Podcast
Questions and Answers
What is the role of Hydrochloric Acid (HCl) in the stomach?
What is the role of Hydrochloric Acid (HCl) in the stomach?
- Killing bacteria (correct)
- Emulsifying fats
- Neutralizing chyme
- Breaking down proteins
What do Chief Cells in the stomach secrete?
What do Chief Cells in the stomach secrete?
Pepsinogen
Salivary enzymes start breaking down food in the mouth.
Salivary enzymes start breaking down food in the mouth.
True (A)
The final site for major chemical digestion and nutrient absorption in the digestive system is the ____________.
The final site for major chemical digestion and nutrient absorption in the digestive system is the ____________.
Match the following enzymes with their respective nutrient types:
Match the following enzymes with their respective nutrient types:
What are the main functions of the urinary system? (Select all that apply)
What are the main functions of the urinary system? (Select all that apply)
Define osmolarity.
Define osmolarity.
Match the anatomical structures with their functions:
Match the anatomical structures with their functions:
Filtration in the kidney occurs when hydrostatic pressure is less than osmotic pressure.
Filtration in the kidney occurs when hydrostatic pressure is less than osmotic pressure.
_______ is responsible for creating an osmolarity gradient in the interstitial fluid.
_______ is responsible for creating an osmolarity gradient in the interstitial fluid.
Flashcards are hidden until you start studying
Study Notes
Here are the study notes for the provided text:
- Urinary System and Filtration*
Functions of the Urinary System
- Maintains blood osmolarity
- Regulates blood volume and pressure
- Removes waste products
Osmolarity
- Definition: Number of particles per liter of solution
- Blood osmolarity: ~300 milliosmoles
- Importance: Keeps dissolved particles in blood constant
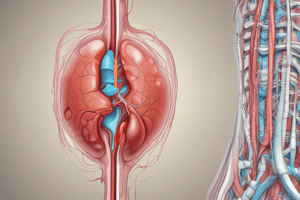
Kidneys: Role and Structure
Primary Functions
- Filtration of blood
- Reabsorption of nutrients
- Secretion of toxins
- Regulation of water balance
Anatomical Structures
- Nephron: Functional unit of the kidney
- Glomerulus: Bundle of capillaries for filtration
- Bowman's Capsule: Captures filtrate from glomerulus
- Renal Artery: Supplies blood to kidneys
- Ureter: Transports urine to bladder
Filtration Process
- Initial Filtration: Blood enters glomerulus, filtrate includes water, small molecules, waste products
- Filtration Mechanics: Driven by hydrostatic pressure, counterbalanced by colloid osmotic pressure
- Filtration vs. Absorption: Filtration occurs when hydrostatic pressure > osmotic pressure, absorption occurs when osmotic pressure > hydrostatic pressure
Detailed Kidney Filtration Steps
- Filtration in the Glomerulus: Blood pressure forces water and small molecules through capillary walls
- Reabsorption: Filtrate passes through nephron, nutrients and water reabsorbed into blood
- Secretion: Additional waste products actively transported into filtrate
- Excretion: Filtrate becomes urine, transported to bladder via ureter
Factors Influencing Filtration
- Hydrostatic Pressure: Blood pressure within glomerulus, favors filtration
- Colloid Osmotic Pressure: Pressure exerted by proteins in blood, opposes filtration
- Net Filtration Pressure: Difference between hydrostatic and osmotic pressures, results in filtration
Capillary Dynamics in Filtration
- Upstream End: Higher hydrostatic pressure, filtration favored
- Downstream End: Lower hydrostatic pressure, absorption favored
- Balance Maintained by Lymphatic System: Prevents buildup of excess fluid, returns filtered fluid to circulatory system
- 8.2: The Nephron*
Mind Map: Nephron and Urine Concentration
Central Topic: Nephron - Functional Unit of the Kidney
- Overview of the Kidney: Sophisticated exchange organ, maintains homeostasis of blood osmolarity (~300 milliosmoles)
Processes in the Nephron
- Filtration
- Reabsorption: Retaining essential nutrients
- Secretion: Eliminating toxins from the body
Regulation of Urine Concentration
- Importance of Osmolarity: Urine osmolarity must vary to maintain blood osmolarity, control of water determines urine concentration
Nephron Structure
- Tubule Properties: Membrane properties vary along its length
- Key Sections:
- Bowman's Capsule
- Proximal Tubule
- Loop of Henle
- Distal Tubule
- Collecting Duct
Mechanisms of Water Control
- Water Movement: No water pumps; water moves by osmosis
- Aquaporins: Water channels facilitating water movement across membranes
- Permeable vs. Impermeable Membranes:
- Permeable: Water leaves filtrate, increasing osmolarity
- Impermeable: Water stays in filtrate, low osmolarity
Collecting Duct Function
- High Water Permeability
- Osmolarity Gradient: Increases from cortex to medulla
- Variable Osmolarity: Controlled by aquaporins and interstitial fluid osmolarity
Loop of Henle
- Descending Limb: High water permeability, water leaves, concentrating filtrate
- Ascending Limb: Low water permeability, ions (NaCl) removed
Osmolarity Control
- Gradient Creation: Loop of Henle creates osmolarity gradient in interstitial fluid
- Minimum Osmolarity: Set by distal tubule, influencing final urine concentration
Overall Urine Formation
- Filtration at Bowman's Capsule
- Reabsorption and Secretion
- Osmolarity Adjustment: Loop of Henle and collecting duct
And so on...
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.