Podcast
Questions and Answers
What is the primary mechanism behind the formation of urinary tract calculi?
What is the primary mechanism behind the formation of urinary tract calculi?
- Increased fluid intake diluting urine solutes
- Acidic urine pH preventing crystal aggregation
- High concentrations of minerals and salts in the urine that crystallize (correct)
- Decreased concentrations of minerals and salts in the urine
Which dietary factor is least likely to contribute to the formation of kidney stones?
Which dietary factor is least likely to contribute to the formation of kidney stones?
- Excessive salt intake
- High intake of animal protein
- Increased intake of oxalate-rich foods
- Adequate intake of dietary fiber (correct)
What physiological response is often observed in patients experiencing renal colic due to urinary tract calculi?
What physiological response is often observed in patients experiencing renal colic due to urinary tract calculi?
- Decreased blood pressure
- Restless behavior(kidney stone dance) (correct)
- Sedation
- Bradycardia
Which diagnostic study is most appropriate for the initial assessment and diagnosis of urinary tract calculi?
Which diagnostic study is most appropriate for the initial assessment and diagnosis of urinary tract calculi?
Why is it important to strain the urine of a patient with urinary tract calculi?
Why is it important to strain the urine of a patient with urinary tract calculi?
For a patient with calcium stones, which dietary modification is generally recommended?
For a patient with calcium stones, which dietary modification is generally recommended?
What is the purpose of using alpha-adrenergic blockers in the acute management of urinary tract calculi?
What is the purpose of using alpha-adrenergic blockers in the acute management of urinary tract calculi?
Which intervention is typically indicated for urinary tract calculi larger than 5 mm that are causing infection or impaired renal function?
Which intervention is typically indicated for urinary tract calculi larger than 5 mm that are causing infection or impaired renal function?
Following a cystoscopy for the removal of bladder stones, what is an important nursing intervention?
Following a cystoscopy for the removal of bladder stones, what is an important nursing intervention?
Which of the following is a characteristic manifestation of a ureteral stricture?
Which of the following is a characteristic manifestation of a ureteral stricture?
Which diagnostic imaging is MOST appropriate to evaluate the presence of a urethral stricture?
Which diagnostic imaging is MOST appropriate to evaluate the presence of a urethral stricture?
A patient with a ureteral stricture reports increased flank pain after consuming a large volume of fluid. What is the most likely explanation for the increased pain?
A patient with a ureteral stricture reports increased flank pain after consuming a large volume of fluid. What is the most likely explanation for the increased pain?
What is a common initial management approach for ureteral strictures identified during diagnostic imaging?
What is a common initial management approach for ureteral strictures identified during diagnostic imaging?
Which of the following nursing interventions is crucial to monitor in a patient post-urethral dilation?
Which of the following nursing interventions is crucial to monitor in a patient post-urethral dilation?
What is the primary indication for using a urethral catheter?
What is the primary indication for using a urethral catheter?
Which nursing intervention is essential during the insertion of a urethral catheter to minimize the risk of infection?
Which nursing intervention is essential during the insertion of a urethral catheter to minimize the risk of infection?
When are ureteral catheters typically indicated?
When are ureteral catheters typically indicated?
What ongoing assessment is critical for a patient with a ureteral stent?
What ongoing assessment is critical for a patient with a ureteral stent?
What is the primary indication for suprapubic catheter placement?
What is the primary indication for suprapubic catheter placement?
What is a key nursing intervention for managing a suprapubic catheter?
What is a key nursing intervention for managing a suprapubic catheter?
Following the insertion of a nephrostomy tube, what is the most important nursing action?
Following the insertion of a nephrostomy tube, what is the most important nursing action?
Why is patency of greatest concern for patients with a nephrostomy tube?
Why is patency of greatest concern for patients with a nephrostomy tube?
Which of the following is NOT an acceptable reason for catheterization?
Which of the following is NOT an acceptable reason for catheterization?
What is a potential long-term complication associated with chronic indwelling urinary catheters?
What is a potential long-term complication associated with chronic indwelling urinary catheters?
Which of the following nursing actions is MOST important when caring for a patient with an indwelling urinary catheter?
Which of the following nursing actions is MOST important when caring for a patient with an indwelling urinary catheter?
Which post-operative measure is essential following renal surgery to prevent complications such as paralytic ileus?
Which post-operative measure is essential following renal surgery to prevent complications such as paralytic ileus?
A patient following urinary diversion surgery is expected to have mucus in their urine. What is an important nursing action related to this?
A patient following urinary diversion surgery is expected to have mucus in their urine. What is an important nursing action related to this?
What nursing action is essential immediately following a Transurethral Resection of the Prostate (TURP) procedure?
What nursing action is essential immediately following a Transurethral Resection of the Prostate (TURP) procedure?
What is the purpose of continuous bladder irrigation (CBI) after a TURP procedure?
What is the purpose of continuous bladder irrigation (CBI) after a TURP procedure?
Which of the following is the priority nursing intervention for a patient with acute pyelonephritis?
Which of the following is the priority nursing intervention for a patient with acute pyelonephritis?
A patient with acute pyelonephritis is being discharged. Which instruction is most important to include in the discharge teaching?
A patient with acute pyelonephritis is being discharged. Which instruction is most important to include in the discharge teaching?
What finding is a hallmark sign when assessing a patient with acute glomerulonephritis?
What finding is a hallmark sign when assessing a patient with acute glomerulonephritis?
A patient with glomerulonephritis has fluid retention. Which dietary modification is MOST appropriate?
A patient with glomerulonephritis has fluid retention. Which dietary modification is MOST appropriate?
What laboratory finding is expected in a patient with a history of recent streptococcal infection now presenting with acute glomerulonephritis?
What laboratory finding is expected in a patient with a history of recent streptococcal infection now presenting with acute glomerulonephritis?
A child is diagnosed with acute post-streptococcal glomerulonephritis (APSGN). What key information should be included in the teaching plan for the parents?
A child is diagnosed with acute post-streptococcal glomerulonephritis (APSGN). What key information should be included in the teaching plan for the parents?
A patient is diagnosed with Rapidly Progressive Glomerulonephritis (RPGN). What initial sign or symptom is the patient most likely to exhibit?
A patient is diagnosed with Rapidly Progressive Glomerulonephritis (RPGN). What initial sign or symptom is the patient most likely to exhibit?
A patient with nephrosclerosis is receiving antihypertensive medications. What should be the priority nursing action when monitoring this patient?
A patient with nephrosclerosis is receiving antihypertensive medications. What should be the priority nursing action when monitoring this patient?
What is a key characteristic finding in nephrotic syndrome?
What is a key characteristic finding in nephrotic syndrome?
The nurse is caring for a patient with renal artery stenosis. Which assessment finding is most indicative of this condition?
The nurse is caring for a patient with renal artery stenosis. Which assessment finding is most indicative of this condition?
A patient is suspected of having renal vein thrombosis. Which symptom is most closely associated with this condition?
A patient is suspected of having renal vein thrombosis. Which symptom is most closely associated with this condition?
A patient with known renal trauma following a motor vehicle accident is admitted to the hospital. What is the initial diagnostic test to be performed?
A patient with known renal trauma following a motor vehicle accident is admitted to the hospital. What is the initial diagnostic test to be performed?
A child is diagnosed with vesicoureteral reflux. What is a common sign/symptom?
A child is diagnosed with vesicoureteral reflux. What is a common sign/symptom?
A child presents with a painless abdominal mass, hematuria, and hypertension. Which condition is most suspected?
A child presents with a painless abdominal mass, hematuria, and hypertension. Which condition is most suspected?
Flashcards
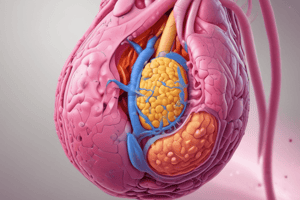
Urinary Tract Calculi Definition
Urinary Tract Calculi Definition
Hard deposits of minerals and salts that form out of the filtrate produced by the nephron.
Urinary Tract Calculi Etiology
Urinary Tract Calculi Etiology
High concentrations of minerals and salts in the urine which crystallize and form stones due to dehydration, diet, genetics, or predisposition.
Climate Risk Factor
Climate Risk Factor
Warm climates increase fluid loss, lower urine volume, and elevate urine solute concentration, increasing stone risk.
Diet Risk Factor
Diet Risk Factor
Signup and view all the flashcards
Genetic Risk Factor
Genetic Risk Factor
Signup and view all the flashcards
Lifestyle Risk Factor
Lifestyle Risk Factor
Signup and view all the flashcards
Metabolic Risk Factor
Metabolic Risk Factor
Signup and view all the flashcards
Urinary pH Risk Factor
Urinary pH Risk Factor
Signup and view all the flashcards
Obstruction/Infection Risk
Obstruction/Infection Risk
Signup and view all the flashcards
Pain Manifestation
Pain Manifestation
Signup and view all the flashcards
Nausea and Vomiting
Nausea and Vomiting
Signup and view all the flashcards
Urinary Symptoms
Urinary Symptoms
Signup and view all the flashcards
Shock Symptoms
Shock Symptoms
Signup and view all the flashcards
Infection Symptoms
Infection Symptoms
Signup and view all the flashcards
Physical Activity
Physical Activity
Signup and view all the flashcards
Imaging and Urinalysis
Imaging and Urinalysis
Signup and view all the flashcards
Blood Tests
Blood Tests
Signup and view all the flashcards
24-Hour Urine Test
24-Hour Urine Test
Signup and view all the flashcards
Stone Analysis
Stone Analysis
Signup and view all the flashcards
Fluid Intake Treatment
Fluid Intake Treatment
Signup and view all the flashcards
Diet Modifications
Diet Modifications
Signup and view all the flashcards
Acute Management
Acute Management
Signup and view all the flashcards
Preventive Measures
Preventive Measures
Signup and view all the flashcards
Surgical Intervention
Surgical Intervention
Signup and view all the flashcards
Cystoscopy
Cystoscopy
Signup and view all the flashcards
Ureteroscopy
Ureteroscopy
Signup and view all the flashcards
Nephrolithotomy
Nephrolithotomy
Signup and view all the flashcards
Lithotripsy
Lithotripsy
Signup and view all the flashcards
Urethral Catheters
Urethral Catheters
Signup and view all the flashcards
Ureteral Catheters
Ureteral Catheters
Signup and view all the flashcards
Suprapubic Catheters
Suprapubic Catheters
Signup and view all the flashcards
Pyelonephritis Definition
Pyelonephritis Definition
Signup and view all the flashcards
Pyelonephritis Signs
Pyelonephritis Signs
Signup and view all the flashcards
Pyelonephritis Interventions
Pyelonephritis Interventions
Signup and view all the flashcards
Glomerulonephritis Definition
Glomerulonephritis Definition
Signup and view all the flashcards
Glomerulonephritis Signs
Glomerulonephritis Signs
Signup and view all the flashcards
APSGN Treatment
APSGN Treatment
Signup and view all the flashcards
RPGN Definition
RPGN Definition
Signup and view all the flashcards
RPGN Treatment
RPGN Treatment
Signup and view all the flashcards
Goodpasture Syndrome
Goodpasture Syndrome
Signup and view all the flashcards
Study Notes
Urinary Tract Calculi
- Hard mineral and salt deposits create urinary tract calculi by solidifying out of filtrate produced by the nephron.
- These stones form as a complication of concentrated minerals and salts in urine.
- Dehydration, high-protein diet, excessive salt or sugar intake, and genetic predisposition increase the risk.
- Within the nephron, excess minerals and salts in filtrate crystalize and aggregate to form stones.
Risk Factors for Urinary Tract Calculi
- Higher fluid loss, lower urine volume, and elevated urine solute concentrations are common in warm climates.
- Diets high in foods rich in oxalates, animal protein, and salt, as well as low calcium and fluid intake, increase risk.
- Dehydration has a strong link to developing urinary tract calculi.
- Cystinuria, gout, or renal acidosis, and a family history of stones are genetic factors.
- Immobility, obesity, and a sedentary lifestyle are risk factors
- Abnormal urine pH, excess calcium, oxalate, uric acid, or low citrate levels are metabolic risks.
- High urine pH favors calcium and phosphate stone formation; low pH favors uric acid and cystine stone formation.
- Urinary stasis and infections with urea-splitting bacteria contribute to struvite stone formation.
Clinical Manifestations of of Urinary Tract Calculi
- Excruciating and sharp pain, also called renal colic, occurs in the flank, back, or lower abdomen, with possible radiation to the groin.
- Nausea and vomiting frequently accompany severe pain.
- Dysuria, hematuria, and urinary urgency/frequency are urinary symptoms.
- Mild shock with cool and moist skin is possible shock symptom
- Fever and chills suggest a concurrent urinary tract infection (UTI).
- Restless behavior is observed with patient's sometimes exhibiting what some call the "kidney stone dance."
Diagnostic Studies for Urinary Tract Calculi
- Noncontrast CT scans or ultrasounds are used for diagnosis.
- Urinalysis detects hematuria and crystalluria and measures urine pH.
- Blood tests measure serum calcium, phosphorus, sodium, potassium, bicarbonate, uric acid, BUN, and creatinine levels.
- 24-hour urine tests gauge various solute levels in recurrent stone formers.
- Clinicians analyze stone retrieval to determine the composition and underlying causes; straining urine is important to collect stones.
Nutrition Therapy for Urinary Tract Calculi
- Increase fluid intake to 2-3 L/day to produce at least 2.5 L/day urine output.
- Avoid high-calcium foods such as dairy, beans, fish with bones, dried fruits, and nuts.
- Limit foods rich in oxalates, (dark roughage, spinach, beets, nuts).
- Reduce intake of high-purine foods such as sardines and organ meats.
- Restrict sodium intake to reduce calcium excretion in urine.
Acute and Preventative Management for Urinary Tract Calculi
- Acute: Pain relief is achieved with opioids or NSAIDs; alpha-adrenergic blockers, may be used as well, and obstruction and infections are treated.
- Preventative: Increased hydration, restricted sodium intake, dietary changes, and Rx to alter urine pH or decrease excretion of stone-forming substances.
- Stones sized over 5 mm, causing infection/impaired renal function/severe pain, warrant surgical intervention.
- Surgical options: endourologic procedures, lithotripsy, or open surgery.
Endourologic Procedures and Lithotripsy for Urinary Tract Calculi
- Cystoscopy removes small bladder stones.
- Ureteroscopy removes stones from the renal pelvis and upper urinary tract with the use of a ureteroscope.
- Percutaneous nephrolithotomy removes kidney stones through a nephroscope inserted into the skin.
- Lithotripsy uses laser, shock waves, ultrasound, or electrohydraulic energy to break stone, with possible complications of hemorrhage/infection/obstruction.
Cystoscopy Nursing Interventions
- Definition: Removal of small bladder stones via a cystoscope inserted through the urethra.
- Pre-procedure: Obtain consent, educate client, NPO if necessary and administer pre-medications.
- Post procedure: Monitor for infection, encourage fluids, assess for bleeding, educate on complications and strain urine.
Ureteroscopy Nursing Interventions
- Definition: Removal of stones from renal pelvis and upper urinary tract using a ureteroscope.
- Pre-procedure: Obtain consent, educate client, NPO if necessary and administer pre-medications.
- Post procedure: Monitor urine output, observe for injury/infection, encourage fluids, provide pain management, educate on hydration and complications and strain urine.
Percutaneous Nephrolithotomy Nursing Interventions
- Definition: Removal of kidney stones via a nephroscope inserted through a small incision in the back.
- Pre-procedure: Obtain consent, educate client, ensure NPO if necessary and Administer pre-medications.
- Post procedure: Monitor vital signs and kidney function, assess incision and nephrostomy tube, encourage fluids, provide pain management, educate on tube care and complications and strain urine.
Lithotripsy Nursing Interventions
- Definition: Breaking up stones using laser, shock waves (ESWL), ultrasound, or electrohydraulic energy.
- Pre-procedure: Obtain consent, educate client, ensure NPO if necessary and administer pre-medications.
- Post procedure: Monitor vital signs and for complications, encourage fluids, provide pain management, educate on complications and strain urine.
Key Points for Kidney Stone Treatment
- Monitor input and output.
- Strain all urine.
- Encourage 2-3L of fluid to assist with flushing of particles of stone.
- Use oral analgesics for pain management during and after discharge.
- Avoid ASA (anticoagulants) before and after procedures to reduce bleeding risk.
Ureteral/Urethral Strictures
- Can involve ureteral or urethral strictures
- Causes include: congenital, surgery, radiation, trauma, urethritis, iatrogenic.
- Management can include: stenting, nephrostomy, surgery, dilation, endoscopic and urethroplasty
- Assessment include: diminished urinary stream, straining, sprayed/split stream, postvoid dribbling, incomplete emptying, frequency, nocturia, acute retention.
- Nursing Interventions (pre/post op): Obtain consent, educate, ensure NPO if required, monitor infection, encourage fluids, assess pain and bleeding, catheter care and educate on complications.
Catheterizations - Urethral Catheters
- Indications: Short-term urinary drainage for urinary retention, surgery/critical care monitoring of output and administration of Rx or contrast dye to bladder.
- Types: Foley (most common), and straight catheter (intermittent).
- Nursing interventions: maintain proper hygiene, secure the catheter, maintain a closed system and monitor urine output/signs of infection.
Catheterizations - Ureteral Catheters
- Indications: Diagnostic or therapeutic procedures in the ureter or kidney.
- Types: Double-J stent and ureteral catheter with a pigtail tip.
Catheterizations - Suprapubic Catheters
- Indications: Long-term bladder drainage for chronic urinary retention, spinal cord injury, or urinary incontinence.
- Types: Standard or Button-style catheters.
- Nursing Interventions: clean/dry exit site, secure the catheter, monitor for infections, provide patient education and it can be temporary or long-term
Catheterizations - Nephrotomy Catheters
- Indications: Temporary drainage from renal pelvis post-surgery/injury to kidney.
- Types: Nephrostomy tube (external catheter) and nephroureteral stent.
- Nursing Considerations/Interventions: Ensure aseptic technique, monitor for infection/obstruction, maintain drainage/assess for bleeding, tube monitoring, education, can be temporary/long-term.
- Management for insertion include general or local anesthesia, using abdominal wall, trocar or sutured, with tubing patent and bladder spasms managed with antispasmodics.
- Always to continue catheter care; use skin barrier at insertion site unless contraindicated.
Complications from Catheters
- Complications of long-term use (30+ days) include CAUTI's (most common) and other bladder spasms, periurethral abscess, chronic pyelonephritis, urosepsis, urethral trauma or erosion, fistula or stricture formation, and stones.
- Never use a catheter for a Routine urine specimen, convenience for nurse or patient's family as it increases risk of infection
- Keep the bag below the bladder and off the floor and tubing q2h for kinks and secure tubing for males on the abdomen and legs on females.
- Hang the bag from the bed's frame and not the side rail with peri care done every shift using soap and water and be sure to empty catheter bags every shift.
Catheter Sizing
- Lumen sizing is done with a French catheter scale
- Women = 14° F-16° F
- Men = 14° F-18° F
- Balloon-5-30mL while tissue erosion can occur catheter too large. Bigger catheter number = larger it is.
Renal and Ureteral Surgery
- Nephrectomy Indications: Renal tumor, bleeding or infected polycystic kidneys, massive trauma, donor transplant.
- Surgical procedures: open or laparoscopic (3 to 5 sites)
- Surgery to ureters/kidneys removes obstruction/congenital abnormalities of fluid diversion.
Post-operative Care for Renal and Ureteral Surgery
- Ensure adequate fluids with normal electrolytes, pain management and potential positioning discomfort and monitor urine output for output with daily weights.
- Monitor: color, consistency and cath patency
- Watch: urine output and respiratory status
- Encourage: Turning, Coughing, incentive and frequent ambulation
- Monitor: abdominal distention and progress diet.
- Interventions: analgesia
Types of Urinary Diversions
- Blocked urine flow by bladder cancer/neurogenic bladder will determine surgical procedures
- Diversion to skin: use of appliance (mostly ileal but no valve/no voluntary control)
- Intraabdominal Reservoir: catheterizable internal pouch (reconstructed from ileum and low pressure)
- Neobladder Reconstruction: New bladder in correct place through surgical intervention; ureters and urethra sutured, with distal part of ileum to neobladder and excreted through urethra.
- Other Management: Avoid distention/paralytic lyeus with NPO and IV hydration and ambulation
Candidates for Neobladder Reconstruction must have:
- Normal: renal function
- Have a: life expectancy of 1-2 years, adequate motor skills and not obese
- Normal health: not have inflammatory digestive health or colon cancer
Postoperative Management for Urinary Diversions
- Prevent: complications
- Maintain: stoma injury and output
- Care: avoid alkaline and prevent skin breakdown
- Monitor bowel obstruction with NPO and hydration, prevent skin injuries.
Interventions for Urinary Diversions
- Teach catheterization, avoid alkaline conditions/dermatitis with post-maintenance and monitoring for frequent emptying.
- Support concerns about personal and sexual recreation.
- Early ambulation with patient NPO and strict PO.
TURP - Transurethral Resection of Prostate
- Used to treat urinary problems caused by an enlarged prostate (BPH) and primarily aims to relieve symptoms.
- These include; difficulty urinating, weak stream, frequent urination (especially at night, nocturia, as well as urgency and retention that may occur.
- CBI (continuous bladder irrigation) can be used to break clots but must STRICTLY monitor fluids ad monitor patients with BPH.
Immediate Post-Operative Care for TURP
- Monitor vitals frequently with assess pain and monitor the I&Os, as well as irrigating and catheter caring appropriately.
Continuous Bladder Irrigation (CBI) Post-Operative for TURP Indications
- Purpose: Prevents clots leading to urinary retention
- Ensures: patency to allow urine drainage
- Reduces post-operative complications and is completed with sterile solution/3 way catheter and is set up on the IV pole.
Acute Pyelonephritis
- Characterized by : a sudden, severe kidney infection often a bacterial infection.
- Infection happens, when pathogens infiltrate renal parenchyma and form abscesses. Pathogens mostly ascending from lower tract (E. coli).
- Nursing Considerations include catheter changes, as they increase rick from lone-term facilities.
Indications of Acute Pyelonephritis
- Present in patient with feverish symptoms, chills. Also note hall mark is for flank pain and to perform CVA (costovertebral angles) for tenderness.
- Dx with urine tests or imaging.
- Treat the infections with IV and other Rxs..
- RNs: Monitor urine and teach and be with patient when necessary.
Acute Glomerulonephritis
- An inflammatory condition of renal glomeruli, causing impaired kidney function
- Aetiology: frequently follows streptococcal infections, in rare cases caused by autoimmune irregularities.
- Hematuria, characterized by tea-coloured urine, Hypertension and edema are frequently observed conditions.
Acute Post-Streptococcal Glomerulonephritis (Pediatrics)
- An inflammation after kidney with previous hx of sore throat/ skin infections.
- Patients report abdominal pain at the CVA scoring higher, pulmonary also with crackles is frequent as well.
- Hallmarks: hematuria and may need low protein diet.
Goodpasture Syndrome
- Autoimmune diseases which attack the bodies own basement membranes and causes shortness of breath, lung or kidney hemorrhage and fatigue.
- Dx: is based off presence of these autoantibodies and treat by improving O2 delivery of immunosuppressive and plasmapheresis Rx's
- Hallmark: can check creatinine or hypertension in kids.
- RNs: Monitor fluids and VS.
Renal Trauma
- Trauma from an injury/falling on that the patient may first indicate internal bleeding and or shock symptoms
- Can lead to other injury (internal/urine leak/kidney failure)
- Can tx for pain, but make sure monitor patients
Acute Kidney Injury (AKI)
- With impaired blood flow (direct/low) they have build up leading to more renal problems.
- Low BP: leads to AKI.
- Tx supportively while monitor.
Types of Dialysis
- Hemodialysis takes blood into a machine while CRRT (Continuous Renal Replacement Therapy, is required with unstable patients and is used slower more gradual treatment to wean off blood.
- CVC (central venous catheters)
- Dialysis interventions for patients need regular check and monitoring.
Complications stemming from Dialysis
- Care related to this is vital for the prevention of all infection to improve QOL.
- Prevent with asepsis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.