional Epithelium)
- Found in the renal pelvis, ureters, bladder, and parts of the urethra
- Structure: basal cells, intermediate cells, and umbrella cells
- Function: protects underlying tissues from the toxic effects of urine and allows the bladder to stretch and contract
Urethra
- Structure: varies in males and females, but includes a prostatic urethra, membranous urethra, and spongy urethra
- Function: conducts urine from the bladder to the exterior, and in males, serves as a conduit for semen during ejaculation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.