Podcast
Questions and Answers
Which function is NOT a primary function of the gastrointestinal (GI) system?
Which function is NOT a primary function of the gastrointestinal (GI) system?
- Absorption of nutrients into the bloodstream
- Regulation of body temperature through metabolic processes (correct)
- Digestion of food into absorbable nutrients
- Elimination of undigested waste products
When assessing a patient with gastrointestinal (GI) complaints, which aspect of their history is most useful in guiding further diagnostic tests?
When assessing a patient with gastrointestinal (GI) complaints, which aspect of their history is most useful in guiding further diagnostic tests?
- Frequency of social gatherings attended by the patient
- Details of the patient's symptoms, including onset and duration (correct)
- Brand of over-the-counter medications the patient uses
- Patient's preferred type of cuisine
A nurse is preparing a patient for a diagnostic test to identify structural abnormalities in the esophagus. Which pre-procedural instruction is MOST important for the nurse to provide?
A nurse is preparing a patient for a diagnostic test to identify structural abnormalities in the esophagus. Which pre-procedural instruction is MOST important for the nurse to provide?
- Refrain from smoking before the procedure (correct)
- Consume a large meal the night before to stimulate bowel activity
- Administer an antihistamine to prevent allergic reaction
- Maintain a high-fiber diet in the days leading up to the test
In a diagnostic setting, what is the primary purpose of using radiopaque contrast media during fluoroscopy?
In a diagnostic setting, what is the primary purpose of using radiopaque contrast media during fluoroscopy?
Following an esophagogastroduodenoscopy (EGD), a patient is drowsy. Which nursing intervention is MOST critical to implement FIRST?
Following an esophagogastroduodenoscopy (EGD), a patient is drowsy. Which nursing intervention is MOST critical to implement FIRST?
After a barium swallow test, a patient is instructed to drink fluids liberally. Why is this instruction given?
After a barium swallow test, a patient is instructed to drink fluids liberally. Why is this instruction given?
A patient who has undergone a gastrostomy is at risk for metabolic alkalosis due to gastric decompression via a nasogastric tube (NGT). What electrolyte imbalance is most commonly associated with metabolic alkalosis in this setting?
A patient who has undergone a gastrostomy is at risk for metabolic alkalosis due to gastric decompression via a nasogastric tube (NGT). What electrolyte imbalance is most commonly associated with metabolic alkalosis in this setting?
Which nursing intervention is MOST important when caring for a patient with a nasogastric tube (NGT) for continuous feeding?
Which nursing intervention is MOST important when caring for a patient with a nasogastric tube (NGT) for continuous feeding?
What is the MOST significant concern when administering medications via the enteral route through a nasogastric, gastrostomy, or jejunostomy tube?
What is the MOST significant concern when administering medications via the enteral route through a nasogastric, gastrostomy, or jejunostomy tube?
Which strategy is MOST appropriate for minimizing the risk of aspiration pneumonia in a patient receiving intermittent bolus feedings through a gastrostomy tube:
Which strategy is MOST appropriate for minimizing the risk of aspiration pneumonia in a patient receiving intermittent bolus feedings through a gastrostomy tube:
A patient reports experiencing frequent heartburn, regurgitation, and epigastric pain, especially after meals. Which condition is MOST likely responsible for these symptoms:
A patient reports experiencing frequent heartburn, regurgitation, and epigastric pain, especially after meals. Which condition is MOST likely responsible for these symptoms:
A patient is diagnosed with GERD. Which lifestyle modification is MOST beneficial in managing this condition?
A patient is diagnosed with GERD. Which lifestyle modification is MOST beneficial in managing this condition?
A patient with GERD is prescribed a proton pump inhibitor (PPI). What is the PRIMARY mechanism of action of this medication?
A patient with GERD is prescribed a proton pump inhibitor (PPI). What is the PRIMARY mechanism of action of this medication?
Which dietary modification is MOST appropriate for a patient experiencing frequent GERD symptoms?
Which dietary modification is MOST appropriate for a patient experiencing frequent GERD symptoms?
A patient is diagnosed with a hiatal hernia. What is the primary anatomical abnormality associated with this condition?
A patient is diagnosed with a hiatal hernia. What is the primary anatomical abnormality associated with this condition?
Which symptom is MOST indicative of a hiatal hernia:
Which symptom is MOST indicative of a hiatal hernia:
A patient with a hiatal hernia reports experiencing nocturnal heartburn. Which intervention is MOST appropriate to recommend?
A patient with a hiatal hernia reports experiencing nocturnal heartburn. Which intervention is MOST appropriate to recommend?
What advice should a nurse give to a patient with a hiatal hernia to minimize symptoms?
What advice should a nurse give to a patient with a hiatal hernia to minimize symptoms?
A patient is diagnosed with gastritis. What is the PRIMARY pathophysiological process underlying this condition?
A patient is diagnosed with gastritis. What is the PRIMARY pathophysiological process underlying this condition?
What dietary modification is generally recommended for a patient with gastritis?
What dietary modification is generally recommended for a patient with gastritis?
A patient with gastritis is prescribed an antacid medication. What is the PRIMARY mechanism of action of antacids in treating gastritis?
A patient with gastritis is prescribed an antacid medication. What is the PRIMARY mechanism of action of antacids in treating gastritis?
A patient is diagnosed with a peptic ulcer. What is the MOST common cause of peptic ulcers?
A patient is diagnosed with a peptic ulcer. What is the MOST common cause of peptic ulcers?
A patient with a peptic ulcer reports experiencing pain that is relieved by eating. Which type of ulcer is MOST likely responsible for this symptom?
A patient with a peptic ulcer reports experiencing pain that is relieved by eating. Which type of ulcer is MOST likely responsible for this symptom?
A patient with a peptic ulcer is prescribed sucralfate (Carafate). What instruction is MOST important for the nurse to provide regarding the administration of this medication?
A patient with a peptic ulcer is prescribed sucralfate (Carafate). What instruction is MOST important for the nurse to provide regarding the administration of this medication?
Several diagnostic tests can be performed for GI deviations. Which of the following represents a common test for detecting H. pylori?
Several diagnostic tests can be performed for GI deviations. Which of the following represents a common test for detecting H. pylori?
Which nursing intervention is essential for a patient undergoing a gastrectomy to prevent potential respiratory complications?
Which nursing intervention is essential for a patient undergoing a gastrectomy to prevent potential respiratory complications?
Following a total gastrectomy, a patient may develop pernicious anemia due to the lack of intrinsic factor production. What is the PRIMARY treatment for this complication?
Following a total gastrectomy, a patient may develop pernicious anemia due to the lack of intrinsic factor production. What is the PRIMARY treatment for this complication?
A patient is admitted with gastroenteritis and severe dehydration. What is the PRIMARY goal of nursing care?
A patient is admitted with gastroenteritis and severe dehydration. What is the PRIMARY goal of nursing care?
A patient is diagnosed with Clostridium difficile (C. difficile) infection. What is the MOST appropriate infection control measure to prevent the spread of this organism?
A patient is diagnosed with Clostridium difficile (C. difficile) infection. What is the MOST appropriate infection control measure to prevent the spread of this organism?
A patient is prescribed antibiotics for C. difficile infection. What should the nurse include in the patient education?
A patient is prescribed antibiotics for C. difficile infection. What should the nurse include in the patient education?
A patient is scheduled for a colonoscopy. Which instruction should the nurse include in the pre-procedure teaching?
A patient is scheduled for a colonoscopy. Which instruction should the nurse include in the pre-procedure teaching?
A nurse is reviewing a patient's medication list and notices the patient is taking long-term NSAIDs. The nurse should assess the patient for which potential gastrointestinal complication?
A nurse is reviewing a patient's medication list and notices the patient is taking long-term NSAIDs. The nurse should assess the patient for which potential gastrointestinal complication?
A patient is prescribed total parenteral nutrition (TPN). What is the BEST way to describe it?
A patient is prescribed total parenteral nutrition (TPN). What is the BEST way to describe it?
A patient with hiatal hernia has a history of GERD. What intervention will assist this patient?
A patient with hiatal hernia has a history of GERD. What intervention will assist this patient?
Flashcards
Gastrointestinal (GI) system
Gastrointestinal (GI) system
The gastrointestinal (GI) system is responsible for digestion and absorption of nutrients, extending from the mouth to the anus, and includes accessory organs like the liver, gallbladder, and pancreas.
Ingestion
Ingestion
The act of taking food and liquid into the body.
Digestion
Digestion
The process of breaking down food into absorbable nutrients.
Absorption
Absorption
Signup and view all the flashcards
Elimination
Elimination
Signup and view all the flashcards
Radiographic Studies
Radiographic Studies
Signup and view all the flashcards
Small Bowel Series
Small Bowel Series
Signup and view all the flashcards
Barium Swallow
Barium Swallow
Signup and view all the flashcards
Ultrasonography
Ultrasonography
Signup and view all the flashcards
Gastrointestinal Endoscopy
Gastrointestinal Endoscopy
Signup and view all the flashcards
Laboratory Tests
Laboratory Tests
Signup and view all the flashcards
NGT decompression
NGT decompression
Signup and view all the flashcards
Nasogastric Tube (NGT) Insertion
Nasogastric Tube (NGT) Insertion
Signup and view all the flashcards
GERD
GERD
Signup and view all the flashcards
GERD dietary changes
GERD dietary changes
Signup and view all the flashcards
GERD Lifestyle changes
GERD Lifestyle changes
Signup and view all the flashcards
Hiatal hernia
Hiatal hernia
Signup and view all the flashcards
axial or sliding hernia
axial or sliding hernia
Signup and view all the flashcards
paraesophageal hernia
paraesophageal hernia
Signup and view all the flashcards
Hiatel Hernia Dieatry changes
Hiatel Hernia Dieatry changes
Signup and view all the flashcards
Hiatel Hernia lifestyle changes
Hiatel Hernia lifestyle changes
Signup and view all the flashcards
Hiatal Hernia Dietary changes
Hiatal Hernia Dietary changes
Signup and view all the flashcards
Gastritis
Gastritis
Signup and view all the flashcards
Gastritis Signs and treatment
Gastritis Signs and treatment
Signup and view all the flashcards
Peptic Ulcer Disease (PUD)
Peptic Ulcer Disease (PUD)
Signup and view all the flashcards
Peptic ulcer signs
Peptic ulcer signs
Signup and view all the flashcards
Peptic Ulcer medicatons
Peptic Ulcer medicatons
Signup and view all the flashcards
Study Notes
- Upper Gastrointestinal System: Structure, Function, & Clinical Considerations
Theory Objectives
- Explore the anatomy and physiology of the gastrointestinal system
- Understand the impact of age and culture on gastrointestinal function
- Learn about diagnostic tests and procedures for gastrointestinal deviations
- Identify nursing considerations for nasogastric tube (NGT) insertion, care, maintenance, and patency
- Discuss nursing considerations for enteral nutrition and medication administration via NGT/GT/JT, including complications and safety precautions
- Differentiate between total parenteral nutrition (TPN) and peripheral parenteral nutrition (PPN)
- Recognize risk factors for oral and esophageal cancer
- Explain hiatal hernia, including causes, symptoms and treatment
- Describe gastritis and gastroesophageal reflux disease (GERD)
- Identify risk factors associated with GERD
- Explain the etiology, pathophysiology, medications, and diet considerations for peptic ulcer disease (PUD)
- Discuss risk factors associated with gastric cancer
- Discuss gastric procedures like total gastrectomy, including possible complications like hemorrhage, dumping syndrome, and nutritional issues
- Discuss bariatric surgery and its potential complications
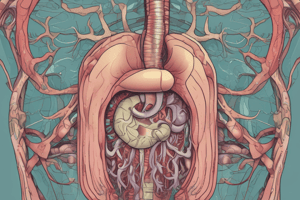
Introduction to the Gastrointestinal System
- The gastrointestinal (GI) system is responsible for the digestion and absorption of nutrients
- Extends from the mouth to the anus
- Includes accessory organs like the liver, gallbladder, and pancreas
Functions of the GI System
- Ingestion: Taking in food and liquid.
- Digestion: Breaking down food into absorbable nutrients.
- Absorption: Uptake of nutrients into the bloodstream.
- Elimination: Removal of undigested waste.
Assessment
- History: Includes chief complaint, length of symptoms, and details
- Nutrition: Assesses ability to eat, type of diet, and tolerance of foods
- Stools: Evaluates characteristics and presence of occult blood using a Guaiac test
- Medications/Herbs/Rx: Review of current medications, herbs, and prescriptions
- Weight: Notes any recent gain or loss
- Medical and Surgical History: Includes information about past medical conditions and surgeries
- Family History: Explores any relevant family medical history
- Allergies: Identifies any known allergies
- Physical Examination: Includes general appearance, skin assessment, mouth examination, abdominal assessment, and anus examination when appropriate
Abdominal Assessment
- Inspection: Visual examination of the abdomen.
- Auscultation: Listening to bowel sounds.
- Percussion: Tapping on the abdomen to assess underlying structures.
- Palpation: Feeling the abdomen to detect tenderness or abnormalities.
Four Quadrants of the Stomach
- Right Upper Quadrant (RUQ): Contains the gallbladder, duodenum, right lobe of the liver, head of the pancreas, right adrenal gland, part of the right kidney, and portions of the ascending and transverse colon
- Left Upper Quadrant (LUQ): Contains the spleen, stomach, body of the pancreas, left lobe of the liver, left adrenal gland, part of the left kidney, and portions of the transverse and descending colon
- Right Lower Quadrant (RLQ): Contains the appendix, cecum, portion of the ascending colon, right ovary, right ureter, right spermatic cord, and lower portion of the kidney
- Left Lower Quadrant (LLQ): Contains the sigmoid colon, portion of the descending colon, left ovary, left ureter, left spermatic cord, and lower portion of the kidney
Diagnostic Tests
- Radiographic Studies:
- Radiopaque contrast media is used with fluoroscopy.
- They help identify the location and structural appearance of organs in the abdomen, chest, or GI system.
- Small Bowel Series:
- Involves fluoroscopy of the small intestine to the lower part.
- It helps to identify obstructions in the jejunum or ileum, tumors, and inflammation.
- Uses more barium and typically takes 5-6 hours.
- Barium Swallow or Upper Gastrointestinal Series:
- Fluoroscopic observation to observe swallowing of barium from the esophagus to the stomach and the beginning of the small intestines.
- It helps identify structural abnormalities in the esophagus, swallowing discoordination, and oral aspiration
- Pre-procedural requisites include: Low-residue diet, Laxative, Smoking
- Post-procedural requisites include: Drink fluids liberally; Obtain stool specimens; Laxative; Obtain stool specimens after barium has passed
- Ultrasonography:
- High-frequency sound waves are used to determine the size and location of organs.
- Outlines structures, abnormalities, cholelithiasis, and pyloric stenosis changes; Appendicitis changes
- Gastrointestinal Endoscopy (EGD - esophagogastroduodenoscopy):
- Visual examination of the lumen of the GI tract using a flexible fiberoptic endoscope.
- Evaluates the appearance and integrity of the GI mucosa and aids in detecting lesions
- Priority Post care includes gag reflex, monitor for bleeding, fever, abdominal distention, and vomiting
- NPO before procedure, use of a local anesthetic, and anxiolytic are needed.
- Laboratory Tests: Includes complete blood count, urinalysis, serum bilirubin, cholesterol, serum ammonia level, prothrombin time, protein electrophoresis, enzymes, common tumor marker blood studies, gastric analysis (H. pylori test), hydrogen breath testing, and stool analysis
Gastrostomy Tubes
- Provides Route: Nutrition, Medications, Gastric decompression, Lavage, Treatment
- Placement: Nasogastric (NG), Orogastric, Surgical placement (Gastrostomy, PEG tube, Jejunostomy)
- Long-term Tube Feedings: partial parenteral nutrition (PPN), total parenteral nutrition (TPN)
- A nasogastric tube (NGT) decompression can lead to metabolic alkalosis, often associated with hypokalemia
Nasogastric Tube (NGT) Insertion
- Used for feeding, medication administration, or gastric decompression
- Nursing concerns: proper placement, patient comfort, prevention of complications
NGT Care and Maintenance
- Regular checks for proper placement.
- Flushing the tube to maintain patency
- Monitoring for signs of irritation or infection.
Esophageal Disorders: GERD
- Etiology: Gastroesophageal Reflux Disease (GERD)
- Gastric contents regurgitates into the esophagus
- Cause: Lower Esophagus Sphincter (LES) insufficiently closes Risk factors: Pregnancy, obesity, hiatal hernia Assessment Findings: Signs and Symptoms - Epigastric pain (dyspepsia), Burning (pyrosis), Regurgitation, Dysphagia, and Esophagitis
- Dietary Changes: Avoid meals 2-3 hours before bed and eliminate foods and drinks that can irritate the stomach lining or increase acid production, like OJ, spicy foods, and chocolate
- Lifestyle Changes: Smoking cessation, weight loss (if obese), avoiding constrictive clothing, and stress reduction are recommended
- Patient Positioning: High fowlers after meals and elevate head of bed (HOB) while resting
- Medication education: Use of Ca, aluminum, and Mg based antacids, H2 antagonists, and proton pump inhibitors are used
Hiatal Hernia
- Part of the stomach pushes through the diaphragm, the muscle that separates the chest from the abdomen
- Cause: Congenital, trauma, factors increasing intra-abdominal pressure, straining to pass bowel, persistent cough
- Assessment Findings: GERD symptoms, Heartburn, Belching, pain after eating, Nausea, and Fullness
- Axial (or sliding): Junction of stomach, esophagus slide in and out through weakened portion of diagram
- Paraesophageal: Fundus is displaced upward
- Nursing Interventions: Small frequent meals, Avoid spicy foods, ETOH, caffeine, and smoking; lifestyle changes, decrease weight, and smoking cessation; positioning (elevate HOB 3-4 hours after eating); medication (Antacids); surgery is an option is problematic
Gastric Disorders: Gastritis
- Inflammation of the stomach lining.
- Causes: Intake of irritating foods, caffeine, poisons, duodenal reflux, medications (steroids, aspirin, NSAIDs), lifestyle factors like smoking and ETOH, increased gastric acid production, and Helicobacter pylori
- Signs and Symptoms: Heartburn, epigastric fullness, pressure, pain, anorexia, N & V
- Nursing Management: Diet restriction, track patient's weight, provide electrolyte drinks (ex. Gatorade, pedialyte, IV fluids), and monitor for signs of bleeding
Peptic Ulcer Disease (PUD)
- Source: Sores in the lining of the stomach or small intestine.
- Cause: Infection with Helicobacter pylori (H. pylori); Family history, chronic gastric inflammation, long-term NSAIDs, smoking, stress, ETOН, Imbalance of enzymes, Hyperacidity or chronic reduction in mucous
- Severe Pain ( upper abdomen and back) “burning”
- Assessments Findings: Greater on empty stomach, Relief when eating, Bleeding: Hematemesis, Melena (black tar like stools), Weight loss Medications:
- Antibiotics: Kills H. pylori (Amoxicillin, Flagyl).
- H2 receptors antagonists: Decrease acid secretion (Pepcid, Tagamet).
- Antacids: Neutralize stomach acid (Sucralfate: Carafate, Tums, Rolaids) - Take 1 hour before meals.
- Proton pump inhibitors: Blocks acid production (Prilosec).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Overview of the upper gastrointestinal system, including anatomy, physiology, and clinical considerations. This includes diagnostic tests, nursing considerations for nasogastric tubes, enteral nutrition, and parenteral nutrition. Also covered are risk factors, causes, symptoms and treatment of oral and esophageal cancer, Hiatal hernia, GERD and peptic ulcers.