Podcast
Questions and Answers
Which structure connects the kidney to the bladder?
Which structure connects the kidney to the bladder?
- Urethra
- Nephron
- Renal artery
- Ureter (correct)
What is the functional unit of the kidney responsible for urine formation?
What is the functional unit of the kidney responsible for urine formation?
- Ureter
- Urethra
- Nephron (correct)
- Bladder
Which hormone causes the kidneys to reabsorb sodium?
Which hormone causes the kidneys to reabsorb sodium?
- Renin
- Antidiuretic hormone (ADH)
- Aldosterone (correct)
- Erythropoietin
What term describes decreased urine output of less than 50 mL in 24 hours?
What term describes decreased urine output of less than 50 mL in 24 hours?
What glycoprotein produced by the kidney stimulates red blood cell production?
What glycoprotein produced by the kidney stimulates red blood cell production?
What is the term for painful or difficult urination?
What is the term for painful or difficult urination?
What is the term for blood in the urine?
What is the term for blood in the urine?
What is the term for awakening at night to urinate?
What is the term for awakening at night to urinate?
What is the normal capacity of the adult bladder?
What is the normal capacity of the adult bladder?
Which system relaxes the bladder wall to allow filling?
Which system relaxes the bladder wall to allow filling?
What percentage of blood that flows into the glomerulus is filtered into the nephron?
What percentage of blood that flows into the glomerulus is filtered into the nephron?
Which hormone regulates water excretion from the kidneys?
Which hormone regulates water excretion from the kidneys?
What is the normal glomerular filtration rate (GFR)?
What is the normal glomerular filtration rate (GFR)?
Which of the following is a function of the kidneys?
Which of the following is a function of the kidneys?
What position is the right kidney in relation to the left kidney?
What position is the right kidney in relation to the left kidney?
Which of the following is a cause for concern in a urologic health history?
Which of the following is a cause for concern in a urologic health history?
What sound is typically produced when percussing the bladder?
What sound is typically produced when percussing the bladder?
What is the normal range of urine specific gravity?
What is the normal range of urine specific gravity?
Until what percentage is the GFR reduced before renal function tests become abnormal?
Until what percentage is the GFR reduced before renal function tests become abnormal?
What is the normal range for BUN (blood urea nitrogen)?
What is the normal range for BUN (blood urea nitrogen)?
What does a KUB X-ray visualize?
What does a KUB X-ray visualize?
What is the primary use of a cystoscopic examination?
What is the primary use of a cystoscopic examination?
What is the second most common type of infection?
What is the second most common type of infection?
What term describes bacteria in the urine?
What term describes bacteria in the urine?
Which of the following is a symptom of a lower UTI?
Which of the following is a symptom of a lower UTI?
What colony count indicates a UTI in a urine culture?
What colony count indicates a UTI in a urine culture?
What finding is seen in all UTI cases?
What finding is seen in all UTI cases?
What is the most common bacteria in uncomplicated UTIs?
What is the most common bacteria in uncomplicated UTIs?
What is a common adjunctive treatment for recurrent UTIs?
What is a common adjunctive treatment for recurrent UTIs?
What should patients avoid to prevent recurrent UTIs?
What should patients avoid to prevent recurrent UTIs?
What is a key symptom of acute pyelonephritis?
What is a key symptom of acute pyelonephritis?
What is a common substance found in kidney stones?
What is a common substance found in kidney stones?
What is the lithotripsy used for?
What is the lithotripsy used for?
What dietary instruction should be given to prevent renal calculi?
What dietary instruction should be given to prevent renal calculi?
What is the primary diagnostic tool for polycystic kidney disease (PKD)?
What is the primary diagnostic tool for polycystic kidney disease (PKD)?
What cause Hydronephrosis?
What cause Hydronephrosis?
Flashcards
Aldosterone
Aldosterone
Hormone from adrenal cortex; causes kidneys to reabsorb sodium.
Antidiuretic Hormone (ADH)
Antidiuretic Hormone (ADH)
Hormone secreted by the posterior pituitary gland to increase water reabsorption in the kidneys.
Anuria
Anuria
Decreased urine output of less than 50 mL in 24 hours.
Bacteriuria
Bacteriuria
Signup and view all the flashcards
Creatinine
Creatinine
Signup and view all the flashcards
Diuresis
Diuresis
Signup and view all the flashcards
Dysuria
Dysuria
Signup and view all the flashcards
Erythropoietin
Erythropoietin
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Glomerulus
Glomerulus
Signup and view all the flashcards
Glycosuria
Glycosuria
Signup and view all the flashcards
Hematuria
Hematuria
Signup and view all the flashcards
Micturition
Micturition
Signup and view all the flashcards
Nephrons
Nephrons
Signup and view all the flashcards
Nocturia
Nocturia
Signup and view all the flashcards
Oliguria
Oliguria
Signup and view all the flashcards
Proteinuria
Proteinuria
Signup and view all the flashcards
Pyuria
Pyuria
Signup and view all the flashcards
Renal Clearance
Renal Clearance
Signup and view all the flashcards
Specific Gravity
Specific Gravity
Signup and view all the flashcards
Urea Nitrogen
Urea Nitrogen
Signup and view all the flashcards
Urinary Frequency
Urinary Frequency
Signup and view all the flashcards
Ureters
Ureters
Signup and view all the flashcards
Urinary Bladder
Urinary Bladder
Signup and view all the flashcards
Urethra
Urethra
Signup and view all the flashcards
Urine Formation Steps
Urine Formation Steps
Signup and view all the flashcards
Urologic Health History
Urologic Health History
Signup and view all the flashcards
Costovertebral Angle
Costovertebral Angle
Signup and view all the flashcards
Kidney, Ureter, and Bladder (KUB) X-Ray
Kidney, Ureter, and Bladder (KUB) X-Ray
Signup and view all the flashcards
Urine Culture
Urine Culture
Signup and view all the flashcards
Urine Specific Gravity
Urine Specific Gravity
Signup and view all the flashcards
Creatinine
Creatinine
Signup and view all the flashcards
Blood Urea Nitrogen (BUN)
Blood Urea Nitrogen (BUN)
Signup and view all the flashcards
Urinary Tract Infections (UTIs)
Urinary Tract Infections (UTIs)
Signup and view all the flashcards
Lower UTIs
Lower UTIs
Signup and view all the flashcards
Upper UTIs
Upper UTIs
Signup and view all the flashcards
Microscopic Hematuria (UTI)
Microscopic Hematuria (UTI)
Signup and view all the flashcards
Pyuria (UTI)
Pyuria (UTI)
Signup and view all the flashcards
Urolithiasis
Urolithiasis
Signup and view all the flashcards
Nephrosclerosis
Nephrosclerosis
Signup and view all the flashcards
Study Notes
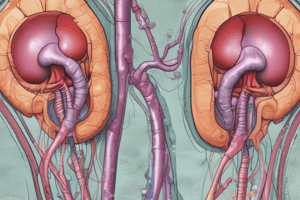
Urinary System Structure and Function
- The kidneys, ureters, bladder, and urethra make up the renal and urinary systems.
- The kidneys create urine, which travels via other structures before being eliminated.
- Kidneys are brownish-red, bean-shaped organs located retroperitoneally, from the T12 to L3 vertebrae.
- The right kidney sits slightly lower than the left due to the liver's position.
- Nephrons, located in the renal parenchyma, are the functional units of the kidneys responsible for urine formation.
- Each kidney around has one million nephrons.
- Ureters are fibromuscular tubes, 24 to 30 cm long, connecting each kidney to the bladder.
- They enter the bladder at an oblique angle to prevent backflow.
- Peristalsis propels urine through the ureters to the bladder.
- The urinary bladder is a distensible muscular sac behind the pubic bone.
- Adult bladder capacity is typically 400 to 500 mL, with the ability to expand further.
- It features a central hollow area, the vesicle, with two ureter inlets and one urethra outlet.
- Internal and external sphincters between the bladder and urethra maintain continence.
- The sympathetic system relaxes the bladder wall for filling and contracts the inner sphincter to retain urine.
- The parasympathetic system contracts the bladder wall and relaxes the inner sphincter to allow urine escape when relieving bladder.
- The urethra stems from the bladder's base, around 3.7cm long in females and 20 cm long in males.
Physiology of the Kidney and Urinary Systems
- Critical for maintaining homeostasis through urine formation, water and electrolyte regulation, acid-base balance, and blood pressure control.
- Urine formation occurs in three steps: glomerular filtration, tubular reabsorption, and tubular secretion.
- Blood flows into the glomerulus where 20% of it is filtered into the nephron forming filtrate (water and small molecules).
- Essential substances like sodium, glucose, and amino acids are reabsorbed into the blood.
- Waste products like potassium and urea are secreted into the filtrate.
- ADH, or vasopressin, regulates water excretion by adjusting kidney reabsorption relative to blood osmolality.
- Secreted by the posterior pituitary, ADH prompts the kidneys to reabsorb water.
- The glomerular filtration rate (GFR) is the plasma volume filtered at the glomerulus into the kidney tubules each minute, with a normal rate of 120 mL/min.
- Approximately 180 liters of blood are filtered daily, with only 1% excreted as urine.
- Urine formation is the primary function of the nephron, the kidney's structural and functional unit.
Functions of the Kidney
- Blood pressure control
- Water balance maintenance
- Waste product excretion
- Electrolyte regulation
- Acid-base balance management
- Red blood cell production regulation
- Renal clearance
- Prostaglandin secretion
- Vitamin D synthesis (active form)
- Urine formation
Assessment of the Kidney and Urinary Systems - Health History
- Requires excellent communication skills due to patient sensitivity about discussing genitourinary issues.
- Inquire about the chief concern, onset, and impact on the patient’s life.
- Note the location, character, duration of dysuria, precipitating and relieving factors, and its relationship to voiding.
- Ask about the history of UTIs, including treatments or hospitalizations.
- Note any fever or chills.
- Document previous renal or urinary tests, surgeries, and catheter use.
- Ask about hesitancy, straining, or frequency of urination.
- Note any urinary incontinence (stress, urge, overflow, or functional).
- Check for hematuria or changes in urine color/volume.
- Ask about nocturia onset.
- Check for renal calculi or passing stones/gravel in urine.
- For female patients, ask about deliveries, vaginal issues, and contraceptive practices.
- Note any history of anuria or other kidney problems.
- Assess for genital lesions or STIs.
- Ask about tobacco, alcohol, or recreational drug use.
- List all prescription and over-the-counter medications.
Physical Assessment
- A comprehensive head-to-toe assessment is essential.
- Assess abdomen, suprapubic region, genitalia, lower back, and lower extremities.
- Palpation may reveal kidney enlargement.
- The right kidney is often easier to palpate due to its lower position.
- Palpation may be difficult in obese patients.
- Renal dysfunction can cause tenderness over the costovertebral angle.
Assessment Techniques
- Inspection: Examine the abdomen and urethral meatus.
- Auscultation: Listen to renal arteries.
- Percussion: Check for kidney tenderness.
- Palpation: detect masses, lumps, or tenderness.
- Percussion of the bladder helps to detect differences in sound towards the bladder's base, normally tympanic.
Diagnostic Evaluation - Urinalysis and Urine Culture
- Urinalysis offers important insights into kidney function and diabetes diagnosis.
- Urine culture detects bacteria strains, their concentration, identifies and suggests antimicrobial therapy options based on local resistance patterns.
Urine Examination
- Includes assessing urine color, clarity, and odor.
- Measures urine pH and specific gravity (normal range: 1.005 to 1.025).
- Tests for protein, glucose, and ketone bodies (proteinuria, glycosuria, and ketonuria).
- Microscopic examination of urine sediment detects hematuria, pyuria, casts, crystals, and bacteriuria.
Renal Function Tests
- Results may be normal until GFR is reduced to less than 50%.
- Common tests: renal concentration, creatinine clearance, serum creatinine, and BUN.
- Specific Gravity reflects kidney concentration ability, with a normal range of 1.005-1.025.
- Creatinine, a product of muscular energy metabolism, has normal ranges: 0.6-1.2 mg/dL in males and 0.4-1.0 mg/dL in females.
- BUN (blood urea nitrogen) normal range 8-20mg/dl, indicates renal function and protein metabolism.
Diagnostic Imaging
- KUB X-RAY visualizes size, shape, position, and kidney stones.
- General and bladder Ultrasonography are performed.
- Computed Tomography and Magnetic Resonance Imaging are non-invasive, providing cross-sectional views of the kidney and urinary tract.
- Nuclear Scans use radioisotope injection; they provide details on kidney perfusion, function, and GFR.
- Renal Angiography provides an image of the renal arteries.
- Urologic Endoscopic Procedures use a cystoscope via the urethra or a percutaneous incision.
- Cystoscopic examination directly visualizes the urethra and bladder.
- BIOPSY of the bladder and kidney determines renal disease, rarely done with one kidney.
Urinary Tract Infections (UTIs) Prevalence
- UTIs are the second most common infection, accounting for 25% of all infections.
- 8.1 million women are diagnosed with UTIs annually in the United States.
- UTIs lead to over 100,000 hospital admissions each year.
- Hospital-acquired infections often include UTIs, with most being catheter-associated (CAUTI) in patients with indwelling catheters for over 2 days.
Types and Pathophysiology of UTIs
- Lower UTIs affect the bladder and structures below, including bacterial cystitis, prostatitis, and urethritis.
- Upper UTIs involve the kidneys and ureters, such as acute pyelonephritis and chronic pyelonephritis.
- The bladder stays sterile due to the urethra's physical barrier, urine flow, ureterovesical junction integrity, antibacterial enzymes, antibodies, and mucosal cell antiadherent effects.
- Dysfunction in these mechanisms increases the risk of lower UTIs.
- Bacteria must access the bladder, attach to the epithelium to avoid being washed out, evade defenses, and initiate inflammation for infection to occur.
- Many UTIs result from fecal organisms ascending from the perineum to the urethra and bladder.
- Bacteriuria describes the presence of bacteria in the urine.
Clinical Manifestations of UTIs
- Lower UTI (Bladder Infection): Burning sensation, frequency, urgency, nocturia, incontinence, suprapubic/pelvic pain, possible hematuria, and back pain.
- Upper UTI (Kidney Infection): Symptoms vary from mild to severe and may include fever, chills, and flank pain.
- In Older Adults: Symptoms may be less common or more subtle.
- Complicated UTIs: Range from asymptomatic bacteriuria to severe sepsis. Often caused by a broader range of organisms, harder to treat, and more likely to recur.
- Catheter-Associated UTIs (CAUTIs): Often asymptomatic, but should be evaluated for urosepsis.
Factors That Increase UTI Risk in Older Adults
- They include cognitive impairment, frequent antimicrobial use, multiple chronic conditions, immunocompromised status, immobility, low fluid intake, obstructed urine flow, and poor hygiene.
Assessment and Diagnostic Findings for UTIs
- Urine Culture: Confirms UTI, identifies organism; >100,000 CFU/mL indicates infection.
- Additional Tests: Urine dipsticks, WBC testing, CT scans, and ultrasounds for obstruction, abscesses, or tumors.
Medical Management of UTIs
- Acute Therapy: Antibiotics vary depending on bacteria; shorter courses (3–7 days) for uncomplicated UTIs in women.
- Complicated UTIs: Require longer treatment, hospitalization, and possible IV antibiotics.
- Patient Education: Complete antibiotics, hydration; further evaluation for recurrent UTIs.
- Urine cultures document UTI and identify organisms; >100,000 CFU/mL indicates infection.
- Recommended for children, men, recently hospitalized, diabetics, persistent symptoms, frequent UTIs, pregnant women, and the immunocompromised.
- Cellular Studies: Microscopic Hematuria (50% of acute UTI cases) and Pyuria (all UTI cases) are seen.
- Other Studies: Dipstick Tests detect WBCs and nitrites. Sexually Transmitted Infection Tests rule out infections causing urethritis. Imaging detects pyelonephritis, abscesses, obstructions, tumors, and cysts.
- Pharmacologic Therapy: Antibacterial agents targeting E. coli or other fecal flora is preferred.
- Acute Treatment: Regimens include single-dose, short-course (3-day), or 7-day antibiotics; complete full course.
- Complicated UTIs: Require longer treatment and possible hospitalization with IV antibiotics. Men should be evaluated for prostatitis.
- Long-Term Pharmacologic Therapy: Recurrences (20% of women), may need another short course (3-4 days) of full-dose antimicrobial therapy, followed by a regular bedtime dose.
- Adjunctive Treatment: Cranberry capsules significantly reduce recurrent UTIs but antibiotics are more effective, though with more severe side effects.
Nursing Process for UTIs
- Diagnosis: Acute pain due to urinary tract infection, lack of knowledge about predisposing factors, detection, prevention, and pharmacologic therapy.
- Planning and Goals: pain relief, improved knowledge of preventive measures, and absence of complications.
Nursing Interventions
- Providing antimicrobial therapy and antispasmodic agents for bladder irritability and pain.
- Provide analgesics and heat to the perineum for pain relief.
- Encourage liberal fluid intake and avoid urinary tract irritants.
- Encourage frequent voiding (every 2 to 3 hours).
- Early recognition and treatment are essential to prevent complications.
- Educate patients to recognize early symptoms.
- Monitor renal function periodically and check for strictures, obstructions, or stones.
Preventing Recurrent UTIs
- Hygiene: Shower instead of bathing, clean perineum front to back after bowel movements.
- Fluid Intake: Drink plenty of fluids, including cranberry juice, and avoid irritants like coffee, tea, colas, and alcohol.
- Voiding Habits: Void every 2 to 3 hours during the day, completely emptying the bladder; void immediately after intercourse.
- Interventions: Take medications as prescribed, consider long-term antimicrobial therapy, and notify the provider if symptoms persist.
Upper Urinary Tract Infections
- Include acute pyelonephritis, chronic pyelonephritis, interstitial nephritis, and kidney abscesses.
- Causes: Upward spread of bacteria from the bladder or via the bloodstream. Susceptibility increased by obstructions, bladder/prostate tumors, or systemic infections.
- Acute Pyelonephritis symptoms include: Fever, chills, leukocytosis, bacteriuria, pyuria, low back/flank pain, nausea/vomiting, malaise, painful urination, and costovertebral angle tenderness.
- Use Ultrasound, CT scan, IV pyelogram, urine culture, and radionuclide imaging for Assessment/Diagnostic Findings.
- Medical Management: Outpatient treatment for uncomplicated cases with a 2-week course of antibiotics. Follow-up cultures 2 weeks after therapy to ensure infection clearance. Hydration is key.
- Chronic Pyelonephritis Clinical Manifestations: Usually asymptomatic unless an acute exacerbation occurs; fatigue, headache, polyuria, excessive thirst, weight loss.
- Assessment/Diagnostic Findings: IV urogram, creatinine clearance, BUN, and creatinine levels.
- Long-term antimicrobial therapy prevents recurrence, monitors kidney function, and avoids nephrotoxic drugs.
- Hospitalized patients require careful fluid intake/output monitoring, often 3-4L/day.
- Monitor temperature, administer antipyretics and antibiotics as prescribed.
- Encourage hydration to alleviate symptoms and prevent dehydration.
Urolithiasis and Nephrolithiasis
- Urolithiasis refers to stones in the urinary tract; nephrolithiasis refers to stones in the kidneys.
- Most common in individuals aged 30-50; men are affected more frequently than women.
- Stone Composition: Common substances include calcium oxalate, calcium phosphate, and uric acid.
- Stones form due to high concentrations of substances like calcium and uric acid, with factors such as infection, urinary stasis, and immobility increasing the risk.
- Common Causes: Hypercalcemia, dehydration, urinary tract infections (UTIs), metabolic disorders, and certain medications.
- Stone Formation: Stones form when urinary concentrations of substances like calcium oxalate, calcium phosphate, and uric acid exceed their solubility, known as supersaturation.
- Locations: Stones can form anywhere in the urinary tract.
- Infection, urinary stasis, and immobility slow kidney drainage, altering calcium metabolism and increasing the likelihood of stone formation.
- Increased calcium levels in blood and urine promote stone formation, with calcium-based stones being the most common type.
- Increased calcium levels in blood and urine promote stone formation, with calcium-based stones being the most common type. Common causes: Hyperparathyroidism, renal tubular acidosis cancers (e.g., leukemia, multiple myeloma), dehydration, granulomatous diseases (e.g., sarcoidosis, tuberculosis), excessive vitamin D intake, excessive milk and alkali intake, myeloproliferative diseases (e.g., polycythemia vera), intestinal bypass surgery.
- Conditions Increasing Risk: Anatomical issues, metabolic factors, and medications.
- Obstruction Symptoms lead to Blockage of urine flow increases hydrostatic pressure, causing renal pelvis and ureter distension. It causes Renal Colic: Sudden severe pain with tenderness, nausea, vomiting, and sometimes diarrhea. Ureteral Obstruction: Sharp, colicky pain radiating to the thigh/genitalia, with possible hematuria. bladder Stones Results in Irritation symptoms like frequency, hematuria, or UTIs. Urinary Retention may occur if the stone obstructs the bladder neck
- Pain Relief: Opioids or NSAIDs to manage renal/ureteral colic.Hydration: Increased fluid intake to aid stone passage and dilute urinary crystalloids.
- Stone-Specific Treatment:Calcium Stones: Thiazide diuretics, diet adjustments. Uric Acid Stones: Low-purine diet, allopurinol. Cystine Stones: Alkalinize urine, increase fluid intake. Oxalate Stones: Fluid intake and oxalate reduction.
- Interventional Procedures:Ureteroscopy: Visualizes and destroys stones Extracorporeal Shock Wave Lithotripsy (ESWL): procedure uses shock waves to break stones into smaller pieces Endourologic Removal: Removes or breaks down stones using percutaneous Chemolysis, stone dissolution using infusions of chemical solutions Used to break up calculus so that client can pass stone with urination. Nephrolithotomy – Incision into the kidney for removal of calculus is done. If the stone does not respond to conservative treatment. To correct anatomic abnormalities in the kidney that affect urine drainage.When the kidney is nonfunctional due to infection or nephrolithotomy – Incision into the kidney for removal of calculus is done. Nephrectomy – Removal of the kidney due to hydronephrosis. Pyelolithotomy – Removal of stones from the kidney pelvis.
Nephrosclerosis
- Hardening of the renal arteries, often due to prolonged hypertension, diabetes, aging, or other factors.
- Risk Factors: African Americans, uncontrolled hypertension, CKD, and diabetic nephropathy increases risk.
- Acute Hypertensive Nephrosclerosis: Caused by prolonged hypertension.
- Benign Nephrosclerosis: Common in older adults, associated with hypertension, atherosclerosis, and diabetes.
- Early Symptoms: Rare, but urine may contain protein and occasional casts.
- Late Symptoms: CKD symptoms, including elevated BUN, creatinine, and mild proteinuria.
- Treatment: Primarily antihypertensive therapy, especially ACE inhibitors.
- Goal: Control blood pressure to prevent further kidney damage and manage symptoms.
Preventing Renal Calculi
- Avoid excess protein intake.
- Limit sodium intake to 3 to 4 g/day.
- Avoid oxalate-containing foods.
- Drink fluids every 1 to 2 hours daily.
- Two glasses of water at bedtime and an additional glass at each nighttime awakening.
- Avoid activities leading to sudden increases in environmental temperatures
- Contact the primary provider at the first sign of a urinary tract infection.
Polycystic Kidney Disease
- Is a genetic disorder characterized by numerous fluid-filled cysts in the kidneys, leading to enlargement and reduced kidney function.
- Types of PKD: Autosomal Dominant PKD (ADPKD), and Autosomal Recessive PKD (ARPKD):
- Genetic Cause: ADPKD is the most common inherited cause of kidney failure.
- Symptoms: Hematuria, hypertension, kidney stones, UTIs, proteinuria, abdominal fullness, and flank pain as cysts grow.
- Family History: Important for diagnosis.
- Physical Exam: Abdominal palpation often reveals enlarged cystic kidneys.
- Tolvaptan slows kidney function decline
- Supportive Care: Manage blood pressure, provide pain relief, and treat infections.
- End stage requires renal replacement therapy and Genetic Counseling.
Hydronephrosis
- Is Abnormal dilation of renal pelvis and calyces.
- Causes: Congenital urethral obstruction, cancer cervix, bladder cancer,BPH,prostatic cancer.
- Manifestations: (colicky flank pain, hematuria, pyuria, fever, nausea and vomiting, abdominal pain. Chronic: intermittent dull flank pain, hematuria, pyuria, fever, palpable mass.
- Diagnosis: Ultrasound, CT scan, Cystoscopy
- Treatment should center around stents, monitor lntake and Output, and Irrigate tubes as ordered
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.